An ultrasound-guided percutaneous electrical nerve stimulation regimen devised using finite element modeling promotes functional recovery after median nerve transection
Xiao-Lei Chu , Xi-Zi Song , Yu-Ru Li, Zi-Ren Wu, Qi Li Qing-Wen Li, Xiao-Song Gu , Dong Ming
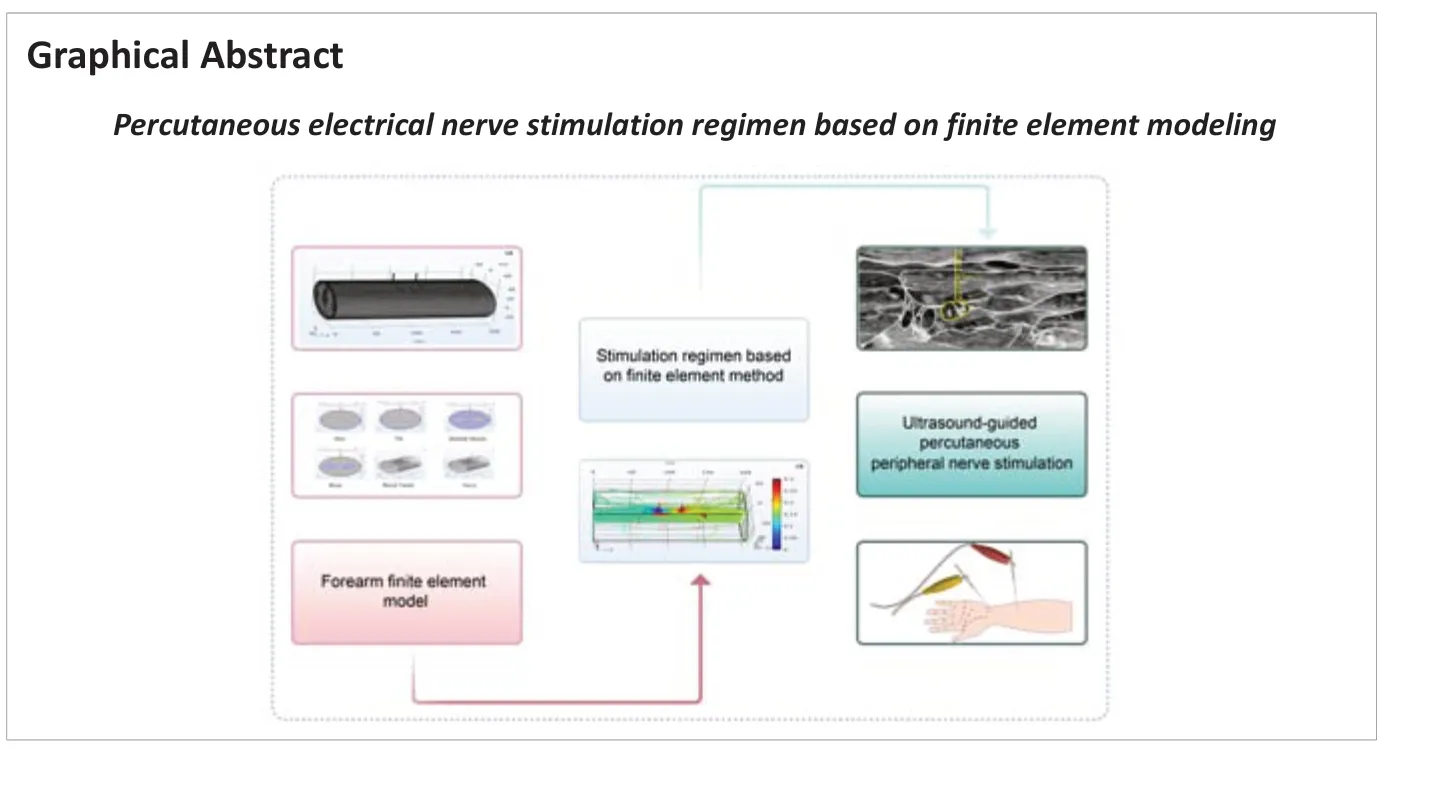
Abstract Percutaneous electrical nerve stimulation of an injured nerve can promote and accelerate peripheral nerve regeneration and improve function. When performing acupuncture and moxibustion, locating the injured nerve using ultrasound before percutaneous nerve stimulation can help prevent further injury to an already injured nerve. However, stimulation parameters have not been standardized. In this study, we constructed a multi-layer human forearm model using finite element modeling. Taking current density and activated function as optimization indicators, the optimal percutaneous nerve stimulation parameters were established. The optimal parameters were parallel placement located 3 cm apart with the injury site at the midpoint between the needles. To validate the efficacy of this regimen, we performed a randomized controlled trial in 23 patients with median nerve transection who underwent neurorrhaphy. Patients who received conventional rehabilitation combined with percutaneous electrical nerve stimulation experienced greater improvement in sensory function, motor function, and grip strength than those who received conventional rehabilitation combined with transcutaneous electrical nerve stimulation. These findings suggest that the percutaneous electrical nerve stimulation regimen established in this study can improve global median nerve function in patients with median nerve transection.
