The Establishment of a New Air Health Index Integrating the Mortality Risks Due to Ambient Air Pollution and Non-Optimum Temperature
Qingli Zhng, Renjie Chen, Gunjin Yin, Xiho Du, Xi Meng,b, Yng Qiu, Hidong Kn,d,*,Migeng Zhou*
aKeyLaboratory of Public HealthSafety,MinistryofEducation, School of PublicHealth,FudanUniversity, Shanghai200032,China
b Shanghai Key Laboratory ofMeteorology and Health, Shanghai Meteorological Service&Shanghai TyphoonInstitute,ChinaMeteorological Administration,Shanghai 200030,China
c Department of Environmental Sciences and Engineering, College of Architecture andEnvironmentalSciences, Sichuan University, Chengdu 610065,China
dChildren’sHospital of FudanUniversity&NationalChildren’s Medical Center, Shanghai 200032, China
eNational Centerfor ChronicandNoncommunicableDiseaseControland Prevention,ChineseCenterforDisease ControlandPrevention, Beijing100050, China
Keywords:Air pollution Temperature Air Health Index Mortality Time-series Risk communication
ABSTRACT A composite Air Health Index (AHI) is helpful for separately emphasizing the health risks of multiple stimuli and communicating the overall risks of an adverse atmospheric environment to the public. We aimed to establish a new AHI by integrating daily mortality risks due to air pollution with those due to non-optimum temperature in China.Based on the exposure-response(E-R)coefficients obtained from time-series models,the new AHI was constructed as the sum of excess mortality risk associated with air pollutants and non-optimum temperature in 272 Chinese cities from 2013 to 2015. We examined the association between the‘‘total AHI”(based on total mortality)and total mortality,and further compared the ability of the ‘‘total AHI” to predict specific cardiopulmonary mortality with that of ‘‘specific AHIs”(based on specific mortalities).On average,air pollution and non-optimum temperature were associated with 28.23% of daily excess mortality, of which 23.47% was associated with non-optimum temperature while the remainder was associated with fine particulate matter (PM2.5) (1.12%), NO2 (2.29%,), and O3(2.29%). The new AHI uses a 10-point scale and shows an average across all 272 cities of 6 points. The E-R curve for AHI and mortality is approximately linear, without any thresholds. Each one unit increase in‘‘total AHI”is associated with a 0.84%increase in all-cause mortality and 1.01%,0.98%,1.02%,1.66%,and 1.71% increases in cardiovascular disease, coronary heart disease, stroke, respiratory diseases, and chronic obstructive pulmonary disease mortality, respectively. Cause-specific mortality risk estimates using the‘‘total AHI”are similar to those predicted by‘‘specific AHIs.”In conclusion,the‘‘total AHI”proposed herein could be a promising tool for communicating health risks related to exposure to the ambient environment to the public.
1. Introduction
Both ambient air pollution and non-optimum temperature have been found to be associated with increased mortality risk due to cardiovascular disease (CVD) and respiratory diseases [1,2]. It was estimated that air pollution caused 1.85 million deaths and 42.51 million disability-adjusted life years in China in 2019 [3].In an effort to reduce the disease burden associated with air pollution,the Air Quality Index(AQI)was developed to inform the public about air pollution levels and the health risks of exposure.However,the current AQI is solely determined by the air pollutant with the highest pollutant-specific AQI score, while the combined health effects of simultaneous exposure to multiple air pollutants are not considered.
In the context of global climate change, non-optimum ambient temperature has been recognized as a global health challenge,especially in developing regions. It has been estimated that 14.33% of non-accidental mortality is attributable to non-optimum ambient temperature in China [2]. Indices that are currently used to indicate health risks due to the ambient temperature, such as the heat-/cold-wave index, only consider extreme temperature [4,5], while the much greater health risk attributed to moderate non-optimum temperature is not addressed. Thus, the heat-/cold-wave index may substantially underestimate the disease burden attributed to non-optimum temperature. In addition, the heat-/cold-wave index is defined based on daily temperature changes and does not consider the relationship between ambient temperature and population health.
In reality, exposure to ambient air pollution and temperature occurs simultaneously. Moreover, these environmental factors share similar biological pathways in inducing acute adverse health effects,such as changes in inflammation,oxidative stress,thermogenesis,and autonomic nervous function[6,7].Therefore,communicating the health risks from both air pollution and temperature is crucial in protecting the susceptible population. However, to the best of our knowledge, no indices have considered the combined health risk from non-optimum temperature and air pollution. It is therefore necessary to establish a new Air Health Index (AHI)integrating the health risks of ambient air pollution and nonoptimum temperature, both individually and overall, in order to better inform the public of the overall health risk of exposure to these ambient environmental factors and to help effectively reduce exposure and mitigate potential harm.
Using a nationwide database, we aimed to establish a new AHI by integrating the mortality risks due to ambient air pollution and non-optimum temperature and to evaluate the association between AHI and daily mortality in China.The new AHI would also provide the daily excess deaths due to each risk factor. Furthermore, we would compare the predictive ability of the ‘‘total AHI”based on total mortality with that of the ‘‘specific AHI” based on specific mortality in order to evaluate the necessity of developing separate AHIs for specific diseases.
