Prognostic significance of peritoneal metastasis from colorectal cancer treated with first-line triplet chemotherapy
INTRODUCTION
Globally,colorectal cancer(CRC)is the third most-common cancer and the second-most-common cause of cancer death in males and third in females[1].There has been a significant improvement in overall survival(OS)for patients with metastatic CRC secondary to the introduction of several new chemotherapy and targeted agents[2-5].Although no major improvement in survival was observed with first-line doublet chemotherapy regimens compared to single-agent regimens[6-8],triplet chemotherapy apparently resulted in improved OS compared to doublets in the first-line setting[9-12].
The boy made one of those hand signs at me as I was about to leave. I asked his sister if your brother is so smart then why is he doing things like that with his hands? She told me that he was saying that he loved me with his hands. I didn t say anything back to her at all because I didn t believe her. People can t talk with their hands and everybody knows that. People can only talk with their mouth.
Several studies have shown that patients with peritoneal carcinomatosis in metastatic CRC have poor survival,and this was an independent poor prognostic factor[13,14].However,the majority of those studies used either single-agent or doublet chemotherapy with or without targeted therapy[13,14].It is unclear whether peritoneal carcinomatosis continues to be a poor prognostic factor in patients with metastatic CRC treated with triplet regimens.
So holidays in here are the worst-at least I thought hey were until I realized a few things. Once I stripped away all the commercialism and hype, I saw what holidays were all about. They re elaborate excuses we use to take a look at our lives, our successes and failures, and to spend quality time with our loved ones.
The power of one man or one woman doing the right thing for the right reason, and at the right time, is the greatest influence in our society. Individually, we may not be captains of our teams, but we are always captains of our own souls and collectively the soul of America. The soul of America rests in our hands, as we seek reconciliation21 and racial healing in America at the dawn of this exciting new century.
We have previously reported the results of our phase I/II trial of triplet chemotherapy using capecitabine,oxaliplatin,and irinotecan with bevacizumab in patients with advanced CRC[15].Here,we report the post hoc analysis of the efficacy of the above combination in patients with and without peritoneal metastasis and examined the different prognostic factors for progression-free survival(PFS)and OS in these groups of patients.
MATERIALS AND METHODS
Study design
Treatment of patients with metastatic CRC should be personalized based on prognostic clinical and molecular factors.The benefit of triplet chemotherapy might outweigh the excess toxicity in certain subgroups,such as those with peritoneal carcinomatosis.
Patients
Patients with metastatic CRC not amenable to surgical resection were enrolled in a phase I/II trial of triplet chemotherapy consisting of capecitabine,oxaliplatin,irinotecan,and bevacizumab.The study procedures have been published earlier[15].Briefly,patients were eligible for inclusion if they were more than 18 years old,had histologically confirmed CRC adenocarcinoma with no prior chemotherapy or targeted therapy for metastatic disease,had Eastern Cooperative Oncology Group performance status 0-2,had measurable disease[defined by response evaluation criteria in solid tumors(RECIST)V1.1][16],and had adequate organ function(defined as absolute neutrophil count ≥ 1.5 × 10/L,platelet count ≥ 100 × 10/L,normal serum bilirubin,serum transaminases ≤ 2.5 times the upper limits of normal,normal serum creatinine,and urine dipstick for proteinuria ≤ 2 +).Patients who had prior adjuvant oxaliplatin or fluoropyrimidine chemotherapy were eligible if the last chemotherapy was ≥ 12 mo.Exclusion criteria included central nervous system metastasis,severe cardiovascular dysfunction,prior malignancy within 5 years(except for adequately treated nonmelanoma skin cancer or in situ cervical cancer),active infection,bleeding diathesis,major surgery within 28 d of starting therapy,uncontrolled hypertension,prior history of dihydropyrimidine deficiency,and pregnancy or breastfeeding.The study was approved by the institutional review board under the number RAC2081068 and was listed on clinical trials.gov(NCT01311050).All patient signed informed consent.