Key Words: finite element modeling; median nerve transection; nerve regeneration; neurorehabilitation; percutaneous electrical nerve stimulation; peripheral nerve injury; randomized controlled trial
Introduction 683 Methods 684 Results 685 Discussion 687
Introduction
The median nerve, also known as the ‘eye of the hand,’ is a mixed nerve that plays a crucial role in hand function. If damaged, the ability to abduct and oppose the thumb may be lost because of thenar muscle paralysis, which can result in severe hand dysfunction and impairment of activities of daily living (Robinson, 2000; Wang et al., 2019). Neurotmesis of the median nerve is more common at the forearm or wrist because it is located superficially in these areas. Neurotmesis is characterized by complete nerve transection and complete loss of function. Recovery cannot occur without surgical intervention. Even when surgery is performed, outcomes are generally poor.
Electrical stimulation is effective for accelerating nerve regeneration and functional recovery. Recent studies have demonstrated that low-intensity electrical stimulation of the proximal nerve stump can promote nerve regeneration (Gordon, 2016; Gordon and English, 2016; Choi et al., 2021; Wang et al., 2021) by increasing the expression of brain-derived neurotrophic factor (Kimura et al., 2019). It also promotes proliferation of Schwann cells and myelin formation during regeneration (Wan et al., 2010; Zhang et al., 2013). Promoting expression of genes associated with growth factors (Geremia et al., 2007) and neurotrophin signaling pathways (English et al., 2007) may also be therapeutic mechanisms that underly electrical stimulation.
Electrical stimulation is categorized according to stimulation depth as transcutaneous electrical nerve stimulation (TENS), percutaneous electrical nerve stimulation (PENS), and peripheral nerve stimulation. PENS is also known as subcutaneous electrical stimulation. In TENS, electrical stimulation electrodes are placed on the skin and electrical impulses are applied to stimulate nerve endings. PENS is performed by placing stimulation electrodes around peripheral nerves in the subcutaneous space. Low-frequency TENS immediately after injury improves peripheral nerve regeneration (Cavalcante Miranda de Assis et al., 2014). PENS has a greater therapeutic effect than TENS because of its higher precision and targeting; however, it is associated with higher incidence of complications and greater cost. PENS also provides stronger electrical stimulation than TENS but requires an operation for electrode implantation. In a study comparing four types of contacts in electrodes implanted in resected sciatic nerves, Yu et al. (2019) found that point contact had the same effect as whole-circle contact. We speculate that electroacupuncture, as a type of PENS, is a low-cost and valid therapy. Electroacupuncture is a widely studied therapy that combines the use of acupuncture points and needles that conduct electrical current to produce therapeutic effects. Peripheral nerve injury (PNI) can be treated using acupuncture (Fei et al., 2019; Zhang et al., 2019). However, electrical needles are often placed at points selected based on acupuncture meridians and collaterals. The reported incidence of acupuncture-induced nerve injury is 1.3%; therefore, the precision of needle placement can be improved (Melchart et al., 2004; Xu et al., 2013).
Ultrasonography is a non-invasive imaging technique used to measure skeletal muscle and nerve architecture in the upper and lower limbs (Romero-Morales et al., 2020; Schreiber et al., 2020). We believe that ultrasoundguided identification and location of nerves before PENS can help prevent acupuncture-induced nerve damage. Acquiring a consistent response to electrical needle stimulation can be difficult because differences in electrode placement, skin movement, and physiological variables produce different tissue conductance. Therefore, a feasible clinical regimen that can adapt to these differences is required to produce repeatable results. Gordon et al. (2010) reported that proximal nerve stimulation can promote nerve regeneration. Brushart et al. (2002) found that application of 20 Hz electrical stimulation to the proximal nerve for 1 hour can temporally compress staggered regeneration and that this stimulation synchronized distal stump reinnervation. Other studies (Koo et al., 2018; Zhang et al., 2018) have shown that stimulating electrodes placed both proximal and distal to the injury site can improve nerve regeneration and lead to better functional outcomes. At present, the optimal stimulation site in injured nerves is unknown. Moreover, most previous electrical stimulation studies have focused on the number of early regenerated nerves and general morphology rather than basic electrical theory. Therefore, several computer models have been developed to explore the effects of these variations and avoid exhaustive human testing. In one, the human lower leg has been constructed using a finite element model to simulate electrical recruitment of the tibial nerve and adjacent saphenous nerve fibers during percutaneous tibial nerve stimulation and to test feasibility of peripheral nerve stimulation in a human model (Elder and Yoo, 2018; Roointan et al., 2020).
In this study, we established a finite element model based on existing models and verified it using experimental data (Roointan et al., 2020). We also established an optimized stimulation regimen for median nerve neurotmesis based on our model and confirmed its efficacy in patients with PNI.
Methods
Design
The study was divided into two phases. In the first phase, a three-dimensional finite element model of the human forearm was constructed. In this model, electrical properties were assigned to each tissue and electrode. The model was used to predict current density and activation function throughout the entire median nerve. Then, electrical simulation was performed to explore a PENS regimen including electrode location, angle, and distance. In the second phase, the efficacy of the regimen was validated using randomized parallelgroup controlled trial data.