2. Materials and methods
2.1. Data sources
The nationwide analysis was based on daily mortality,air pollutants levels, and weather conditions in 272 Chinese cities from 1 January 2013 to 31 December 2015. Details of this dataset have been described previously [8-10]. In brief, these cities are located in all 31 provincial administrative regions and cover more than 20% (almost 290 million) of the total population in the mainland of China. Daily mortality counts in these cities, including allcause and cause-specific mortality, were obtained from the China Disease Surveillance Points system,which has been shown to have good representativeness at the national and provincial levels[11,12].
We selected fine particulate matter(PM2.5),NO2,and O3as representative air pollutants for this study, as they were shown to have significant and stable associations with mortality in our previous studies in the same database[8,10,13].Daily average concentrations of PM2.5, NO2, and the maximum 8 h mean concentration of O3were collected from the National Urban Air Quality Real-Time Publishing Platform†† http://106.37.208.233:20035/.‡ http://data.cma.cn/.. This platform had a total of 1265 monitors,with a median of four monitors (range 1-7) in each city by 2015.Daily air pollution levels in each city were then calculated as the mean across all valid monitors in these cities. The daily mean temperature and mean relative humidity in each city were derived from the China Meteorological Data-Sharing Service System‡† http://106.37.208.233:20035/.‡ http://data.cma.cn/.. The study protocol was approved by the Institutional Review Board at School of Public Health, Fudan University (No. 2014-07-0523).
2.2. Data analysis
We started by obtaining the associations of daily air pollution and temperature with all-cause and cause-specific mortality using time-series analyses. Then, we calculated the daily excess mortality risk for these ambient risk factors. Finally, we obtained the national AHIs by dividing the daily excess mortality risk by the maximum weighted-average excess mortality risk and multiplying by 10.
2.2.1. Time-series analysis
First,we excluded days when the ambient air pollution or temperature was below the 2.5th percentile or above the 97.5th percentile in order to reduce the influence of extreme values. We then used standard time-series analyses to obtain regression coefficients for the daily mortality per unit (1 μg·m-3) change in daily PM2.5, NO2, and O3. Details of the analytic protocols have been described in our previous studies [2,10,13]. As air pollutant concentrations differ in warm and cold seasons, we obtained relative risk (RR) estimates for air pollutants in the warm (May-October)and cold (November-April) seasons for use in subsequent steps.Covariates included a natural cubic spline smooth function of the calendar day with 7 degrees of freedom(DoF)per year,an indicator variable for ‘‘day of the week,” and natural smooth functions for mean temperature and relative humanity on the concurrent day with 6 and 3 DoF, respectively [14].
For temperature,we used the 21-day moving average temperature,as considered in our previous work,and adopted the temperature that was estimated to have the lowest all-cause mortality risk(i.e.,22.8°C)as the optimum temperature[2].In our previous study, the exposure-response (E-R) curve for temperature and mortality exhibited an inverted-J shape with an approximately linear increase in mortality risk with non-optimum temperature [2].Therefore, we assumed a piecewise linear function divided by the optimum temperature for the association between temperature and mortality. According to the RRs for extreme low (RR = 1.68)and extreme high (RR = 1.16) temperature estimated in the previous study, we calculated the coefficients for the increase in daily mortality per unit (1 °C) change in temperature as follows:
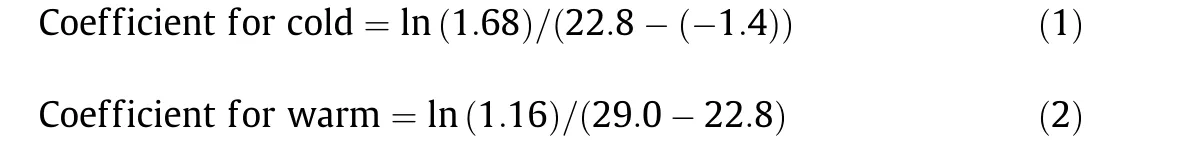
where 1.68 and 1.16 are the RRs of daily total mortality associated with extreme low and extreme high temperature,respectively;22.8 is the optimum temperature for total mortality; and -1.4 and 29.0 are the averages of the extreme low and extreme high temperatures, respectively.
2.2.2. Constructing the national AHI
We used the RRs estimated for PM2.5and NO2on the concurrent day (lag 0 day) and that for O3on lag 2 day in this step because these lag days were shown to have the largest effect estimates[14].First,we calculated the daily excess mortality risk for air pollution (with 0 as the reference) and temperature (with 22.8 °C as the reference) in each city using Eq. (3):

where ERitis the percentage of excess mortality associated with the risk factor i(air pollutants or temperature)on day t;βiis the regression coefficient indicating the increase in daily mortality per unit change (1 μg·m-3for air pollutants; 1 °C for temperature) of risk factor i; Δxitis the difference between risk factor i on day t and the reference level(0 for air pollutants and 22.8°C for temperature).The daily excess mortality risk is the sum of the excess mortality risks of all risk factors. Calculations were conducted only for days when data were available for all risk factors.
