Anti-Müllerian hormone and antral follicle count predict ovarian response in women less than 45 years following GnRH antagonist multiple-dose protocol
Mohammed M.Laqqan ,Maged M.Yassin
1Department of Laboratory Medical Sciences,Faculty of Health Sciences,Islamic University of Gaza,P.O.Box 108,Gaza,Palestine
2Department of Human Physiology,Faculty of Medicine,Islamic University of Gaza,P.O.Box 108,Gaza,Palestine
ABSTRACT Objective:To speculate which of the following parameters: antral follicle count (AFC),anti-Müllerian hormone (AMH),folliclestimulating hormone (FSH) and age can be used as a predictor of ovarian response to gonadotropin-releasing hormone (GnRH)antagonist stimulation multiple-dose protocol in women under 45 years,and to determine the cutoff value of these parameters and their correlations for predicting low and high ovarian response.Methods:This prospective study included 462 women with the mean age of (29.3±6.5) years.All women were subjected to the GnRH antagonist stimulation multiple-dose protocol.On the second day of the menstrual cycle,ultrasonography was conducted to determine AFC in both ovaries.Peripheral blood samples were collected to evaluate the level of estradiol,FSH,luteinizing hormone,prolactin,thyroid-stimulating hormone,and AMH.The women were divided into three groups: low response(AHH<1 ng/mL,n=173),normal response (AMH=1.0-3.5 ng/mL,n=175),and high response (AMH >3.5 ng/mL,n=114).Results:A significant decrease was found in the age and FSH level in the high response group compared to other groups (P<0.001).Conversely,a significant increase was shown in AMH,estradiol on human chorionic gonadotropin (hCG) day,AFC,mature oocytes,fertilized oocytes,and embryos transferred in the high response group compared to the other two groups (P<0.001).The receiver operating characteristic (ROC) curves demonstrated that AFC and AMH had the highest accuracy,followed by basal FSH level and age in the prediction of low ovarian reserves (P<0.001) with cutoff values of ≤4.50 and ≤0.95 for AFC and AMH,respectively.Moreover,the ROC analysis showed that AFC had the highest accuracy,followed by AMH level and age in the prediction of high ovarian reserves with a cutoff value of ≥14.50,≥3.63,and ≤27.50 years,respectively (P<0.01).A significant decrease was observed in women's age,estradiol level,and oocyte fertilization rate in pregnant women compared to non-pregnant women (P<0.001).Additionally,significant negative correlations were found between the AFC,the number of mature oocytes,fertilized oocytes,embryos transferred,and the age of pregnant women (P<0.001).Conclusions: AFC and AMH predict low and high ovarian response to GnRH antagonist stimulation multiple-dose protocol in women under 45 years.
KEYWORDS: Antral follicle count;Anti-Müllerian hormone;Antagonist;Controlled ovarian stimulation;GnRH;Multiple-dose;Ovarian response
1.Introduction
Infertility is a disease characterized by the failure to establish a clinical pregnancy after one year of unprotected sexual intercourse.Approximately 8%-12% of reproductive-aged couples worldwide are suffering from infertility problems[1].Female infertility is considered a primary reason for about 65% of infertile couples.Advanced maternal age,tubal damage due to infections,polycystic ovary syndrome,and endometriosis were classified as the most common causes of women’s infertility[2].Infertility problems are considered a common feature in couples attending a fertility center;most fertility centers perform ovarian reserve tests as part of the evaluation of women before undergoing controlled ovarian stimulation and intracytoplasmic sperm injection (ICSI)[3].A study noted that the ovarian reserve is reduced in females during the mid to late thirties and at times earlier,reflecting the declining oocyte quality and quantity[4].The controlled ovarian stimulation with exogenous gonadotropin hormones is used to obtain a large number of mature oocytes which is considered a very critical step in the procedure of ICSI[5].Nevertheless,the prediction of ovarian response to the controlled ovarian stimulation program is difficult and variable.This leads to an inadequate response,which involves poor ovarian response or ovarian hyperstimulation syndrome (OHSS),leading to the cancelation of the ICSI cycle[6].
During the past years,several ovarian reserve biomarkers have been proposed to predict a possible response to controlled ovarian stimulation to obtain good results or to adjust the controlled ovarian stimulation protocols with the appropriate doses of administered gonadotropins[7].Anti-Müllerian hormone (AMH),folliclestimulating hormone (FSH),and antral follicle count (AFC) are considered the most predictors used for ovarian response assessment.However,selecting one of these variables as a preferred indicator in clinical practice is still a highly debated issue[8].Recently,there is an interest in AMH and its uses to predict ovarian response for patients undergoing ovarian stimulation protocol.
AMH is a dimeric glycoprotein that belongs to the family of transforming growth factor-beta and is secreted by granulosa cells[9].AMH is produced constantly by pre-antral and small antral follicles[10].Approximately 60% of serum AMH is derived from follicles 5-8 mm in diameter[11].The level of serum AMH depends on the number of developing follicles,and in turn,this controls the recruitment and growth of primary follicles[9].A study reported that AMH level indicates the quantity and quality of the ovarian follicular pool[12].AMH is highly expressed during the reproductive life of females until menopause where it is undetectable after this stage[10].