Finite element model establishment
A three-dimensional forearm model was created using COMSOL Multiphysics® finite element software version 5.3a (COMSOL AB, Stockholm, Sweden). The length of the three-dimensional forearm model was 20 cm along the longitudinal axis (Figure 1
). Based on gross dissections, we modeled the median nerve as a single nerve with a diameter of 2 mm. The geometry of the human forearm was modeled as concentric cylinders for the skin (3 mm), fat (10 mm), muscle (25 mm), bone (2 cm), and blood vessels (3 mm) as shown inFigure 2
(Roointan et al., 2020). The corresponding tissue layer was described by the conductivity σ and the relative permittivity ε. σ and ε for each component of the model were designed according to Gabriel et al. (1996). Tissue material constants are shown inTable 1
.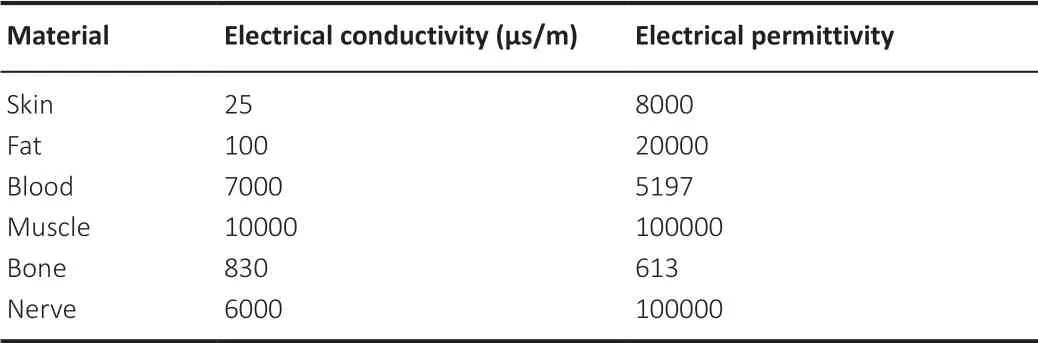
Table 1 |Tissue material constants
PENS was modeled using two uninsulated stainless steel needle electrodes (cylinder, diameter = 0.3 mm, length = 40 mm). Simulations were run under conditions of constant current (0.3 V). The selected frequency was 20 Hz, which is thought to promote nerve regeneration (Gordon et al., 2009; Park et al., 2019). PENS was simulated by changing the position of the electrodes, leaving all other model parameters unchanged. Next, a finite element model was constructed to calculate current density and active function of the corresponding nerve fibers. The current density represents the current per unit section area. The second derivative of biological tissue’s electrical potential along the nerve fiber axis under the action of electrical stimulation was called active function, which can characterize the effect of an electric field on peripheral nerve electrical activity (McNeal, 1976; Rattay and Aberham, 1993). When neurons depolarize and become excited, the active function is positive; when neurons hyperpolarize and become inhibited, the excitation function is negative. To calculate the best electrode location, we set three lines in the model: center line of nerve, forearm line of nerve, and line between two needles (Figure 2
). The current density and active function values on the center line of nerve were calculated at different positions, distances, and angles. Finally, the optimal treatment regimen was determined by comparing the ratio of the current density and active function on the line between two needles to the forearm line of nerve.Clinical trial
This study was approved by the Human Research Ethics Committee of Tianjin Hospital (approval No. 2020-053) and registered in the Chinese Clinical Trial Registry (registration No. ChiCTR2000030790) on August 12, 2020 (Additional file 1
). All patients provided written informed consent (Additional file
2
). Consolidated Standards of Reporting Trials guidelines were followed (Additional file 3
).Patients aged 10 to 70 years who were diagnosed with complete median nerve neurotmesis and underwent neurorrhaphy at Tianjin Hospital from September 1, 2020 to January 1, 2021 were eligible. Inclusion criteria were as follows: 1) complete median nerve transection based on observation in surgery (the surgeon was a hand surgeon from Tianjin Hospital with rich experience in neurosurgery), 2) stable vital signs, 3) disease course < 2 months, 4) no previous electrical stimulation treatment, and 5) no metal allergy or intolerance to electroacupuncture stimulation. We excluded patients with heart disease, hypertension, tuberculosis, asthma, hepatitis, nephritis, serious metabolic disease (hyperthyroidism, hypothyroidism, scurvy or edema), and unstable upper extremity fracture. Patients taking drugs affecting metabolism and those with acute fever, diarrhea, or other acute disease were also excluded. Patients were able to voluntarily withdraw from the trial at any time.