Treatment
The phase I part of the trial has been described earlier in a previous publication[15].According to phase I,the recommended doses for phase II were capecitabine 1000 mg/morally on days 1 to 14,oxaliplatin 130 mg/m,irinotecan 150 mg/m,and bevacizumab at 7.5 mg/kg of body weight,all on day 1 of each cycle.Treatment cycles were repeated every 21 d.Patients were given 5-8 cycles of a triplet regimen with bevacizumab.Responding patients were placed on maintenance capecitabine and bevacizumab at the above doses until disease progression or unacceptable toxicity.
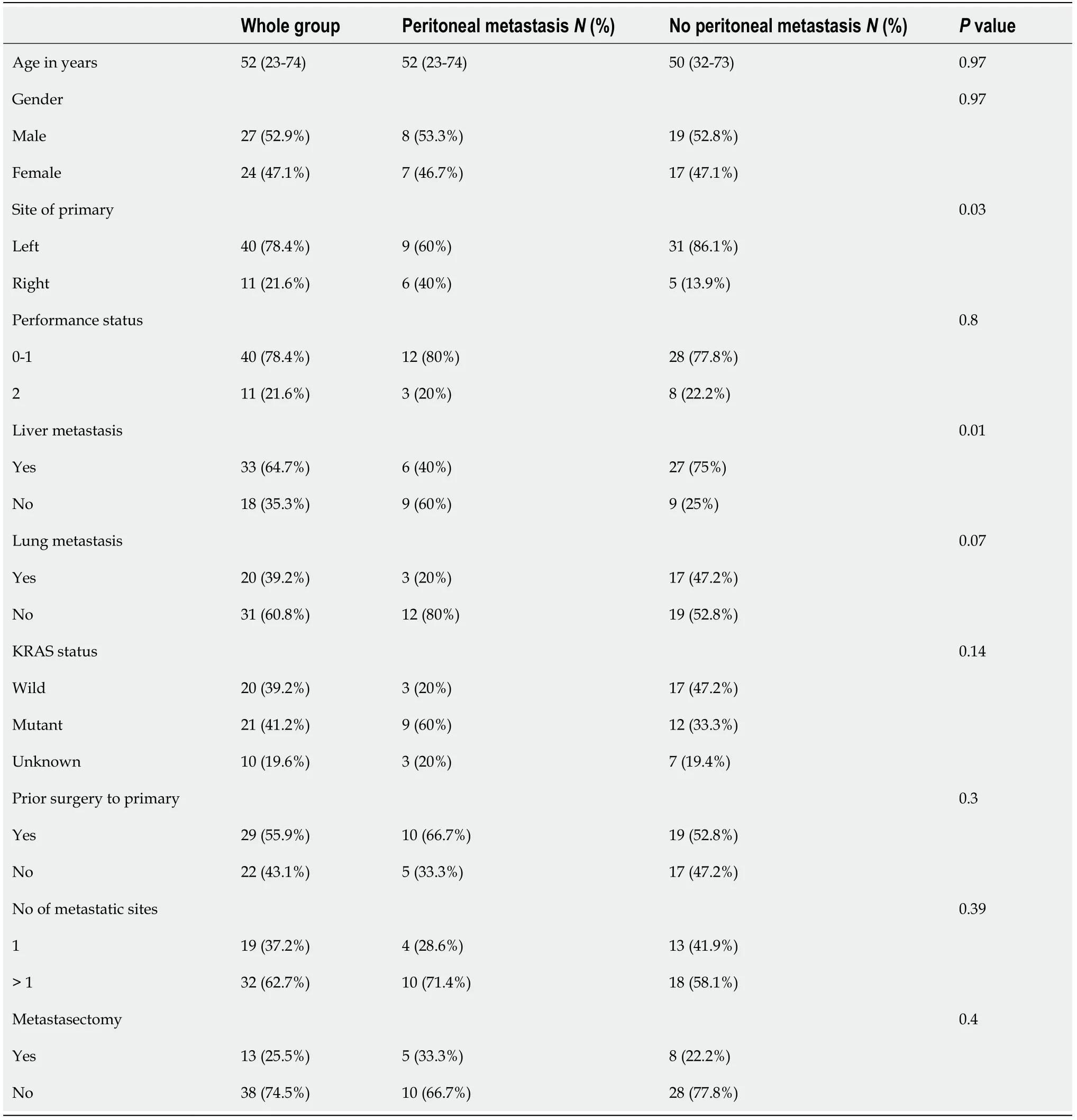
The presence of other site involvement in patients with CRC peritoneal metastasis has been examined by Franko[14].A total of 10553 patients treated with systemic therapy in prospective randomized trials were reported by the ARCAD database.Of those,9178(87%)had nonperitoneal metastasis,194(2%)had isolated peritoneal metastasis,and 1181(11%)had peritoneal and other organ metastases.Survival was better in the nonperitoneal metastasis group(adjusted HR 0.75,95%CI: 0.63-0.91,= 0.003).Patients with peritoneal metastasis and one other site had similar survival to those with isolated peritoneal metastasis(adjusted HR 1.10,95%CI: 0.89-1.37,= 0.37).Two of 14 trials reported in the above pooled analysis used triplet regimens as an investigational arm;however,none of them reported a subgroup analysis based on peritoneal metastasis[11,25].In our study,the patients with peritoneal metastasis had a higher percentage of more than 1 metastatic site involvement(71.4%)than the nonperitoneal metastasis group(58.1%),a difference that was not statistically significant(= 0.39).