Traditionally,the ovary reproductive potential was evaluated by determining the levels of basal serum FSH or estradiol (E2)[13].However,these hormones are dependent on the number of developing oocytes and fluctuate during the menstrual cycle.Additionally,these hormones are affected by artificial hormonal variations including those arising from the use of oral contraceptives[14].Consequently,using these hormones to evaluate ovarian response may be inaccurate[15].On the other hand,there are distinct differences between the use of AFC and AMH in ovarian response evaluation.Previous studies reported that the advantages of AMH include a less invasive procedure (it is assessed through a simple blood test),and lower intra-and inter-cycle variability,which suggests that it can be predictive at any time during the menstrual cycle[16].Today,fertility centers use both AMH level and AFC to predict potential ovarian response for stimulation protocol by recombinant follicle-stimulating hormone (r-FSH),oocyte yield,and the possibility of pregnancy outcome in assisted reproductive technology[17].Although AFC and AMH have been reported to correlate with ovarian response[18,19],the correlation of AMH level with ovarian reserve and response is still unclear.Therefore,this study was performed to (Ⅰ) speculate which of the following parameters: AFC,AMH,basal level of FSH and age can be used as a predictor of ovarian response to GnRH antagonist stimulation multiple-dose protocol in women under 45 years,(Ⅱ) determine the cutoff value of AFC,AMH,FSH,and age for predicting low and high ovarian response,and (Ⅲ) investigate the correlation between age,hormone levels,and other clinical parameters.
2.Materials and methods
2.1.Study population
This prospective study included 462 women with a mean age of(29.3±6.5) years old and was conducted between January 2011 and September 2014.All women were subjected to the GnRH antagonist stimulation multiple-dose protocol in Al Bassma Fertility Center in Palestinian Territories.The sample size was calculated based on the formula for a cross-sectional study where the EPI-INFO statistical package version 7.2 was used with a 99.9% confidence interval(CI),85% power,and 0.4 ratios.All the participants were selected according to the following inclusion criteria: women aged between 20 to 45 years old,women undergoing the first ICSI cycle,women undergoing GnRH antagonist multiple-dose protocols,a normal body mass index,women who had a regular menstrual cycle,and the male partner had normal semen parameters.On the other hand,the exclusion criteria included cigarette smokers,diabetes mellitus,women using oral contraceptives,women suffering from endocrine abnormality and polycystic ovary syndrome,women with a history of ovarian surgery,and women suffering from recurrent abortion.The medical records were used by the researcher to gather general and medical information that included women's age,hormone profile,AFC,number of mature oocytes,immature oocytes,fertilized oocytes,number of embryos transferred,and the pregnancy results[β-human chorionic gonadotropin (β-hCG) level].
2.2.AFC measurement and hormonal assays
On the second day of the menstrual cycle,ultrasonography was conducted to evaluate the status of the female reproductive system and to determine AFC in both ovaries.Peripheral blood samples were collected,and then the serum was immediately separated by centrifugation at 2 058 ×gfor 20 min.The serum was used to evaluate the basal levels of E2,FSH,luteinizing hormone (LH),prolactin (PRL),thyroid-stimulating hormone(TSH) and AMH using the Tosoh Instrument (AIA-360,Tokyo,Japan).The women undergoing GnRH antagonist stimulation multiple-dose protocol were divided into three groups according to the AMH level: low response (AHH <1 ng/mL,n=173),normal response (AMH=1.0-3.5 ng/mL,n=175),and high response (AMH >3.5 ng/mL,n=114)[20].
2.3.Controlled ovarian stimulation treatment
The GnRH antagonist multiple-dose protocol involved the administration of 0.25 mg cetrorelix or ganirelix (Merck Serono)daily from day 5 of stimulation with gonadotropins,or when the leading follicle was 14-15 mm,until the day of hCG administration.At this dose,the premature LH surge was prevented and good clinical outcomes were obtained after stimulation with r-FSH[21].The used dose of gonadotropins is variable (with a minimal daily dose of 300 IU) depending on the patient's age.The oocyte pickup was scheduled for 33-36 h after the administration of 5 000 to 10 000 IU of hCG (Pregnyl) depending upon the age of the female and the number of oocytes.Sixteen to eighteen hours after the ICSI procedure,fertilization was evaluated by checking the number of polar bodies and pronuclei,and embryo cleavage was evaluated 48 h after ICSI.A maximum of three embryos with high-quality (grade Ⅰ or Ⅱ) were transferred on the third day after ICSI fertilization.All women received luteal support with vaginal progesterone until a pregnancy test was performed after 2 weeks from embryo transfer.Pregnancy was confirmed byβ-hCG measurement (> 5 mIU/mL) on day 12 after embryo transfer.