Next,we introduced the weighted-average excess mortality risk to reduce the influence of overweighting small cities with high pollution levels or extreme temperatures.To be specific,we extracted the maximum value of the daily percentage of excess mortality in each city for warm and cold temperature, separately. Then, we averaged the maximum value across all cities for each day and weighted it by the average counts of daily deaths in each city during the warm and cold periods, separately. The weighted-average excess mortality risk was calculated separately for cold and warm temperature, as follows:
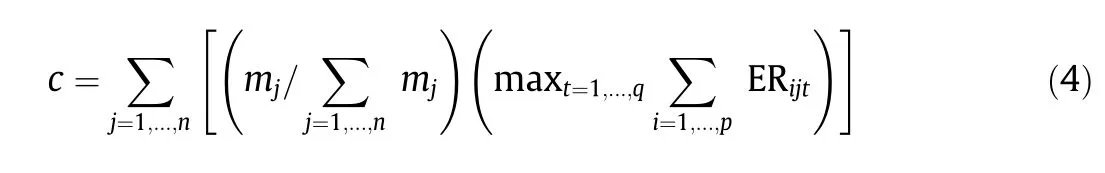
where c is the maximum weighted-average excess mortality as a percentage in the 272 cities during the study period for cold or for warm temperature; mjdenotes the daily average death count in the jth city; and ERijtis the percentage of excess mortality for the ith risk factor on the tth day in the jth city.
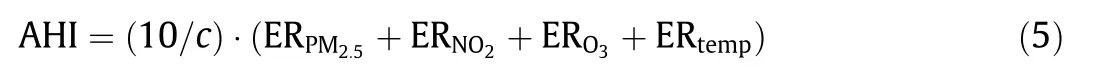
Finally, the national AHIs in cold and warm temperature were obtained by dividing the daily percentage of excess mortality by the maximum weighted-average percentage of excess mortality and multiplying by 10. The formula is provided in Eq. (5):
This procedure produced a series of daily AHI values during the study period scaling from 0 to 10+. A value greater than 10 indicates that the excess mortality risk related to air pollution and temperature on this particular day is greater than the maximum weighted-average excess mortality (i.e., c) as observed in the current database. For simplicity of communication, AHI values were rounded to the nearest integer.
2.2.3. Performance evaluation
We evaluated the performance of the AHI in predicting mortality by estimating the associations of the AHI with the daily total and cause-specific mortality on lag 0 day in 272 Chinese cities from 2013 to 2015. In addition, we plotted the E-R curves for AHI and mortality at the national level using an approach described elsewhere [15]. For possible nonlinear relationships, we used a Bspline function for the AHI with two knots at the 25th and 75th percentiles.
In this evaluation, we built an AHI based on total mortality(‘‘total AHI”)and on cause-specific mortality, including CVD, coronary heart disease (CHD), stroke, respiratory disease, and chronic obstructive pulmonary disease(COPD)(‘‘specific AHI”).We further evaluated the performance of the ‘‘total AHI” in predicting causespecific mortality risks by comparing coefficient estimates and model fit statistics(R2and Akaike Information Criterion(AIC))with cause-specific mortality for ‘‘total AHI” with the models for‘‘specific AHI.” In addition, we rescaled this AHI to between 0-500 (AHI0-500) by replacing 10 with 500 in Eq. (5) so that this index matches the current AQI. We also compared the predicting performance of AHI0-500with the ‘‘total AHI.”
Furthermore, we considered the sensitivity analyses by using a natural cubic spline smooth function of the calendar day with 8 or 10 DoF per year instead of 7 DoF in the time-series analyses and by additionally including other air pollutants (PM10, SO2, and CO) as representative pollutants in the construction of the AHI.All statistical analyses were conducted using R software with the ‘‘mgcv”and‘‘tlnise”packages.Two-sided p values less than 0.05 were considered to be statistically significant.
3. Results
3.1. Establishing the AHI
A total of 272 Chinese cities were included in this study.Table 1 summarizes daily deaths,weather conditions,and air pollutants in 272 Chinese cities from 2013 to 2015. On average, there were 16 daily deaths per city and the annual means of PM2.5, NO2, and O3were 56,31,and 77 μg·m-3,respectively.Weather conditions varied across the 272 cities, and the average temperature (annual mean) was 15 °C (range from -0.5 to 25 °C).