Statistics and efficacy endpoints
The statistical design of the phase I and II parts of this study was described earlier[15].The number of patients planned for the phase II part of the trial was 46.All patients were assessed for response according to RECIST criteria V1.1 by computed tomography scans or magnetic resonance imaging performed after the second,fifth,and eighth cycles of chemotherapy and every 2 mo thereafter.
Patient characteristics were summarized using frequencies with percentages,while continuous variables were summarized using medians with interquartile ranges.Patient characteristics were further retrospectively compared according to the presence or absence of peritoneal metastasis.Categorical variables were compared using the chi-square test,while continuous variables were compared using the Mann-Whitney test.
Our study has several limitations,firstly the retrospective nature of the study.Additionally,the small number of patients included makes interpretations of the data difficult.On the other hand,our patient cohort was treated in a prospective phase I/II study with a uniform treatment plan.
RESULTS
A total of 53 patients with metastatic or locally advanced unresectable CRC were enrolled in a phase I/II trial of combination chemotherapy with capecitabine,oxaliplatin,irinotecan,and bevacizumab(6 in the phase I part and 47 in the phase II part).Among those,two withdrew.Therefore,a total of 51 patients were available for evaluation.Patient characteristics are illustrated in Table 1.Fifteen patients(29.4%)had peritoneal metastasis.Forty(78.4%)had left-sided colon cancer.Thirty-three(64.7%)had liver metastasis;20(39.2%)had lung metastasis,and 32(62.7%)patients had more than one site of metastasis.
The characteristics of patients with peritoneal metastasisno peritoneal metastasis are illustrated in Table 1.Of note,31(86%)patients with no peritoneal metastasis had left-sided primary tumors,while only 9(60%)patients in the peritoneal metastasis group had left-sided primary tumors(= 0.03).Additionally,25(75%)of the patients with no peritoneal disease had liver metastasis,while only 6(40%)of the patients with peritoneal metastasis had liver metastasis(= 0.01).