Based on published data (Gordon et al., 2010), a sample size of 20 patients was enough to prove a treatment effect. To account for patients lost to follow-up, we recruited 30 subjects and randomly assigned them to the PENS (n
= 15) or TENS group (n
= 15) using the random number table method. Patient numbers were arranged in the order of inclusion and grouping was determined. Odd number cards and their corresponding patient names were put into the envelope of the experimental group; even number cards and their corresponding patient names were put into the envelope of the control group. The details of grouping were sealed in opaque envelopes by an independent researcher. This researcher was blinded to group allocation. Three patients in the experimental group and four in the control group voluntarily withdrew during the study. Finally, 23 participants (8 women and 15 men) were included in the analysis.Interventions
Patients in the TENS group received conventional rehabilitation treatment and TENS; those in the PENS group received conventional rehabilitation treatment and PENS. Conventional rehabilitation treatment included: 1) movement training: passive and active extension/flexion of fingers, elbows, and shoulders (aiming to prevent joint ankylosis and muscle atrophy); 2) manipulative therapy (aiming to reduce muscle cramps, eliminate local swelling, release adhesions, and relieve clinical symptoms); 3) occupational therapy; and 4) sensory training, including cold and hot sensory training, two-point discrimination training, and positioning training. Patients received conventional rehabilitation once a day for 1 hour, four times a week, for 5 consecutive weeks.
For patients in the PENS group, first, the site of median nerve recruitment was located and the distance from skin to nerve measured using ultrasonography (SonoScape-X5; Shenzhen SonoScape Bio-Medical Technology Co., Ltd., Shenzhen, Guangdong Province, China) (Figure 3
). Then two disposable sterilized stainless-steel acupuncture needles (0.3 mm × 40 mm; Beijing Keyuanda Medical Device Manufactory, Beijing, China) were used to administer electrical stimulation with the SDZ-III acupuncture instrument (Hwato, Suzhou, China). Stimulation parameters were as follows: discontinuous wave, frequency 20 Hz, width 0.2 ms. PENS was administered once a day for 1 hour, four times a week, for 5 consecutive weeks (Figure 4
).For those in the TENS group, the neurotmesis site was located at the midpoint between electrode patches (5 cm × 5 cm; Hwato, Suzhou, China); the distance between patches was 3 cm. Then, electrical stimulation was administered using the SDZ-III acupuncture instrument (Hwato, Suzhou, China). Stimulation parameters were as follows: discontinuous wave, frequency 20 Hz, and width 0.2 ms. PENS was administered four times per week in 1-hour sessions for 5 consecutive weeks (Figure 5
). None of the patients in the study experienced unintended effects or harm from PENS or TENS.Outcome measurements
Motor function assessment
The British Medical Research Council (BMRC) score is widely used to assess sensory and motor function after PNI (Lundborg et al., 2004) and considered the most effective method for evaluating the function of a single nerve innervating both proximal and distal muscles (Shen and Zhu, 1996). Motor function is graded from M0 to M5. A higher grade indicates a better level of functioning. Recovery above grade M3 was considered good. However, the BMRC score is highly subjective and the grading is rough. Grip strength can also be measured as an indicator of median nerve injury rehabilitation (Wachter et al., 2018b) and was the primary outcome measure in this study. Grip strength was measured before and after treatment using a hydraulic hand dynamometer (Baseline® HiResER, NY, USA). Because of individual differences between patients, grip strength is expressed as relative grip strength (grip strength/body weight) to reduce individualization.
Sensory function assessment
The median nerve provides sensory innervation to the radial portion of the palm, thumb and index finger, and half of the middle and ring fingers (Soldado et al., 2016). Sensory dysfunction is common in patients with PNI. Sensory function was assessed using the BMRC score, which grades it from S0 to S4 (Shen and Zhu, 1996). Recovery above grade S2 was considered good. Grade was assigned to deep and superficial sensation and allodynia. Higher grade indicates higher level of functioning.
Global function
The functional median nerve subscore of the Chinese Society of Hand Surgery upper limb functional assessment was used to assess median nerve function (Pan et al., 2000). This scale does not require any special equipment, is easy to apply, and provides accurate and objective results. Four indicators are evaluated: strength of wrist and finger flexors and thumb opposition as well as sensory function. Each indicator is graded on a four-point scale; therefore, the minimum and maximum scores are 0 and 16, respectively. Higher score indicates better median nerve function.
The Disabilities of Arm, Shoulder, and Hand (DASH) score was also used to assess upper limb function and disability (Hudak et al., 1996). This score is based on a self-reported questionnaire and divided into two parts: activities of daily living and the effect of upper limb symptoms on sleep and selfsatisfaction. Each item is rated on a five-point scale, 30 items in total. Total DASH score = (scale score ‒ 30)/1.2. Higher scores indicate worse functioning.Patient functional assessment was performed before the first treatment (visit 1) and after the last treatment (visit 20) and the scores recorded. To avoid subjective errors, patients were examined by the same physiatrist (YRL or ZRW).