The c values and regression coefficients for daily PM2.5,NO2,O3,and temperature are provided in Table 2. The c values were 18.00 and 66.10 in the warm and cold periods, respectively. The coefficients for the all-cause mortality increase per unit change in risk factors were 0.000171, 0.000498, 0.000090, and 0.0239 for PM2.5,NO2, O3, and temperature, respectively, in the warm period; and 0.000212,0.000724,0.000214,and 0.0214,respectively,in the cold period.Therefore,the‘‘total AHI”on any given day and at any location (e.g. Beijing, Shanghai, Wuhan) during the warm and cold periods can be calculated by Eqs. (6) and (7):
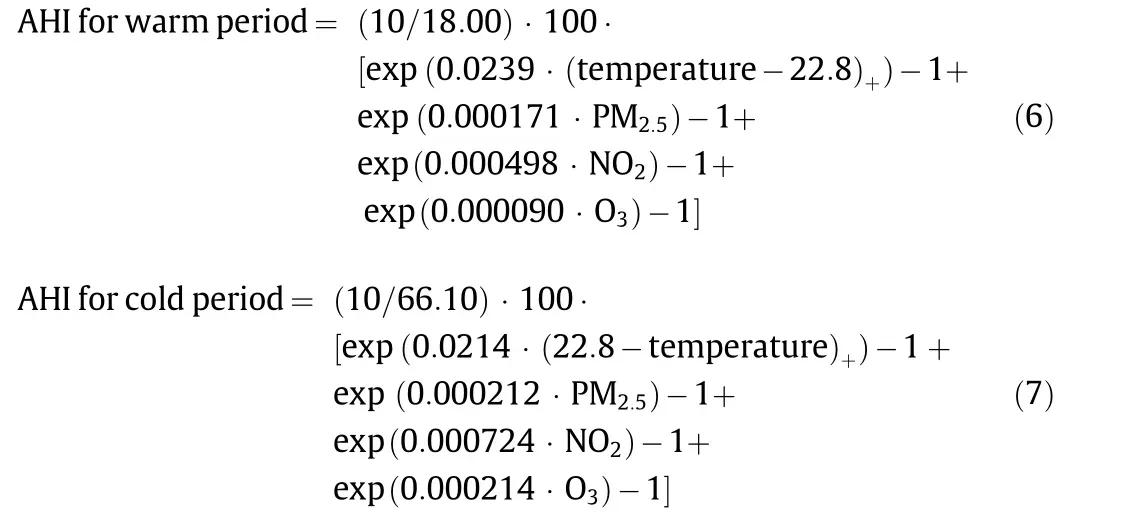
Table3 providesthe descriptive dataofthe AHI,aswellasthedaily excess mortality risk from air pollutants and non-optimum temperature.The average AHI was 6 during the study period across all 272 cities.During the study period,36% of days nationwide had an AHI no greater than 3,21%had an AHI between 4 and 5,24%had an AHI between 6and 8,and20%had anAHI greater than8.The average daily percentage of excess mortality related to air pollution and nonoptimum temperature was 28.23%, among which PM2.5, NO2, O3,and non-optimum temperature accounted for 1.12%, 2.29%, 1.35%,and 23.47%,respectively(as calculated by Eq.(3)).
The c value is the scaling factor that denotes the maximum weighted average of excess deaths per 100 people in the 272 cities.‘‘Warm”is defined as a temperature above the minimum mortality temperature; ‘‘cold” is defined as a temperature below the minimum mortality temperature; and ‘‘coefficient” refers to the total and specific mortality change associated with a unit change in temperature and air pollutants. All AHIs were calculated based on the temperature at lag 0-21 day, PM2.5at lag 0 day, NO2at lag 0 day, and O3at lag 2 day.
3.2. Predicting the performance of the AHI
As shown in Table 4, the AHI is significantly associated with total and cause-specific mortality on the concurrent day. A unit increase in the ‘‘total AHI” is associated with increments of 0.84%(95%confidence interval(CI):0.62%,1.07%)in daily mortality from all causes, 1.01% (95% CI: 0.72%, 1.30%) from overall CVD, 0.98%(95%CI:0.57%,1.40%)from CHD,1.02%(95%CI:0.65%,1.39%)from stroke, 1.66% (95% CI: 1.18%, 2.15%) from overall respiratory diseases, and 1.71% (95% CI: 1.15%, 2.27%) from COPD. As shown in Fig. 1, the E-R curves of the ‘‘total AHI” at the national level with total and specific mortality are almost linear, without anythresholds. In comparison, the coefficient estimates and model fit statistics (R2and AIC) are quite similar between ‘‘total AHI” and‘‘specific AHI”for cause-specific mortality(Table 4).After rescaling the AHI to 0-500, we found that the per-50-unit increases in AHI0-500were associated with 0.91%, 1.13%, 1.18%, 1.07%, 1.79%,and 1.84%increases in total,CVD,CHD,stroke,respiratory diseases,and COPD mortality, respectively (Table S1 in Appendix A). These estimates are comparable to the estimates per one unit increase in the ‘‘total AHI” (0-10 scale).
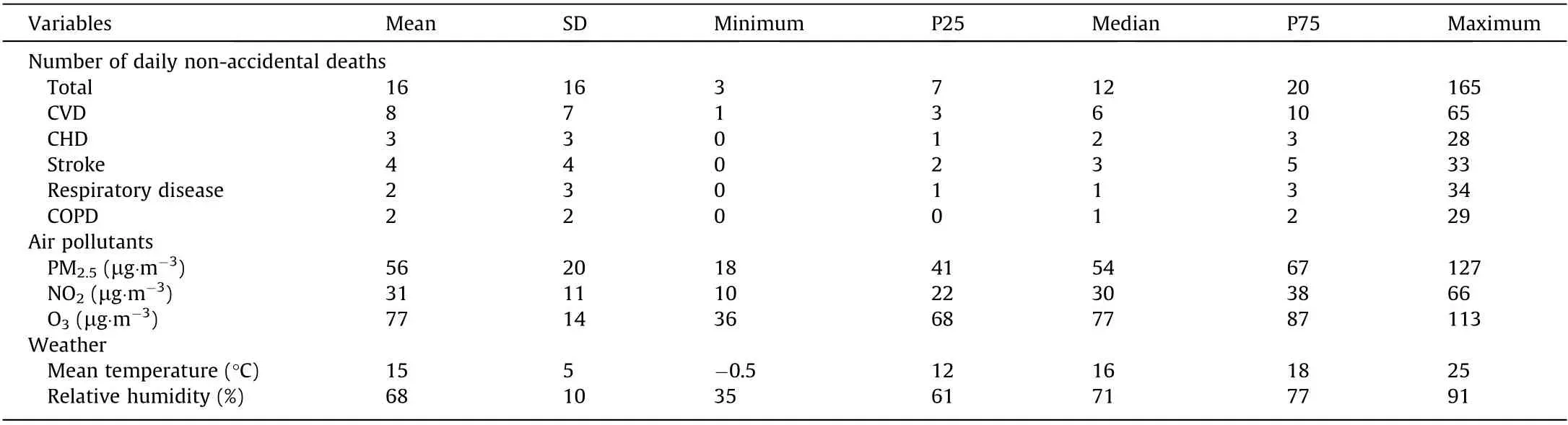
Table 1 Summary statistics of environmental and health data in 272 Chinese cities from 2013 to 2015.