2.4.Statistical analysis
All the data were analyzed using IBM SPSS for Windows software package version 24.0 (SPSS,Inc.,Chicago,USA).Data included in this study were non-normally distributed (non-parametric) according to the value of the Skewness test,Kurtosis test,andZ-value.So,the data were presented as the median and interquartile range (IQR).Kruskal-Wallis (H-test),and Mann-Whitney (U-test) were applied to compare the quantitative variables among the study groups.Spearman's rank correlation coefficient was used to evaluate the correlations between the clinical parameters.Receiver operating characteristic (ROC) curves were created for AFC,AMH,female age,and basal level of FSH to investigate their ability to predict low or high ovarian response.The results in the above-mentioned tests were accepted as statistically significant whenP<0.05.
2.5.Ethics approval and consent to participate
This study was approved by the Health Research Council,Palestinian Territories (Reference.No.PHRC/HC/03/10),and consent was provided according to the Declaration of Helsinki Committee.Besides,all participants signed an informed approval form to participate in this study.The samples were analyzed according to the guidelines and standard procedures of the Al Basma Fertility Center,Palestinian Territories.
3.Results
3.1.Clinical parameters among different ovarian response groups
This study consisted of 462 women with a mean age of (29.3±6.5)years old.The women were divided into three groups according to the AMH level: low response 173 (37.4%),normal response 175 (37.9%),and high response 114 (24.7%).As illustrated in Table 1,women's age,basal levels of FSH and TSH in the high ovarian response group were significantly lower than the normal and low ovarian response groups (P<0.001,P<0.001,andP=0.005,respectively).A significant variation was found between the study groups in the basal levels of E2,LH,and oocyte fertilization rate(P=0.031,P=0.011,andP<0.001,respectively).On the other hand,significantly higher values of AMH,E2on hCG day,AFC,number of mature oocytes,immature oocytes,fertilized oocytes,number of embryos transferred,andβ-hCG were observed in the high ovarian response group compared to the other groups (allP<0.001).
3.2.Correlations between clinical parameters of the study population
Table 2 reveals significant negative correlations between E2level on hCG day (r=-0.318,P<0.001),AFC (r=-0.452,P<0.001),number of mature oocytes (r=-0.433,P<0.001),immature oocytes(r=-0.310,P<0.001),fertilized oocytes (r=-0.408,P<0.001),and the age of women.Conversely,significant positive correlations were found between E2level on hCG day (r=0.473,P<0.001),AFC (r=0.822,P<0.001),number of mature oocytes (r=0.781,P<0.001),immature oocytes (r=0.603,P<0.001),fertilized oocytes (r=0.784,P<0.001),number of embryos transferred (r=0.395,P=0.001),β-hCG level (r=0.303,P<0.001),and AMH level.Significant positive correlations were also found between AFC,the number of mature oocytes,immature oocytes,fertilized oocytes (allP<0.001),level of E2on hCG day (P=0.010),and the basal level of LH.
3.3.Predictive values of ovarian reserve tests and age for ovarian response
As pointed out in Table 3,the ROC curves in the low ovarianresponse group displayed that AFC and AMH level had the highest accuracy (AUC 0.99,95%CI0.97-1.00;AUC 0.96,95%CI0.94-0.98,respectively;P<0.001) (Figure 1A and 1B) followed by the basal level of FSH (AUC 0.72,95%CI0.67-0.77,P<0.001) (Figure 1C) in prediction of the low ovarian response compared with the women's age (AUC 0.69,95%CI0.64-0.74,P<0.001) (Figure 1D).The selected cutoff value of AFC was ≤4.5 (sensitivity 96.12%,specificity 98.36%),AMH level was ≤0.95 (sensitivity 97.57%,specificity 91.80%),the basal level of FSH was ≥10.15 (sensitivity 58.47%,specificity 86.89%),and that of the women age was ≥31.50(sensitivity 53.01%,specificity 79.13%) for prediction of the low ovarian response.On the other hand,the ROC curve analysis in the high ovarian response group showed that AFC had the highest accuracy (AUC 0.98,95%CI0.96-1.00,P<0.001) (Figure 2A)followed by AMH level (AUC 0.88,95%CI0.84-0.92,P<0.001)(Figure 2B) in prediction of the high ovarian response compared with the women's age (AUC 0.61,95%CI0.54-0.68,P=0.005)(Figure 2C).The basal level of FSH had the lowest accuracy (AUC 0.57,95%CI0.49-0.64,P=0.086) (Figure 2D).In the prediction of high ovarian response,the optimum cutoff value of AFC,AMH level,and women's age was ≥14.50 (100.00% sensitivity,96.60%specificity),≥3.63 (78.08% sensitivity,76.70% specificity),and≤27.50 (50.49% sensitivity,78.08% specificity),respectively.
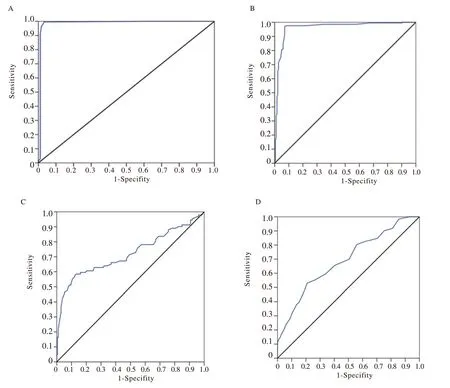
Figure 1.Receiver operating characteristic (ROC) curve of clinical parameters to predict low ovarian response.A: antral follicle count (AFC);B: anti-Müllerian hormone (AMH) level;C: basal level of follicle-stimulating hormone (FSH);D: women's age.