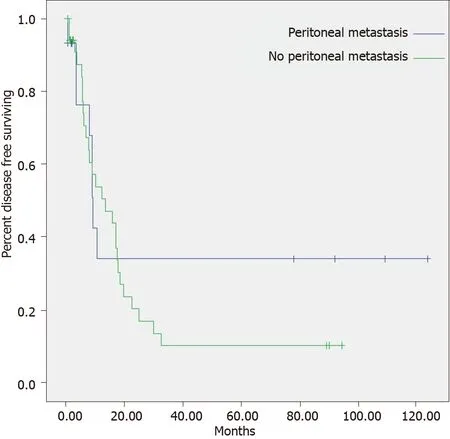
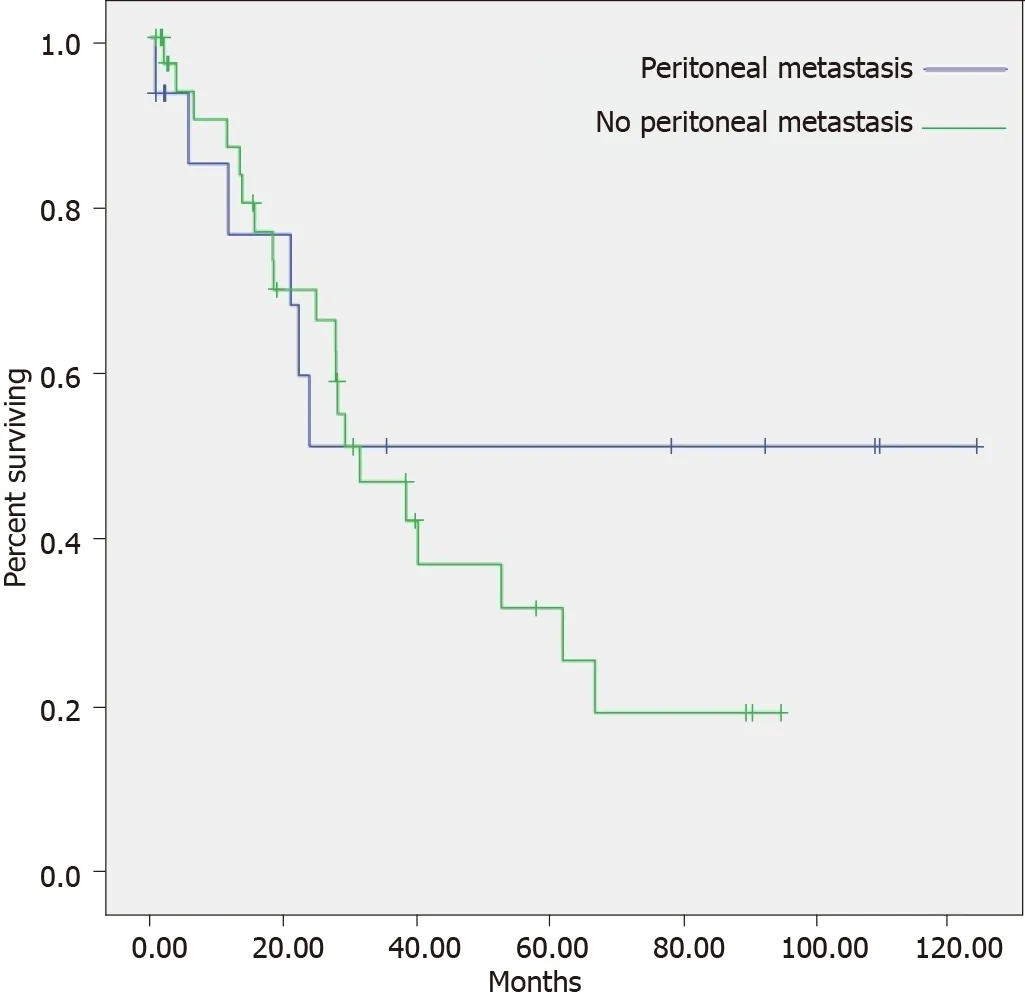
The median PFS and OS for the whole group were 10.8 mo[95% confidence interval(CI): 5.1-16.5]and 31.3 mo(95%CI: 16.9-45.6),respectively.The median PFS for the peritoneal metastasis groupthe group without peritoneal metastasis was 9.4(95%CI: 8.6-10.1)mo13.7(95%CI: 4.4-22.9)mo(= 0.401).The median OS for the group with peritoneal metastasisthe group without peritoneal metastasis was not reached31.3(95%CI: 19.5-43.1)mo(= 0.368)(Figures 1 and 2).