Statistical analysis
Statistical analyses were conducted using SPSS software version 22.0 (IBM Corp., Armonk, NY, USA). Intergroup comparisons were performed using the independent-samplet
-test. Intragroup comparisons were performed using the paired-samplet
-test. Data are expressed as means ± standard deviation (SD). The Wilcoxon signed-rank test was used to compare categorical variables. BMRC score was compared using the Wilcoxon signed-rank test.P
< 0.05 was considered significant.Results
Finite element model results
Location of needles
Using the finite element model, we compared stimulation with both electrodes proximal to the injury site with stimulation using one electrode proximal to the injury site and the other electrode distal (Figure 6A
andB
). The latter caused a 131.54% increase in current density and higher nerve activation (Figure 6C
); therefore, stimulation using one electrode proximal to the injury site and the other distal was considered superior.Distance between needles
Next, we examined the optimal distance between needles (1‒12 cm). Current density gradually declined with increased distance (Figure 6D
). The current density increased considerably when the distance was 1 to 3 cm. Active function peaked at distances between 3 and 5 cm (Figure 6E
). Current density distribution was then examined with the electrodes at different distances. As shown inFigure 7
, a 3 cm distance resulted in a moderate current density. When considering the current density results alone, 3 cm was the better distance. To further validate these results, current distribution at different distances was simulated using the finite element model (Figure 8
). We found that the current was parallel to the nerve when the distance was 3 cm. Combining the current density and active function data, we concluded that 3 cm was the optimal distance between needles and that the nerve injury site should be located at the midpoint between the needles.Angle between the needles
Current density was relatively large when the angle between the needles was 0°, 15°, 30°, 45°, and 90°(Figure 9A
). Nevertheless, active function was higher when the angle was 0°, 60°, 75°, and 90° (Figure 9B
). 0° and 90° were considered the point of intersection of the two parameters. A current density distribution map is shown inFigure 10
. Greater current flow parallel to the nerve resulted in stronger nerve activity. It was difficult to accept 90° because inserting needles at this angle would cause severe pain. Ultimately, 0° was considered the best angle.Therefore, we concluded that the optimal needle parameters for PENS were parallel placement located 3 cm apart with the injury site at the midpoint between the needles. These parameters were used in the clinical trial portion of the study.
Results of clinical trial
Baseline characteristics
There were no significant differences in baseline data between the PENS and TENS groups (Table 2
). The study flow chart is shown inFigure 11
.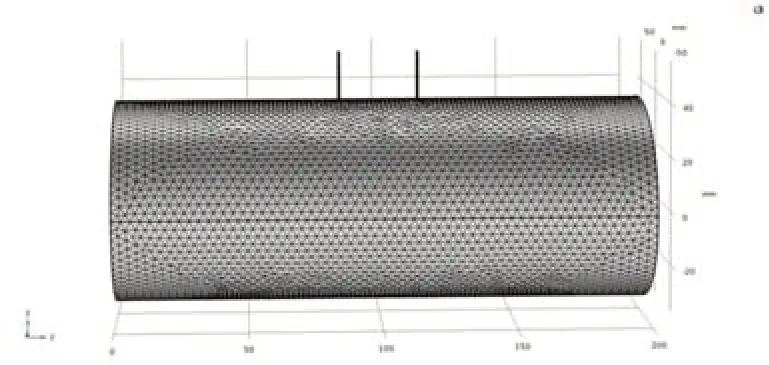
Figure 1 |Three-dimensional forearm model created using COMSOL Multiphysics® finite element software version 5.3 (COMSOL AB, Stockholm, Sweden).
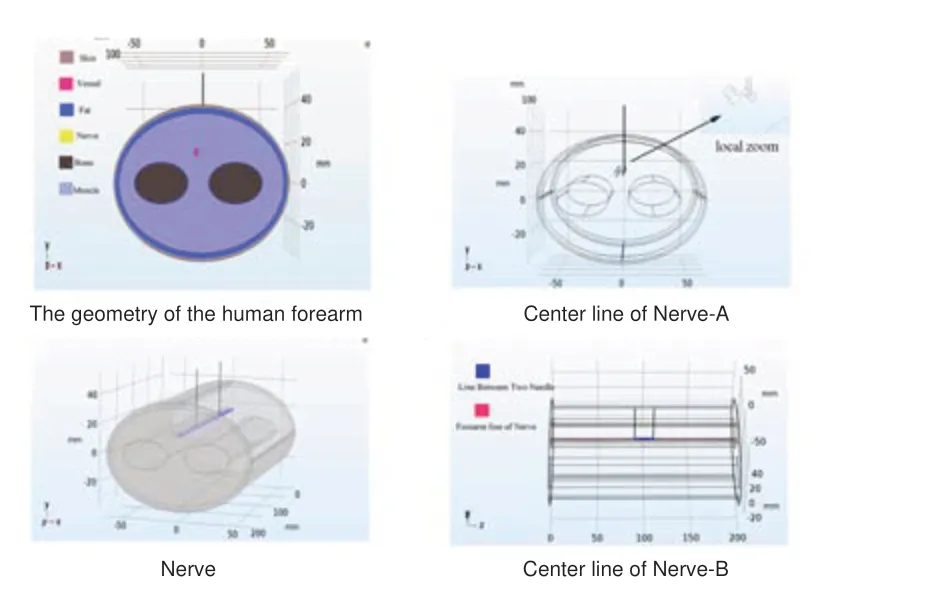
Figure 2 |Geometry of the human forearm model.Cross-sectional (A) and three-dimensional (B) geometry of the human forearm. In (A), forearm tissues are represented as shown in the key. In (B), the nerve is blue. (C) The red line represents the center line of nerve. (D) The red line represents the forearm line of nerve and the blue line represents the line between two needles.