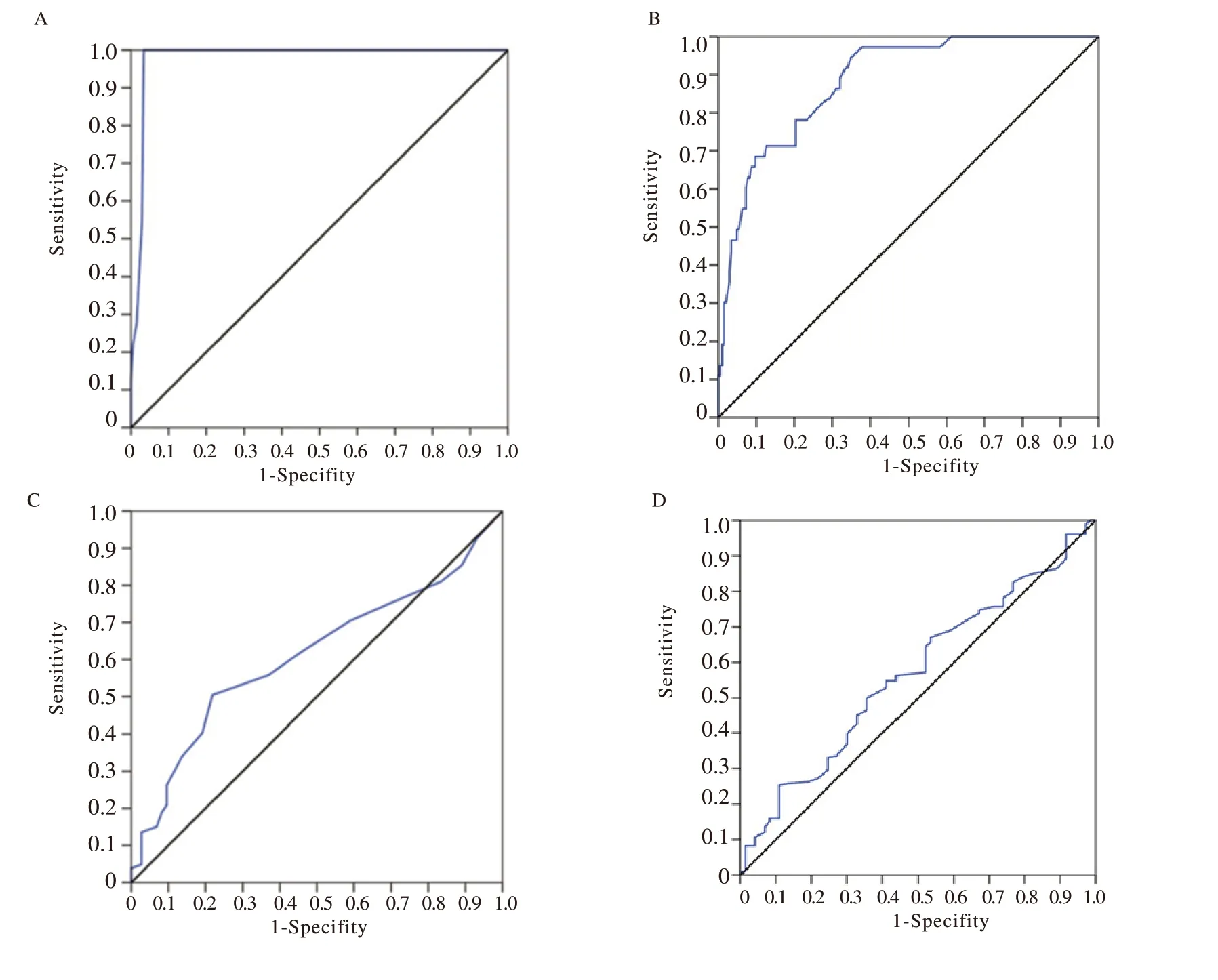
Figure 2.Receiver operating characteristic (ROC) curve of clinical parameters to predict high ovarian response.A: antral follicle count (AFC);B: anti-Müllerian hormone (AMH) level;C: women's age;D: basal level of follicle-stimulating hormone (FSH).