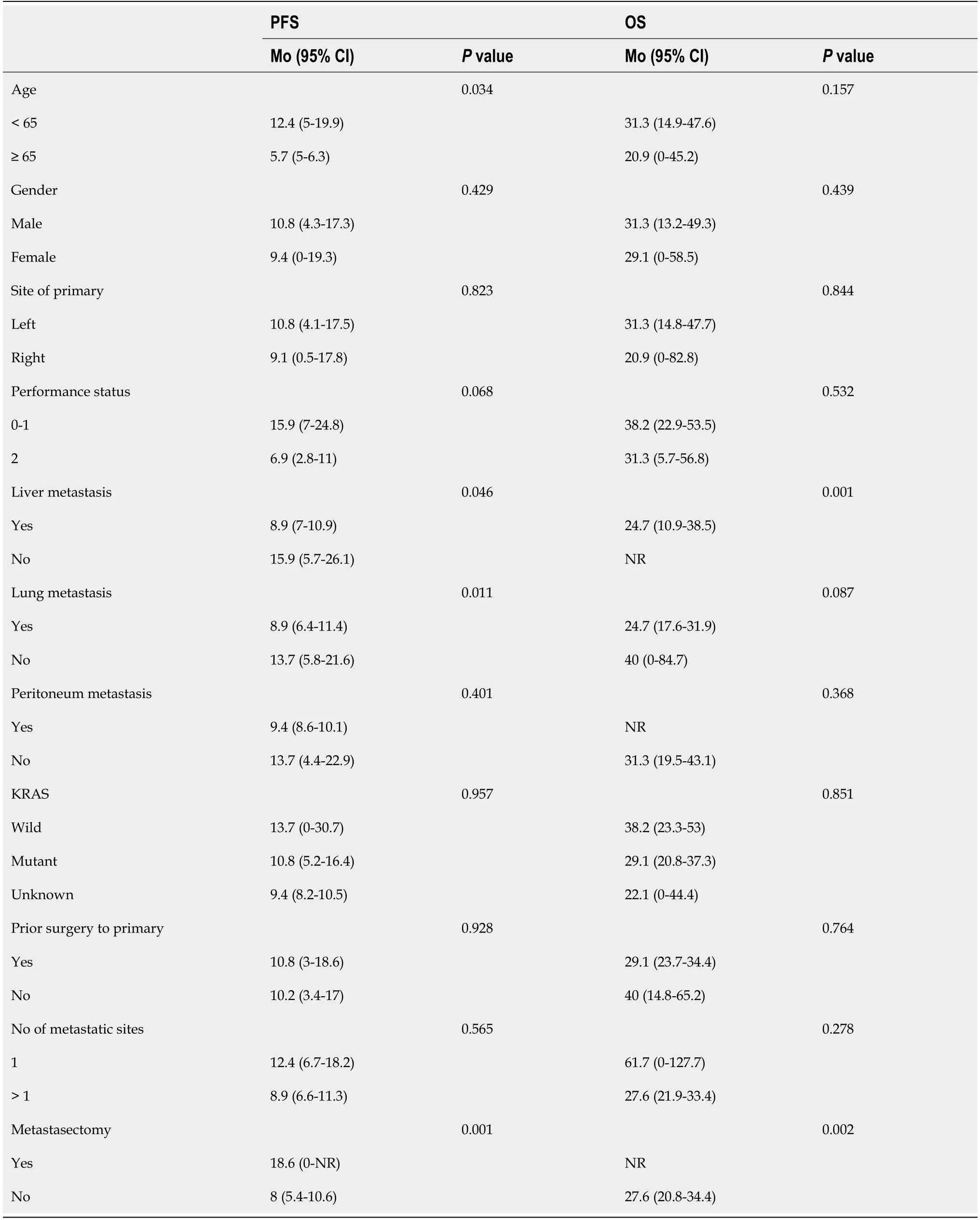
Univariate analysis of known prognostic factors is shown in Table 2.Age(less than 65 years),presence of liver/lung metastasis,and metastasectomy were statistically significant for PFS,withvalues of 0.034,0.046,0.011,and 0.001,respectively.Only liver metastasis and metastasectomy werestatistically significant for OS,withvalues of 0.001 and 0.002,respectively.