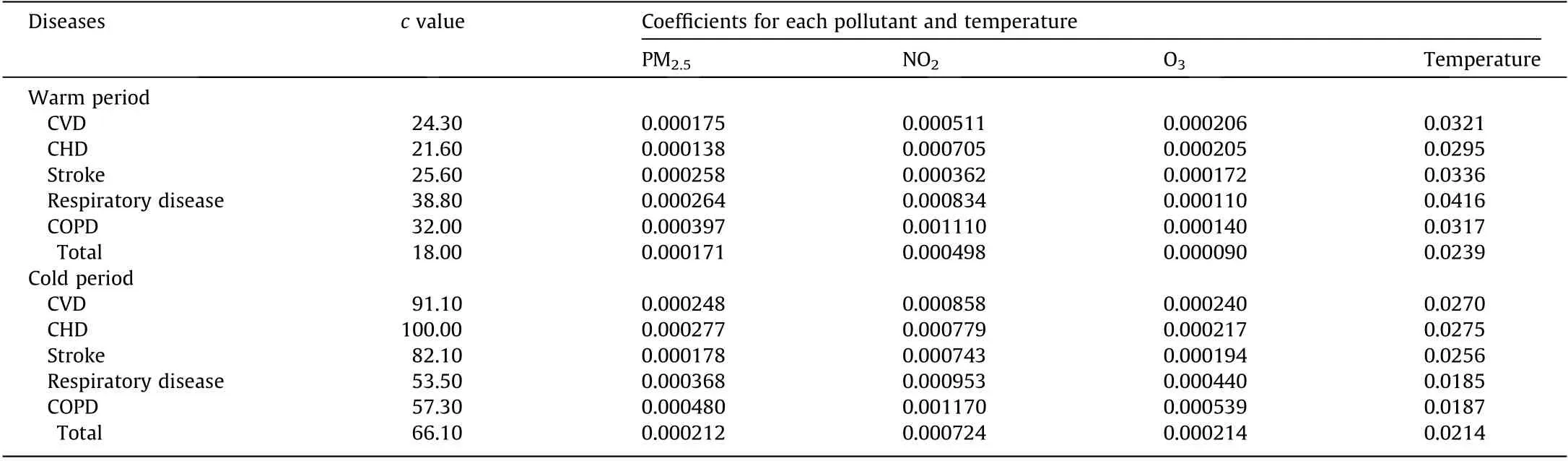
Table 2 Coefficients for each component in the AHI formulas for specific diseases in 272 Chinese cities from 2013 to 2015.
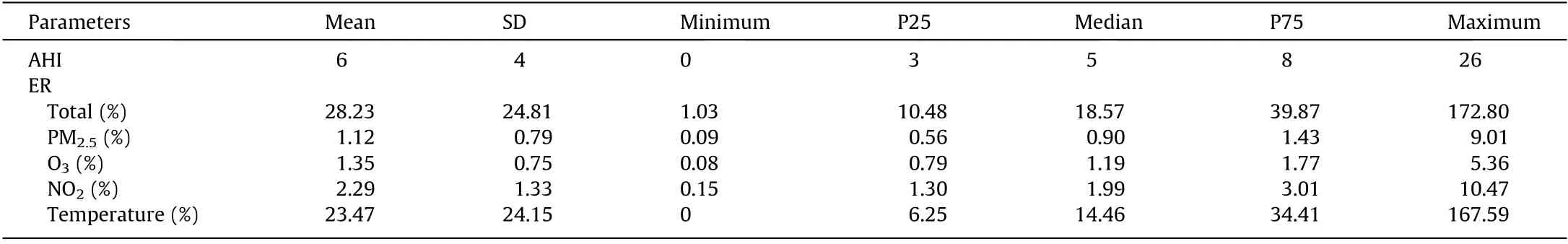
Table 3 Descriptive statistics of AHI and daily excess mortality risk from air pollutants and non-optimum temperature.
The results obtained from the sensitivity analysis after changing the DoF in the natural cubic spline smooth function for the calendar day were comparable to our main models(data not shown).Tables S2 and S3 in Appendix A show the regression coefficients and daily excess mortality risks for PM10, SO2, and CO. The distribution of the AHI was similar with the main results after adding PM10, SO2,and CO to the construction of the AHI(Tables S2-S4 in Appendix A).
Estimates are presented as percentage changes and 95%CI associated per unit increase in indices.
4. Discussion
In this large, multi-city study, we constructed a new AHI for ambient air pollution and non-optimum temperature based on data collected from 272 Chinese cities. Our new index is the first to combine air pollution and temperature in the construction of a health-based exposure index. Our results show that this AHI exhibits good performance in predicting total and cause-specific mortality. Overall, this national AHI has the potential to be a useful tool in communicating short-term health risks from air pollution and temperature exposure to the public in China.