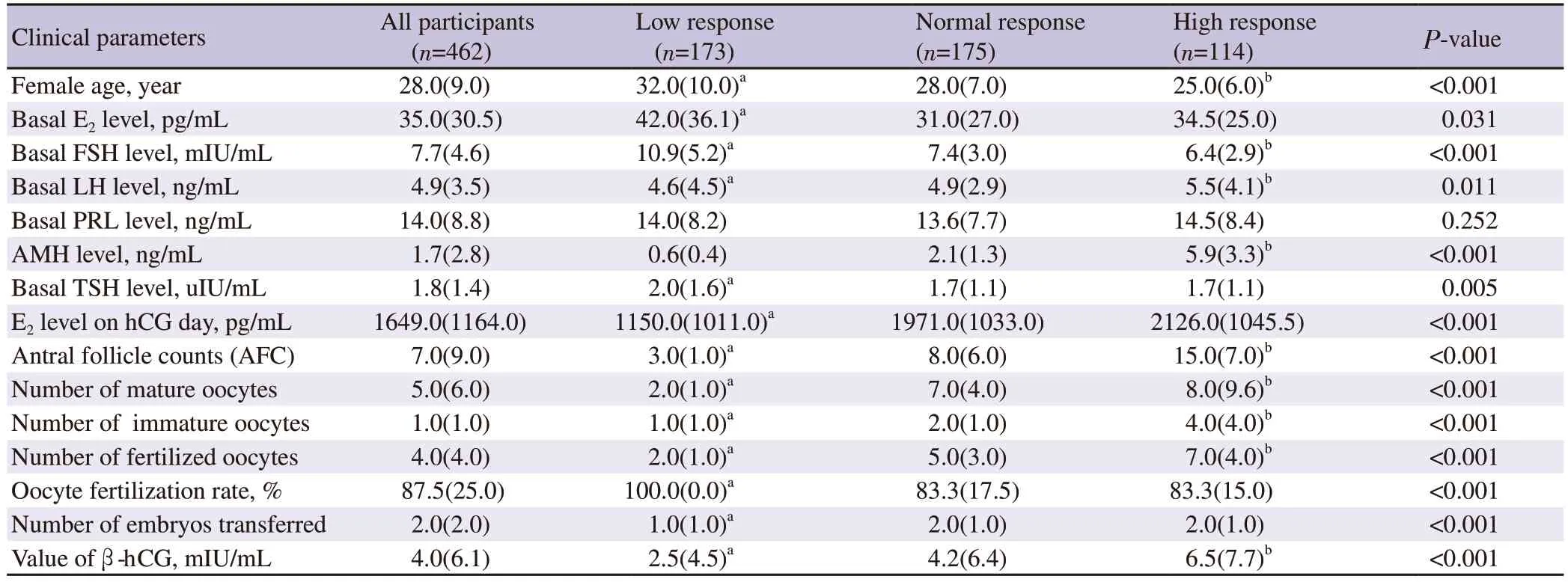
Table 1.Clinical parameters of the study population.

Table 2.Correlation (r) between the clinical parameters of the study population.
3.4.Clinical parameters of pregnant women and their correlations
Table 4 shows significant decreases in the women's age,basal level of E2,and the oocyte fertilization rate in pregnant women compared to non-pregnant women (P<0.001).In contrast,significant increases were found in the level of AMH,AFC,number of mature oocytes,immature oocytes,fertilized oocytes,and number of embryostransferred in pregnant women compared to non-pregnant women(P<0.001).The Spearman’s correlation test in Table 5 illustrates significant negative correlations between the level of E2on hCG day (r=-0.363,P<0.001),AFC (r=-0.406,P<0.001),the number of mature oocytes (r=-0.389,P<0.001),fertilized oocytes (r=-0.393,P<0.001),embryos transferred (r=-0.357,P<0.001),and the age of pregnant women.Additionally,significant negative correlations were found between the same clinical parameters except for oocyte fertilization rate and the basal level of FSH in pregnant women(P<0.001).On the other hand,significant positive correlations were reported between the level of E2on hCG day (r=0.545,P<0.001),AFC (r=0.787,P<0.001),the number of mature oocytes (r=0.690,P<0.001),immature oocytes (r=0.613,P<0.001),and fertilized oocytes (r=0.699,P<0.001),number of embryos transferred (r=0.402,P<0.001),and the level of AMH in pregnant women.
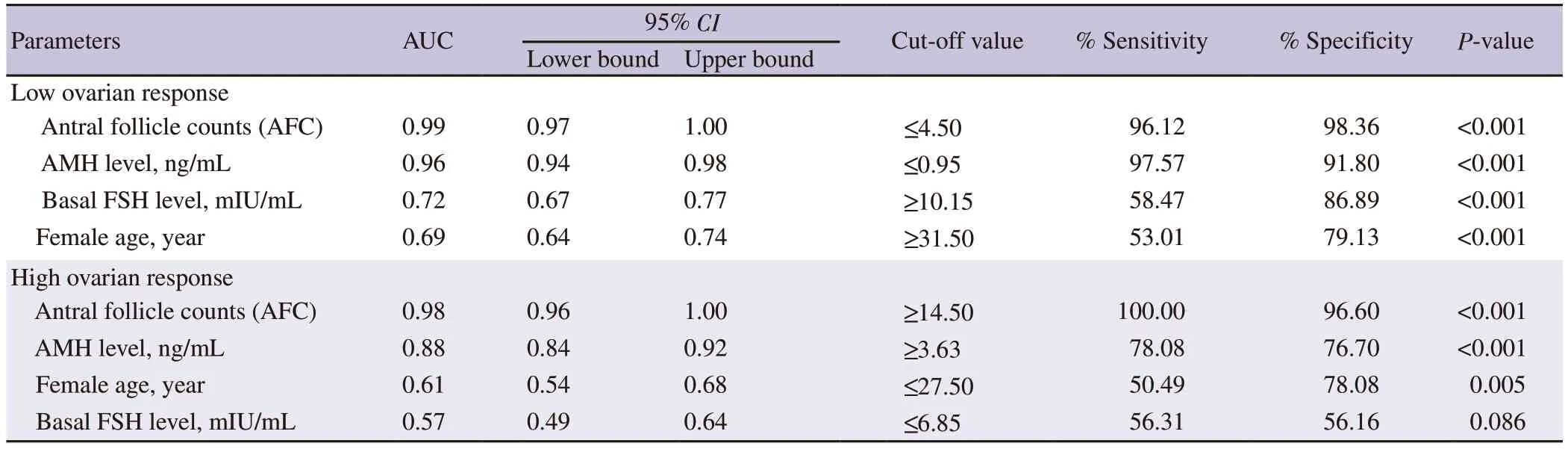
Table 3. Predictive values of antral follicle counts,basal FSH level,and age for ovarian response.