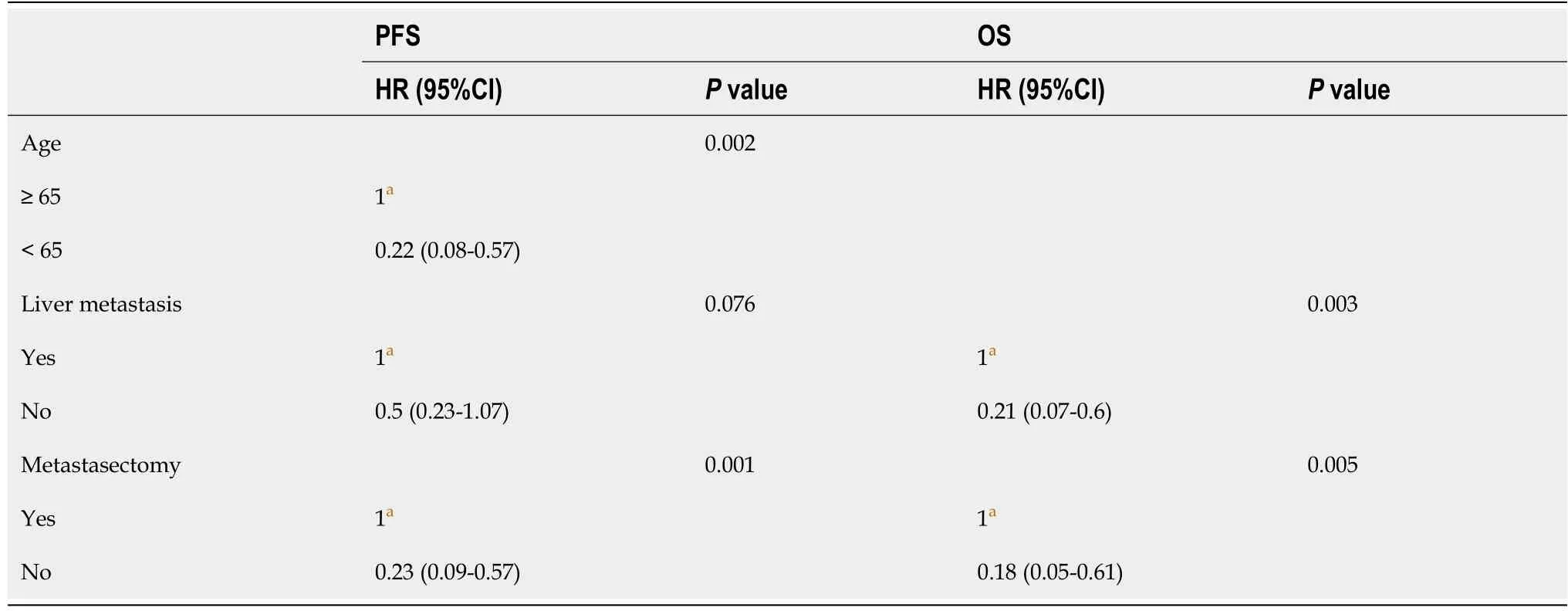
Multivariate analysis showed that age(less than 65 years)and metastasectomy were statistically significant for PFS,withvalues of 0.002 and 0.001,respectively.On the other hand,the absence of liver metastasis and metastasectomy were statistically significant for OS,withvalues of 0.003 and 0.005,respectively(Table 3).
Amy did get her wish of a special day without teasing at South Wayne Elementary School. Additionally, everyone at school got another bonus. Teachers and students talked together about how bad teasing can make others feel.
DISCUSSION
To our knowledge,this is the first study to evaluate the prognostic significance of peritoneal metastasis in patients with metastatic CRC treated primarily with triplet first-line chemotherapy.Historically,the presence of peritoneal carcinomatosis in patients with metastatic CRC has resulted in poor prognosis[13,14].The median OS in patients treated with modern chemotherapy regimens,including targeted therapy,has ranged from 8 to 12 mo[17].Bakkers[17]reported a population-based study with 7233 patients with metastatic CRC,of which 743 had peritoneal carcinomatosis.The median OS for the 409patients with synchronous peritoneal carcinomatosis was 8.1 mo compared to 12 mo for those with metachronous peritoneal metastasis.This difference was not statistically significant in multivariate analysis,with a hazard ratio of 1.03(95%CI: 0.83-1.27).Since this was a population-based study,treatment consisted of palliative chemotherapy,cytoreductive surgery with hyperthermic intraperitoneal chemotherapy(CRS-HIPEC)and best supportive care.The percentage of patients who had CRS
HIPEC in the above study was 16% in the metachronous group and 8% in the synchronous group.Palliative chemotherapy was given to 55% and 69% of patients in the metachronous and synchronous groups,respectively.