4.1. Formulation of the AHI
Unlike the current AQI, which is solely determined by the air pollutant with the highest AQI score, this new AHI considers the combined health effects of major air pollutants and temperature.In another study, Hu et al. [16] constructed a health-risk-based AQI (HAQI) using the estimated E-R relationships of PM2.5, PM10,SO2,NO2,and O3with daily mortality based on a systematic review of Chinese studies [17]. They found that the HAQI values were higher than the current AQI when multiple air pollutants were simultaneously high, suggesting that the AQI may not capture the combined effects of multiple pollutants in high-exposure scenarios. In addition to air pollution, we introduced non-optimum temperature into our AHI in order to comprehensively evaluate the overall health risk of these major ambient environmental risk factors and to better communicate risk to the public.
Selecting the appropriate risk factors is an important step in establishing the AHI. Similar to that of the HAQI, the AHI formula is determined by the specific air pollutant types included. In its methodology, the AHI formula has a flexibility that allows researchers to include any air pollutant of interest.From an empirical standpoint, it is not ideal to combine the excess health risks from all air pollutants, as doing so may lead to multi-collinearity and overfitting [18]. In this study, we did not include PM10, CO,and SO2for the following reasons: ①A large proportion of the effects of PM10might be attributed to PM2.5; ②the effects of SO2were greatly attenuated after adjustments were made to other air pollutants in our previous publications using the same dataset[19]; and ③ the annual average daily concentrations of CO(1.2 mg·m-3)were found to be well below the air quality standard in China(4 mg·m-3).We finally selected PM2.5,NO2,and O3as the indicators of air quality in the construction of the AHI because they are representative of certain sources and because their associations with daily mortality were independent of other air pollutants[8,10,13].
4.2. AHI validity
We evaluated the performance of our new AHI in predicting the all-cause and cause-specific mortality. Our results showed an almost linear association between ‘‘total AHI” and all-cause mortality, without notable thresholds. These findings confirmed that the AHI exhibits a good performance in predicting the daily total mortality risk.In addition,our‘‘total AHI”yielded similar estimates for its associations with cause-specific mortality compared with those estimated using the ‘‘specific AHI.” Furthermore, the model fit statistics were comparable between these AHIs. These findings confirm that the ‘‘total AHI” may be sufficient for predicting cause-specific mortality related to air pollution and temperature.Although estimating separate AHIs for different causes of mortality can be more accurate when the health outcome of interest is not all-cause mortality, using a single ‘‘total AHI” to indicate allcause and cause-specific mortality may be more convenient and practical for communicating health risks to the public.
4.3. Communication issues
The AHI proposed herein is a comprehensive health-risk communication tool that can be used to inform the public and prompt them to seek mitigations to reduce the harmful health impacts of short-term exposure to ambient air pollution and non-optimal temperature. Moreover, this index not only characterizes the overall risk of simultaneous exposure to all environmental risk factors, but also provides the excess health risk from each exposure.Therefore,it can help to identify the dominant risk factorand guide the public in adopting the most efficient protections.For example,people can reduce the duration and intensity of their outdoor activities, stay indoors, and use an air purifier with the windows closed when PM2.5is the key risk factor. When extreme temperature is the dominant risk factor,people may consider staying indoors with air conditioning and/or appropriate ventilation.To better summarize and interpret this index in terms of health protection, Table 5 lists the health risk levels, potential harmful health effects, and suggested mitigation measures corresponding to different levels of the AHI. The AHI may also have potential to serve as a supplement to the existing AQI and to act as a tool for risk communication to susceptible groups in order to achieve public health benefits.Following our proposed methods,policymakers may develop AHIs based on local environmental conditions and for subgroups of their population.
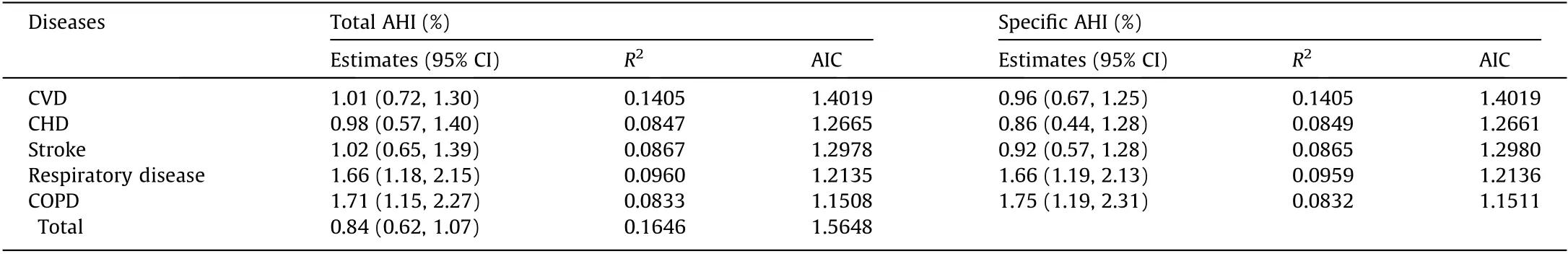
Table 4 Comparisons of the associations of ‘‘specific AHI” and ‘‘total AHI” with daily specific mortality in 272 Chinese cities from 2013 to 2015.