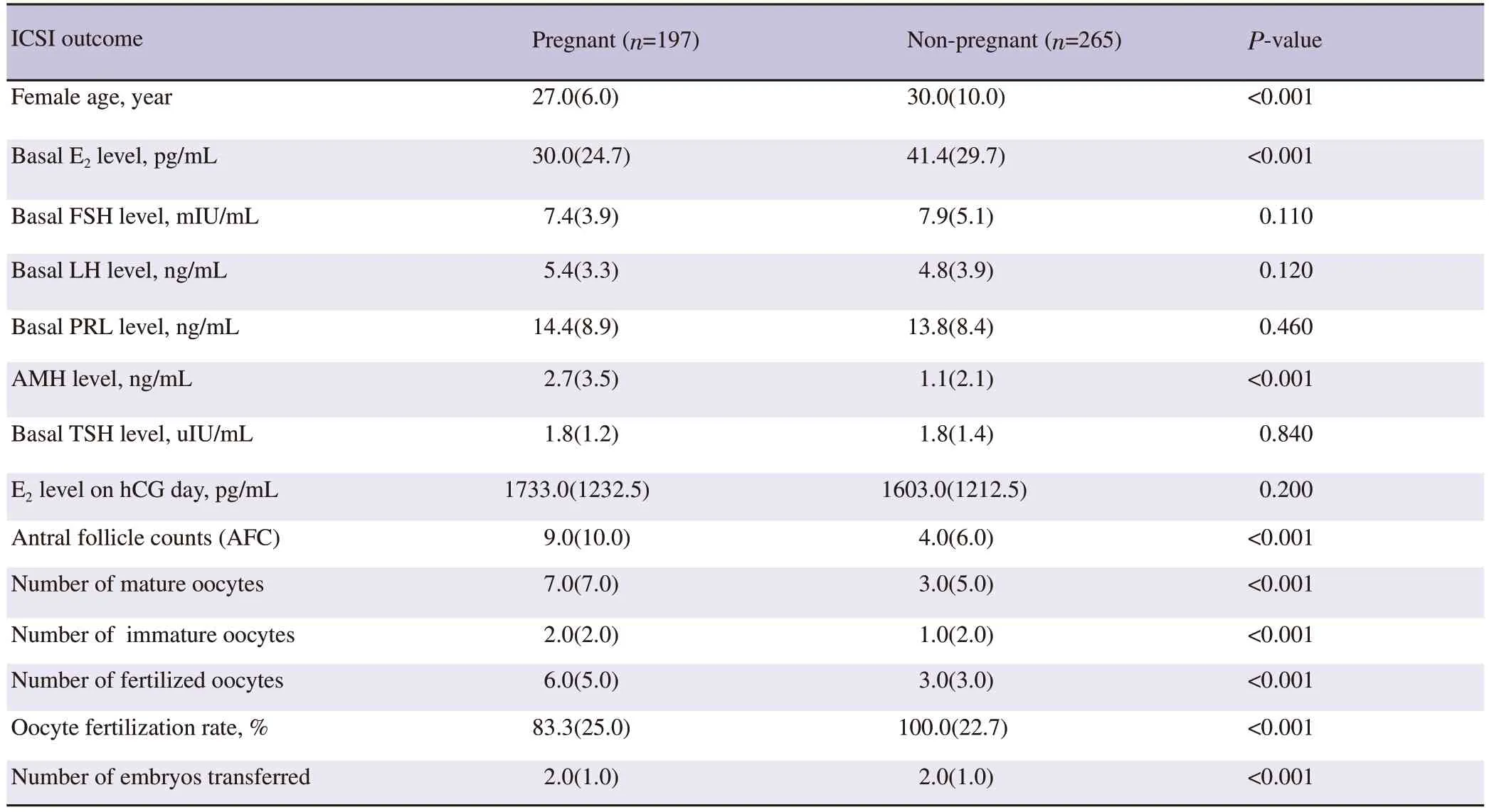
Table 4.Clinical parameters of pregnant women compared to non-pregnant women.