Figure 3 |An ultrasonographic image.The dotted green line is a cross-section of the median nerve. The dotted red line represents the distance from skin to nerve. An individualized depth plan was developed for each patient.

Figure 4 |Percutaneous nerve stimulation.

Figure 5 |Transcutaneous electrical nerve stimulation.

Figure 6 |Locations and distance of the needles under finite element analysis.(A) Both electrical needles were placed proximal to the nerve injury site. The black arrows represent needle electrodes, the black segment represents the nerve, and the red segment represents the injury site. (B) One electrical needle is placed proximal to the injury site and the other distal. (C) Current density and action function ratios at different locations. (D) Current density ratio at different needle distances. (E) Active function ratio at different needle distances.

Figure 7 |Current density distribution with the electrodes at different distances.Current density distribution with interelectrode distances of 1 cm (A), 2 cm (B), 3 cm (C), and 4 cm (D). On the x-axis, the site of median nerve injury was plotted at 100. With distances of 1 cm and 2 cm, the current at the injury site was relatively high. With a 3 cm distance, current density was moderate. Current density was relatively low at 4 cm.
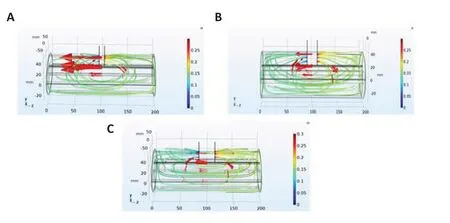
Figure 8 |Current distributions at 1 (A), 2 (B) and 3 (C) cm inter-needle distances.The curves represent the electric field lines at different needle distances in the forearm model; the arrows indicate the direction of current. The figure C shows that smaller arrows indicate decreased current density. However, arrow number and depth increase. Besides, it has more homogeneous distribution of current and more electric field lines parallel to the nerve compared with the A and B.
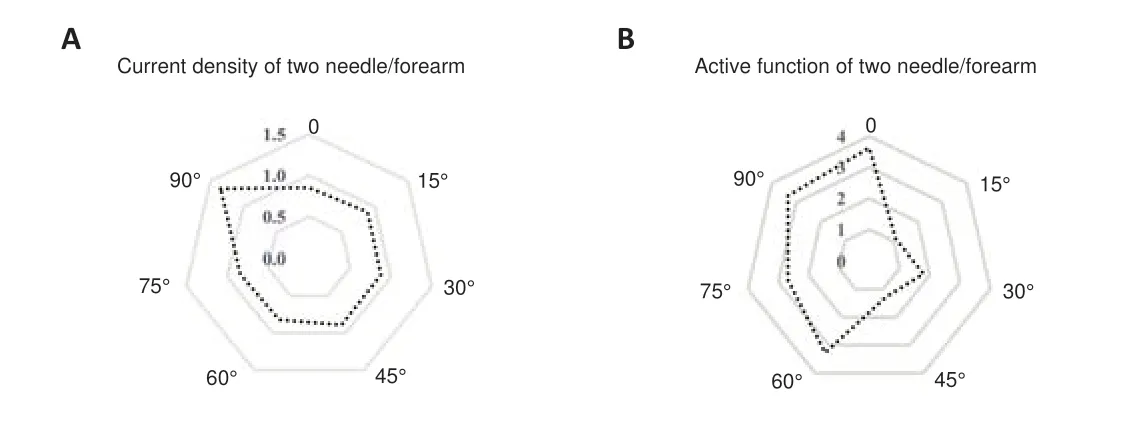
Figure 9 |Changes in current density and active function at different angles between the two needles.(A) The current density was relatively high when the angle between the two needles was 0°, 15°, 30°, 45°, and 90°. (B) The active function was relatively high when the angle was 0°, 60°, 75°, and 90°.
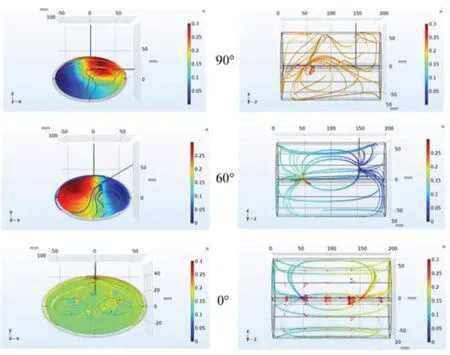
Figure 10 |Current density distribution diagram.The left panels indicate cross-sectional current distribution within the nerve at the midpoint between the two needles. Red indicates higher current density and blue indicates lower. The right panels indicate field line and current direction at different angles. When the angle between the two needles was 0°, the current distribution was more uniform and most of the electric field lines ran parallel to the nerve.