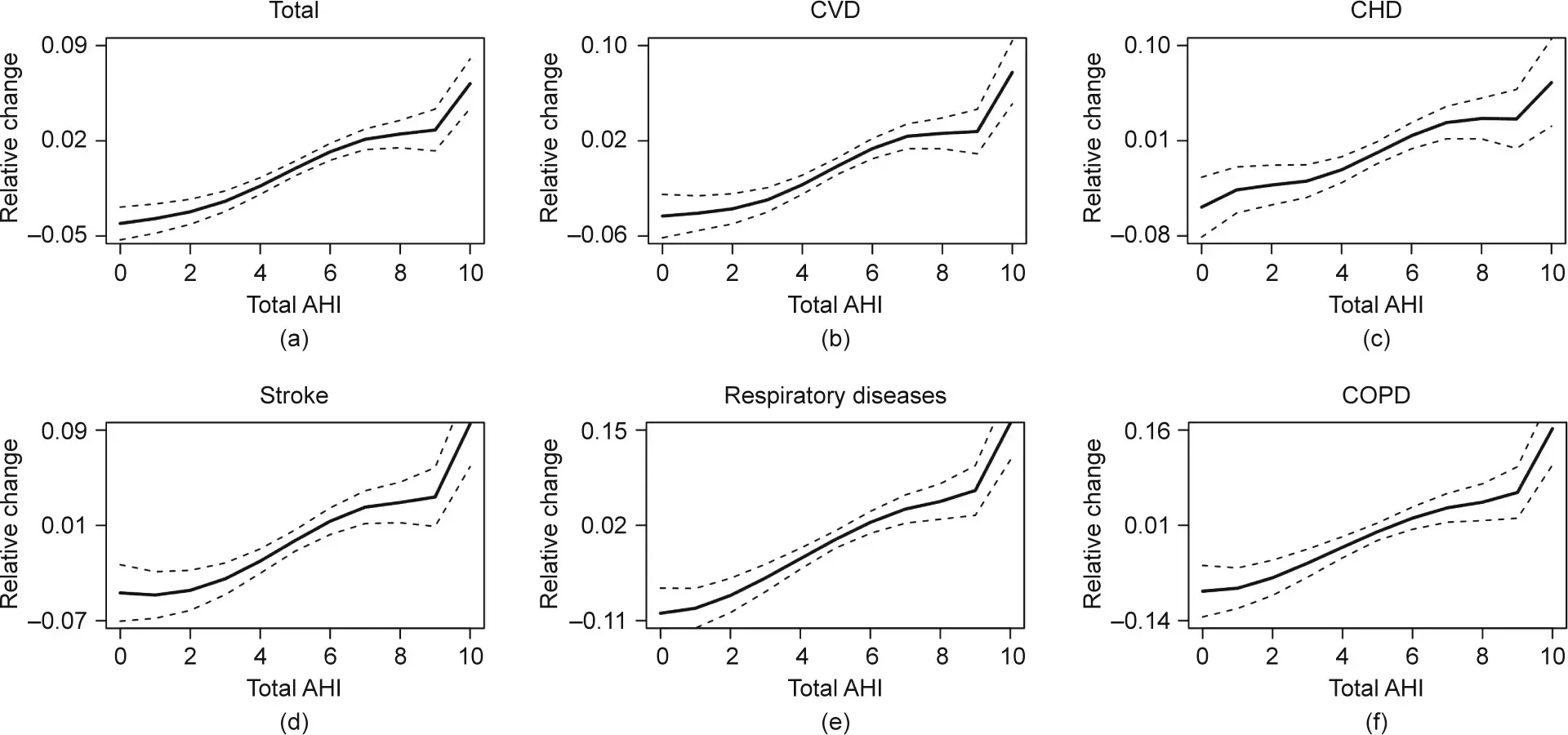
Fig.1. Combined E-R curves for the associations of the present-day AHI with daily(a)total,(b)CVD,(c)CHD,(d)stroke,(e)respiratory diseases,and(f)COPD mortality in 272 Chinese cities from 2013 to 2015.The y-axis can be interpreted as the relative change from the effect of the AHIs on mortality.The solid lines represent mean estimates,and the dashed lines represent their 95%CI.
4.4. Strengths and limitations
The study has several strengths.First,we established a national AHI using a large, multi-city dataset in the mainland of China.Therefore,our results have nationwide representativeness.Second,compared with other indices, we integrated non-optimum temperature and air pollution together in this AHI, which can better reflect the actual exposure scenario in reality and lead to a more comprehensive risk assessment. Third, our AHI can provide not only the overall health risk due to simultaneous exposure to these factors, but also the excess mortality risk from each individual factor, so as to better inform the public and prompt them to seek targeted protection.
This work has some limitations. First, as we obtained exposure data (air pollutants and temperature) from fixed-site monitors in each city, exposure misclassification was inevitable. Second, we only included the most severe health event—that is, mortality—as the health outcome due to limited data availability, so morbidity was not considered. As a result, the current AHI may have a limited ability to capture more acute and relatively weaker health effects. Third, the index uses an E-R function derived from local contexts, so the predictability of the AHI is related to the local characteristics. In a large area such as the whole country, the predictability is less stable than in a small area where the atmospheric and population characteristics are more homogeneous.In addition, given the limited availability of data, we could not include more recent data to examine the predictive ability of the AHI in this study.