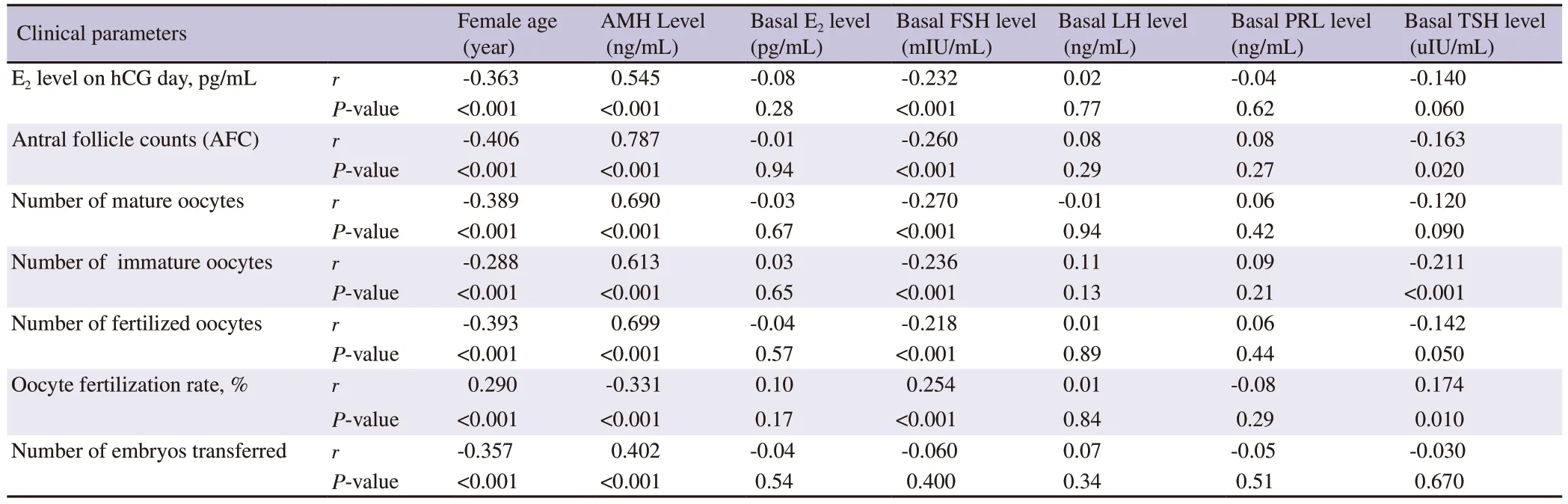
Table 5.Correlations (r) between the clinical parameters in pregnant women (n=197).
4.Discussion
To increase the success rate of the ICSI outcome in the first cycle,it is essential to recognize the ovarian reserve and the potential ovarian response.The risk of ovarian response decline during assisted reproductive technology increases in older women[22].Consequently,the proper estimation of ovarian reserve and correct identification of ovarian response degree is important to improve overall ICSI outcomes and pregnancy rate in women undergoing the ICSI cycle.A previous study indicated that there are several factors like women's age,basal level of FSH,AMH,and AFC that could be used as clinical predictors of oocyte yield and ovarian response during ovarian stimulation protocol[23].
In this study,the results of ROC were used to evaluate the performance of women’s age,AMH level,basal level of FSH,and AFC as potential predictor factors of the ovarian response in women less than 45 years old undergoing the first ICSI cycle with GnRH antagonist multiple-dose protocols.Significant increases were found in the level of AMH,E2on hCG day,the value ofβ-hCG,AFC,number of mature oocytes,immature oocytes,fertilized oocytes,and embryos transferred in the high ovarian response group compared to other groups.Besides,significant reductions were found in the female age,basal level of FSH,and TSH in the high ovarian response group compared to other groups.All of these findings are in agreement with a previous study prepared by Lekamge and his colleagues who found a reduction in the AFC,mature oocytes,the value ofβ-hCG,fertilized oocytes,and the number of embryos transferred in the low AMH group compared to the high AMH group[13].Additionally,another study showed significant increases in the level of AMH,E2on hCG day,AFC,the number of mature oocytes,immature oocytes,fertilized oocytes,number of embryos transferred,and the value ofβ-hCG,whereas significant reductions were observed in the women's age,basal E2level,and oocyte fertilization rate among the responder groups[18].Another study also supported such findings[24].
In the present investigation,significant negative correlations were found between the level of E2on hCG day,AFC,the number of mature oocytes,immature oocytes,fertilized oocytes,embryos transferred,level ofβ-hCG,and the age of women.Also,significant negative associations were found between the AFC,the number of mature oocytes,fertilized oocytes,embryos transferred,the value ofβ-hCG,and the basal E2level.Conversely,significant positive correlations were registered between the level of E2on hCG day,AFC,number of mature oocytes,immature oocytes,fertilized oocytes,embryos transferred,level ofβ-hCG,and AMH level.Similar results showed significantly positive correlations between the number of oocytes,embryos transferred with AMH,and AFC[24].Besides,another study found that AFC correlates with the number of mature oocytes[25].Furthermore,AFC was reported to be strongly related to the level of AMH[26].The results of our study present multiple lines of evidence that women with a high AMH level have higher reproductive potential and ovarian reserve compared to women with a low AMH level.Women who have a high level of AMH can give a high number of oocytes (mature and immature),a higher rate of fertilized oocytes,and a high number of embryos transferred.Consequently,an increase in the pregnancy rate per ICSI cycle ultimately was observed.Several previous studies support these findings[18,27].