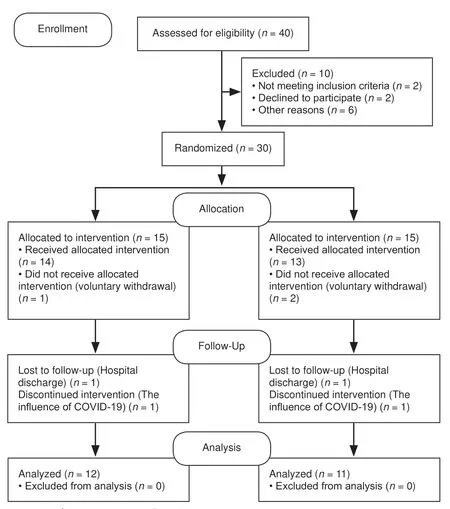
Figure 11 |CONSORT 2010 flow diagram.
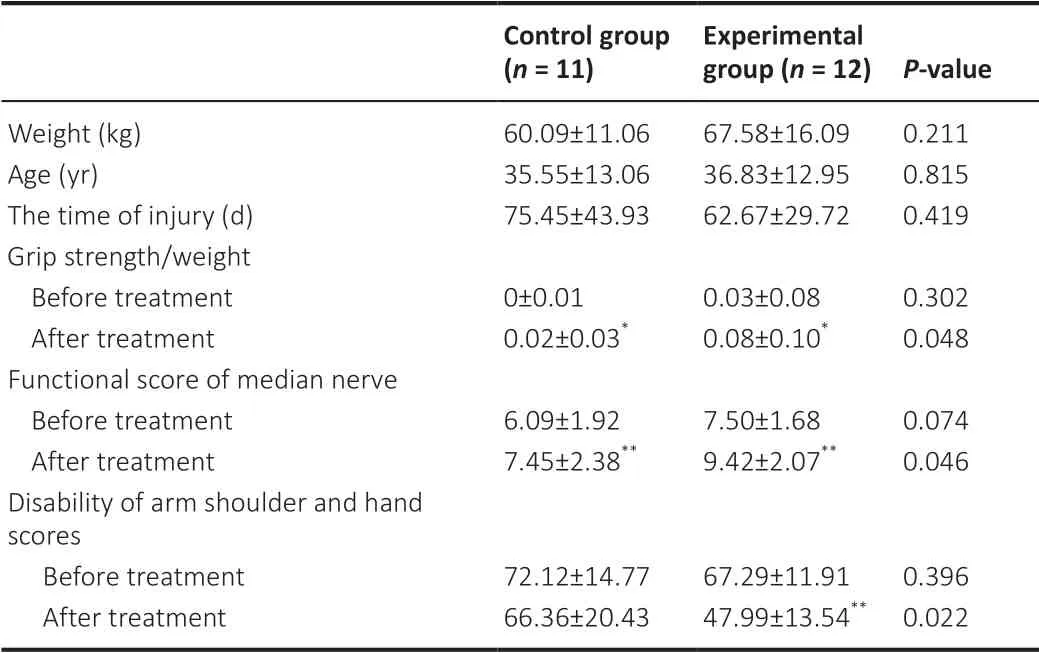
Table 2 |Characteristics of patients with complete median nerve neurotmesis
Global function
DASH score
The DASH score in the PENS group significantly decreased by 29% after treatment. However, it did not significantly decrease in the TENS group. DASH score after treatment was significantly lower in the PENS group, indicating that patients in this group acquired greater upper limb function (P
< 0.01;Table 2
).Functional score of the median nerve
The functional score of the median nerve significantly increased after treatment in the PENS and TENS groups (bothP
< 0.01). However, the functional score of the median nerve in the PENS group was significantly higher (P
< 0.05;Table 2
).Sensory function assessment
After treatment, 12 patients in the PENS group and seven in the TENS group showed sensory function grade S2 or higher. Sensory function improved in each group after treatment. The degree of improvement was greater in the PENS group (P
< 0.05;Table 3
).
Table 3 |Number of patients with complete median nerve neurotmesis after treatment with different British Medical Research Council sensory evaluation indices
Motor function assessment
After treatment,10 patients in the PENS group and three in the TENS group showed motor function grade M3 or higher. Motor function improved in each group after treatment. The degree of improvement was greater in the PENS group (P
< 0.05;Table 4
).
Table 4 |Number of patients with complete median nerve neurotmesis after treatment with different British Medical Research Council motor evaluation indices
Grip strength improved significantly after treatment in each group (P
< 0.05). However, the degree of strength improvement was greater in the PENS group (P
< 0.05;Table 2
).Discussion
PNI represents 2% of all extremity trauma and can result in long-term physical and functional disability (Robinson, 2000; Wang et al., 2019). The median nerve is the most commonly injured nerve (Mansiz-Kaplan et al., 2020). Electrical stimulation is an effective treatment (Fei et al., 2019; Wang et al., 2019). Selection of points to administer stimulation is generally based on traditional Chinese medicine. Stimulation parameters should be selected to optimize treatment effects. Therefore, we created a three-dimensional anatomical finite element model of the forearm in which electrical properties were assigned to component tissues and electrodes. Then, PENS was simulated to explore variations in electrode location, distance, and angle. Our modeling results suggested that placement of one electrode proximal to the injury site and another distal promotes neural excitation and exerts a greater stimulatory effect.