A more similar cohort to our study was the pooled analysis reported by Franko[13],wherein they looked at the survival and prognostic significance of patients with peritoneal metastasisother organ metastasis from two large north central cancer treatment group phase III studies(N9741 and N9841).Since those patients were entered in a prospective clinical trial,all had good performance status from 0 to 1 and expected survival of more than 3 mo with no negative prognostic factors such as ascites or malignant bowel obstruction.All patients were treated with doublet regimens(FOLFOXIFLIROX).There was no differential impact of the type of systemic chemotherapy used on the basis of the presence or absence of peritoneal carcinomatosis.Expectedly,peritoneal carcinomatosis in this pooledanalysis had a negative prognostic impact on survival,with a hazard ratio(HR)of 1.316(95%CI: 1.152-1.504,<0.0001).Other investigators at an earlier date found no benefit of infusional 5-fluorouracil(5-FU)as opposed to bolus 5-FU in patients treated for CRC with peritoneal metastasis[18].
Our cohort was treated uniformly with the combination of capecitabine,oxaliplatin,irinotecan,and bevacizumab.The PFS was 9.4 mo for patients with no peritoneal metastasis13.7 mo in patients with peritoneal carcinomatosis.A difference was not statistically significant in univariate and multivariate analyses.Similarly,OS in our cohort was not reached for patients with peritoneal carcinomatosis compared to 31.3 mo in the no peritoneal metastasis group(= 0.0368,univariate analysis).The median follow-up for the whole group was 89 mo.
Generally,survival in patients with peritoneal carcinomatosis from CRC metastasis has improved with the introduction of CRS-HIPEC.The benefit of CRS-HIPEC has been proven in randomized controlled clinical trials using older chemotherapy regimens(fluoropyrimidine alone)[19].There are,however,multiple prospective phase II and retrospective studies reporting a 3-year survival of 30% to 60% in patients with isolated peritoneal carcinomatosis treated with CRS-HIPEC[20-24].In our cohort,the percentage of metastasectomy that could have influenced the efficacy of our therapy was 33.3% in the peritoneal carcinomatosis group22.2% in the no peritoneal carcinomatosis group,a difference that did not reach statistical significance.We accordingly believe that surgery played a partial role in the good results seen in the group of peritoneal metastases.
Peris who had seen Gul consumed by her love for me now interceded170 with the king, and said: It is clear that your daughter s fortunes are bound up with his, for the fire has not hurt him
OS was defined as the time to death of any cause,while PFS was defined as the time to disease progression,recurrence,or death from any cause.Surviving patients were censored at last follow-up.Probabilities of OS and PFS were calculated using the Kaplan-Meier estimator with variance calculated using the Greenwood formula.Survival curves were compared using log-rank test.Multivariate analysis was performed using the cox proportional hazard regression model.The proportional hazards assumption was tested,and covariates that violated the proportional hazards assumption were added as time-dependent covariates.value <0.05 was considered significant.Analysis was conducted using RStudio.Version 1.4.1106 © 2009-2021 RStudio,PBC.The statistical methods of this study were performed and reviewed by Tusneem Elhassan from King Faisal Specialist Hospital and Research Center.
CONCLUSION
In conclusion,our data showing equal survival in metastatic CRC patients with peritoneal metastasisno peritoneal metastasis and the absence of a negative prognostic impact of peritoneal carcinomatosis when patients are treated with a triplet chemotherapy regimen as a first-line therapy is hypothesisgenerating.These data need to be confirmed in large prospective studies.
ARTICLE HIGHLIGHTS
Research background
All study participants,or their legal guardian,provided informed written consent prior to study enrollment.
“I must travel,” he had said to her; “I must see this beautiful princess; my parents desire it; but they will not oblige me to bring her home as my bride
Research motivation
We have shown before that triplet first-line chemotherapy in metastatic CRC overcomes the poor prognosis of right-sidedness.We wanted to examine whether the same applies to peritoneal metastasis in CRC.
Research objectives
We wanted to examine the progression-free survival(PFS)and overall survival(OS)of patients with peritoneal vs no peritoneal metastasis treated with first-line triplet chemotherapy and to confirm the lack of a statistically significant difference in the two groups on univariate and multivariate analysis.