With regard to the ability of ovarian reserve tests and age to predict ovarian response,the study results showed that AFC and AMH level had the highest accuracy (AUC=0.99;AUC=0.96,respectively)followed by basal FSH level (AUC=0.72) and the women's age(AUC=0.69) in the prediction of low ovarian response.Additionally,the results of the ROC curve showed that AFC had the highest accuracy (AUC=0.98),followed by AMH level (AUC=0.88) and the women's age (AUC=0.61) in the prediction of high ovarian response.These findings are in the line with previous studies which pointed out that AFC and AMH were the best predictor factors of high and low ovarian response[28,29].Another study concluded that age and AMH are good predictors of ovarian reserve and response in women undergoingin vitrofertilization[30].Several studies have reported that AFC and AMH were superior to the other ovarian tests to predict ovarian response in assisted reproduction[19,31].In accordance with our findings,many studies concluded that AFC and the level of AMH are the most reliable ovarian reserve markers to predict excessive response in controlled ovarian hyperstimulation[32].Other studies showed AUC of 0.79 for AFC in excessive response women and 0.76 for AFC in the poor ovarian response women.Based on these studies,AFC is one of the best markers to predict poor and excessive ovarian responses to controlled ovarian hyperstimulation[31,33].Nevertheless,other studies showed that women’s age is the most accurate compared to the basal level of FSH.The AUC for age was higher than the basal level of FSH[34,35].
The current study observed a significant decline in the age,basal level of E2,and the oocyte fertilization rate in pregnant women compared to non-pregnant women.Conversely,a significant increase was found in the AMH level,AFC,the number of mature oocytes,immature oocytes,fertilized oocytes,and the number of embryos transferred in pregnant women compared to non-pregnant women.These findings are matching with other previous studies which showed that the women's age is one of the factors attributing to clinical pregnancy,and that is very easy to understand[18,36].With women aging,the quality and quantity of oocytes decline,which leads to an increased rate of infertility and a reduced chance of clinical pregnancy during the ICSI cycle[37,38].
Significant negative correlations were found between the level of E2on hCG day,AFC,mature oocytes,immature oocytes,fertilized oocytes,embryos transferred,and the age of pregnant women.Additionally,significant negative correlations were observed between the same clinical parameters -except oocyte fertilization rate-and the basal level of FSH in pregnant women.Conversely,significant positive correlations were reported between the level of E2on hCG day,AFC,the number of mature oocytes,immature oocytes,fertilized oocytes,embryos transferred,and AMH level in pregnant women.These results coincide with previous studies that found an association between AMH level and oocyte yield and suggested that AMH could be used to predict pregnancy outcomes[39,40].Moreover,several studies revealed that low AMH levels correlated with lower rates of clinical pregnancies and higher cancelation rates for the ICSIcycle[41,42].
One of the limitations of this study is the need for future studies to investigate the relationship between embryo development,pregnancy outcomes,and predictive factors of ovarian response (AMH,AFC,and age).
In conclusion,this study exhibits that AFC and AMH level are the best candidates as biomarkers to predict the low and high ovarian response to GnRH antagonist stimulation multiple-dose protocol in women under 45 years of age,followed by the basal level of FSH in poor ovarian response,and age in high ovarian response.The value of AFC (≤ 4.5 oocytes),level of AMH (≤ 0.95 ng/mL),basal level of FSH (≥10.15 mIU/mL),and the women’s age (≥31.5 years) can be considered as potential indicators of poor ovarian response.On the other hand,the value of AFC (≥14.5 oocytes),level of AMH (≥3.63 ng/mL),and the women’s age (≤ 27.5 years) are considered potential indicators of high ovarian response.
Conflict of interest statement
The authors have no relevant financial or non-financial interests to disclose.
Acknowledgments
The authors would like to express their gratitude’s to all doctors and clinical staff at Al Bassma Fertility Center in the Palestinian Territories.
Funding
This study received no extramural funding.
Authors’contributions
Mohammed M.Laqqan and Maged M.Yassin performed equal effort in the conceptualization,formal analysis,investigation,supervision,and visualization.Mohammed M.Laqqan performed the main effort in the data curation,methodology,and writing the original draft.On the other hand,Maged M.Yassin performed support in the data curation,methodology,writing,reviewing,and editing.
 Asian Pacific Journal of Reproduction2022年5期
Asian Pacific Journal of Reproduction2022年5期
- Asian Pacific Journal of Reproduction的其它文章
- Impact of gamete health on fertilization and embryo development: An overview
- An incidental presentation of Herlyn-Werner-Wunderlich syndrome with secondary infertility: A case report
- L-carnitine improves developmental competence of buffalo oocytes in vitro
- Evaluation of intratesticular chlorhexidine gluconate for chemical contraception in dogs
- Oxytocin improves testicular blood flow without enhancing the steroidogenic activity in Baladi goats
- Association of the microbial culture of follicular fluid,vaginal swab and catheter tip with β-hCG IVF positive and negative