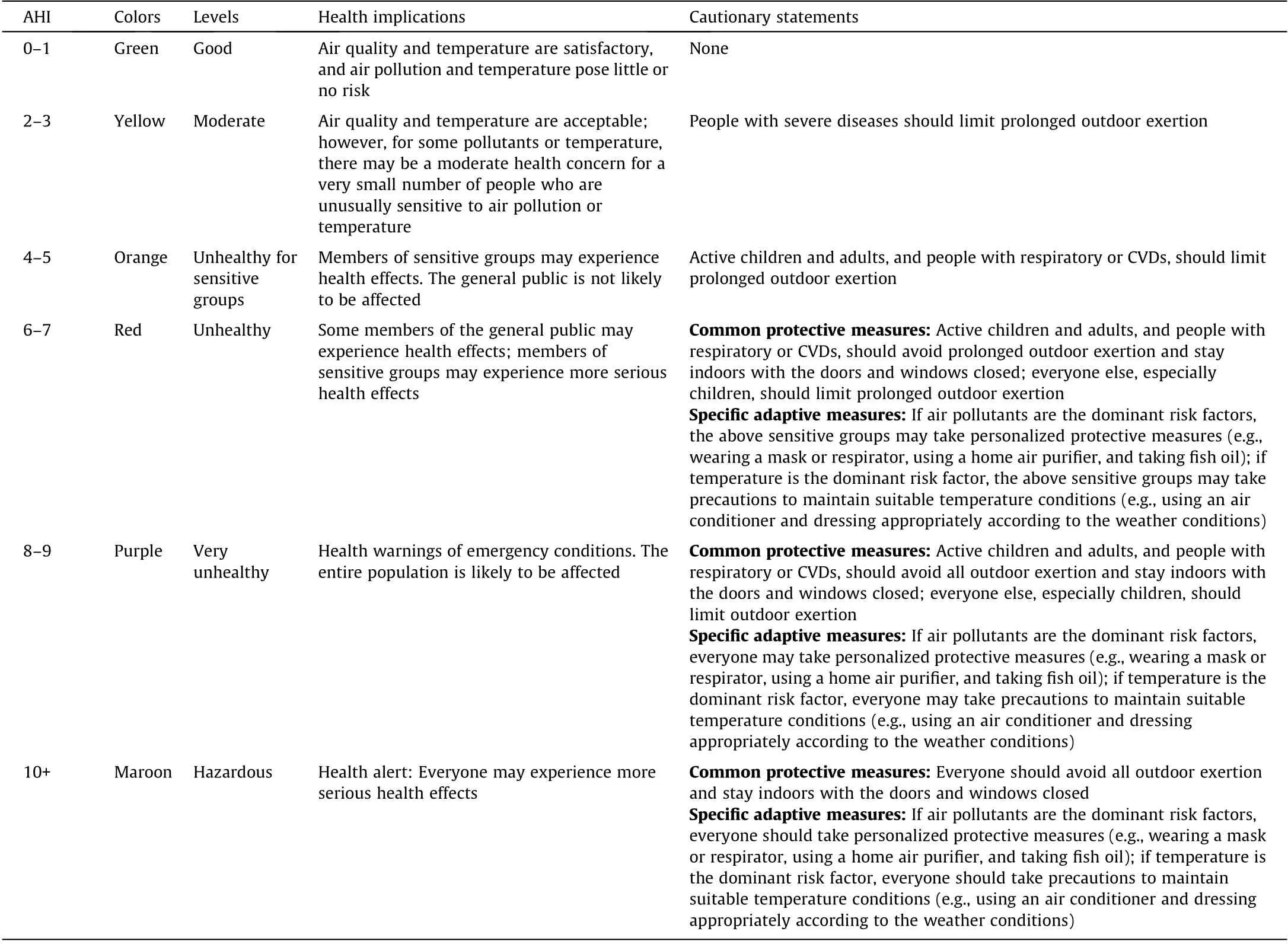
Table 5 Values, levels, implications, and cautionary statements in the AHI for public communication.
5. Conclusion
In this work, we established a new AHI based on the associations of PM2.5, NO2, O3, and temperature with daily total mortality using 272 cities in the mainland of China from 2013 to 2015. The‘‘total AHI” was found to be significantly associated with total and cause-specific mortality. The E-R curves for the associations between the AHI and mortality were approximately linear,without any thresholds. This index provides a flexible and promising tool for communicating health risks related to exposure to different ambient environmental risk factors to the public.
Acknowledgment
The study was supported by the National Natural Science Foundation of China (92043301, 82030103, and 91843302), and the Research Program of the Shanghai Meteorological Service(ZD201904).
Compliance with ethics guidelines
Qingli Zhang, Renjie Chen, Guanjin Yin, Xihao Du, Xia Meng,Yang Qiu, Haidong Kan, and Maigeng Zhou declare that they have no conflict of interest or financial conflicts to disclose.
Appendix A. Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.eng.2021.05.006.
- Engineering的其它文章
- The Pathway Toward Carbon Neutrality: Challenges and Countermeasures
- Weights-Based Gravity Energy Storage Looks to Scale Up
- New US Rules Promise to Unlock Hearing Aid Availability
- Flow in Porous Media in the Energy Transition
- Reactive Extrusion (REx): Using Chemistry and Engineering to Solve the Problem of Ocean Plastics
- A Future Perspective on In-Sensor Computing