21. Lost her breath and fell down as if dead: The first temptation relates to Snow White s body, but the bodice laces bind her too tight and she cannot breath - breath is a symbol of the spirit. IRReturn to place in story.
Research methods
This was a post hoc analysis of a phase I/II trial evaluating the efficacy and toxicity of triplet chemotherapy in the first-line treatment of metastatic CRC.Patient characteristics,PFS,and OS were examined for the groups with and without peritoneal metastasis.Univariate and multivariate analyses were performed to include other known prognostic factors in metastatic CRC.
Research results
No statistically significant difference was found in the PFS and OS in the group with or without peritoneal metastasis.Peritoneal metastasis was confirmed not to be an independent prognostic factor in patients with metastatic CRC treated with first-line triplet chemotherapy based on multivariate analysis.
Bettelheim states: Starvation anxiety has driven him [Hansel] back, so now he can think only of food as offering a solution to the problem of finding his way out of a serious predicament (Bettelheim 1976). Unfortunately, Hansel appears to have forgotten that birds will eat bread crumbs and destroy his trail. Return to place in story.
Research conclusions
The study suggests that first-line triplet chemotherapy overcomes the poor prognostic significance of patients with metastatic CRC.This needs to be confirmed in large prospective trials.
Research perspectives
The present study represents a post hoc analysis of the previously published phase I/II trial of triplet therapy in patients with unresectable metastatic or locally advanced CRC.Efficacy data were analyzed according to the presencethe absence of peritoneal metastasis.
FOOTNOTES
This study is registered at https://clinicaltrials.gov/ct2/show/NCT01311050?term=bazarbashi&draw=2&rank=4.The registration identification number is: NCT01311050.
This study was reviewed and approved by the Institutional Review Board at King Faisal Specialist Hospital and Research Center under the number RAC2081068.
Bazarbashi S contributed to designing the study;Bazarbashi S,Alghabban A and Aseafan M contributed to data analysis;Bazarbashi S,Alghabban A,Aseafan M,Aljubran AH and Alzahrani A contributed to write the manuscript;Elhassan TA has contributed to the statistical analysis.
Meantime the golden lad dreamt that he was out hunting and was giving chase to a noble stag, and when he woke he said to his bride: I must go off and hunt
Peritoneal metastasis has been shown to be a poor prognostic factor in metastatic colorectal cancer(CRC).In all published literature citing the above,the patients were treated with either single or doublet first-line chemotherapy.There are no data on the prognostic significance of peritoneal carcinomatosis in patients treated with first-line triplet chemotherapy.
All authors have nothing to disclose.
When the ship was finished the launch took place, and everything seemed going smoothly4 when a gale5 sprang up, and the vessel6 was dashed to pieces on the rocks
No additional data are available.
It is the fallacy of the time, and manypoets express it, to say that all that is noble is bad and stupid, andthat, on the contrary, the lower one goes among the poor, the morebrilliant virtues38 one finds
The authors have read the CONSORT 2010 statement,and since the study is not randomized trial,the CONSORT 2010 statement do not apply.
This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial(CC BYNC 4.0)license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is noncommercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
Saudi Arabia
Shouki Bazarbashi 0000-0002-8913-8158;Abdulrahman Alghabban 0000-0003-3009-1014;Mohamed Aseafan 0000-0001-9993-9664;Ali H Aljubran 0000-0001-9130-2968;Ahmed Alzahrani 0000-0003-4406-8835;Tusneem AM Elhassan 0000-0002-1625-1168.
Wang JJ
A
Wang JJ
 World Journal of Clinical Cases2022年8期
World Journal of Clinical Cases2022年8期
- World Journal of Clinical Cases的其它文章
- Analysis of bacterial spectrum,activin A,and CD64 in chronic obstructive pulmonary disease patients complicated with pulmonary infections
- Developing natural marine products for treating liver diseases
- Computed tomography perfusion imaging evaluation of angiogenesis in patients with pancreatic adenocarcinoma
- Epidemiological features and dynamic changes in blood biochemical indices for COVID-19 patients in Hebi
- Identification and predictive analysis for participants at ultra-high risk of psychosis:A comparison of three psychometric diagnostic interviews
- Effect of intraoperative cell rescue on bleeding related indexes after cesarean section