If the distance between the two needles is small, the injured nerve can easily experience a high short-circuit current. However, if the distance is large, the nerve may not recover from injury because the electric current is too low.
Our finite model indicated that a needle distance of 3 cm can achieve best therapeutic effect. Moreover, several studies have reported that a parallel field is more sensitive than an orthogonal field (Roth and Basser, 1990; Ju et al., 2020), which may be the reason a 0° angle between needles results in optimal active function. Finally, our finite model simulations suggested that the optimal needle parameters for PENS were parallel placement located 3 cm apart with the injury site at the midpoint between the needles.
In the clinical trial phase of the study, we compared treatment effects of PENS and TENS in patients who underwent neurorrhaphy after median nerve transection. Compared with the TENS group, grip was significantly stronger in the PENS group after treatment. Therefore, PENS using stimulation parameters determined using a finite element model restored motor function to a greater degree than TENS. Both motor and sensory recovery as measured by their respective BMRC scores was also better in the PENS group. These results are similar to those reported in a previous study (Koetsier et al., 2020). However, BMRC assessments lack precision. The functional median nerve subscore was used to validate these results. The functional score includes measures of motor and sensory function as well as thumb and finger movement. The functional score findings were consistent with those obtained using the BMRC score: improvement was better in the PENS group.
We believe that PENS promotes not only medial nerve regeneration but also functional recovery. Outcome analysis after PNI in previous studies usually included only measures of nerve impairment such as sensory and motor function. Few studies have evaluated functional outcome or health-related quality of life. Therefore, we used the DASH score to evaluate upper limb function. The degree of improvement in upper limb function was greater in the PENS group than in the TENS group. These results are consistent with those in previous studies (Gordon, 2016; Tang et al., 2016). Therefore, we believe that the PENS regimen used in this study can reduce disability and improve function of median nerve-innervated muscles in patients with median nerve injury. However, the degree of improvement in forearm function was not significant after treatment compared with before treatment. We speculate that this may be related to weaker stimulation effects. Philip et al. (2020) found that patients with PNI report considerable disability and that pain is the strongest predictor of DASH score. As DASH score in patients with PNI can be predicted by higher pain and disability, we believe PENS can be used to alleviate neuropathic pain and reduce DASH score.
Previous studies were reported mainly from the viewpoint of physiology. Our study reported outcomes in the context of electrical stimulation. Our PENS regimen, in which electrical needles are parallel and located at both ends of the injured nerve at a distance of 3 cm, creates an electric field parallel to the nerve and maximizes current density and active function. Ultimately, this may help optimize treatment effects in patients with median nerve injury. Furthermore, PENS can transmit electricity subcutaneously through the skin and onward, is low-cost, and does not require electrode implantation.
In our future research, we plan to expand the sample size and observe longterm effects of the established percutaneous electrical nerve stimulation regimen. Additionally, we will investigate our PENS regimen in patients with other types of PNI. In conclusion, we have presented a PENS regimen for median nerve transection that was developed using element finite modeling and shown to be effective in a small clinical trial. We believe this regimen has potential for widespread clinical use pending confirmation in large-scale studies.
Acknowledgments:
We express our sincere thanks to Shuai Wang, Yu-Song Han, Si-Yao Li, Jia-Xin Li and Shi-Yi Zhang for their help during the course of the experiment in Tianjin Hospital.
Author contributions:
Study conception and design: YRL, ZRW, QL, QWL; manuscript draft: XLC, XZS; manuscript revision: DM, XSG. All authors read and approved the final manuscript.
Conflicts of interest:
All authors claim that there are no conflicts of interest.Editor note: XSG is an Editorial Board member of Neural Regeneration Research. He was blinded from reviewing or making decisions on the manuscript. The article was subject to the journal’s standard procedures, with peer review handled independently of this Editorial Board member and their research groups.
Author statement:
This paper has been posted as a preprint on Research Square with doi: 10.21203/rs.3.rs-1063940/v1, which is available from: https://assets.researchsquare.com/files/rs-1063940/v1/4e39801b-4c69-435a-857f-f1f4a79ca3f2.pdf?c=1637005527.
Availability of data and materials:
All data generated or analyzed during this study are included in this published article and its supplementary information files.
Open access statement:
This is an open access journal, and articles are distributed under the terms of the Creative Commons AttributionNonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
Open peer reviewer:
Standiford Helm, University of California, Irvine, USA.
Additional files:
Ethics Approval (Chinese).
Informed Consent Form (Chinese).
CONSORT checklist.
Open peer review report 1.
- 中国神经再生研究(英文版)的其它文章
- Inflammation and retinal degenerative diseases
- Synaptic alterations as a common phase in neurological and neurodevelopmental diseases: JNK is a key mediator in synaptic changes
- Brain-derived neurotrophic factor in main neurodegenerative diseases
- The best of both worlds: mastering nerve regeneration combining biological and nanotechnological tools
- Exosomal miR-23b from bone marrow mesenchymal stem cells alleviates oxidative stress and pyroptosis after intracerebral hemorrhage
- Chlorogenic acid alleviates hypoxic-ischemic brain injury in neonatal mice

