Safety, immunogenicity, efficacy, and acceptability of COVID-19 vaccination in people with multiple sclerosis: a narrative review
Fioravante Capone, Mariagrazia Rossi, Alessandro Cruciani, Francesco Motolese, Fabio Pilato, Vincenzo Di Lazzaro
Abstract In the last two years, a new severe acute respiratory syndrome coronavirus (SARS-CoV) infection has spread worldwide leading to the death of millions. Vaccination represents the key factor in the global strategy against this pandemic, but it also poses several problems, especially for vulnerable people such as patients with multiple sclerosis. In this review, we have briefly summarized the main findings of the safety, efficacy, and acceptability of Coronavirus Disease 2019 (COVID-19) vaccination for multiple sclerosis patients. Although the acceptability of COVID-19 vaccines has progressively increased in the last year, a small but significant part of patients with multiple sclerosis still has relevant concerns about vaccination that make them hesitant about receiving the COVID-19 vaccine. Overall, available data suggest that the COVID-19 vaccination is safe and effective in multiple sclerosis patients, even though some pharmacological treatments such as anti-CD20 therapies or sphingosine l-phosphate receptor modulators can reduce the immune response to vaccination. Accordingly, COVID-19 vaccination should be strongly recommended for people with multiple sclerosis and, in patients treated with anti-CD20 therapies and sphingosine l-phosphate receptor modulators, and clinicians should evaluate the appropriate timing for vaccine administration. Further studies are necessary to understand the role of cellular immunity in COVID-19 vaccination and the possible usefulness of booster jabs. On the other hand, it is mandatory to learn more about the reasons why people refuse vaccination. This would help to design a more effective communication campaign aimed at increasing vaccination coverage among vulnerable people.
Key Words: COVID-19; multiple sclerosis; SARS-CoV-2; vaccination; vaccine
Introduction 284 Search Strategy and Selection Criteria 284 COVID-19 Vaccine and Multiple Sclerosis 285 Discussion 287 Conclusions 287
Introduction
In 2019, the pandemic caused by Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) infection started to spread around the world, affecting millions of people. The Coronavirus Disease 2019 (COVID-19) causes a complex set of symptoms, primarily involving the respiratory tract, but in many cases affecting also multiple organs and leading to life-threatening conditions or even death. To date, 347 million people have been infected, and 5.57 million deaths have been reported all around the world (No author listed, 2022a). Like many other viruses, SARS-CoV-2 tends to mutate over time. The currently used nomenclature divided variants into four classes: Variant Being Monitored (VBM), Variant of Interest (VOI), Variant of Concern (VOC), and Variant of High Consequence (VOHC) (Arora et al., 2022). The currently circulating VOCs are the delta and omicron, while previously circulating VOCs include alpha, beta, and gamma variants (No author listed, 2022b).
Over the past two years, new therapeutic strategies (i.e., antiviral drugs, humanized and recombinant monoclonal antibodies) have been developed, leading to a significant reduction in death and severe complications. However, only a global vaccination campaign can bring things to normal, since a large amount of data (Lopez Bernal et al., 2021; Tenforde et al., 2021) has shown the reduction of hospitalization and complication rates following the extensive vaccination of the population. Vaccination is especially recommended for vulnerable people such as the elderly and patients with chronic diseases and/or those who are receiving pharmacological treatments with effects on the immune system.
People with multiple sclerosis (PwMS) are considered at a high risk for COVID-19-related complications for several reasons (Brownlee et al., 2020) Moreover, it has been shown that infections are associated with an increased risk of relapses or pseudo-relapses in PwMS, and infection-associated relapses are more likely to induce sustained disability (Buljevac et al, 2002). Finally, some subgroups of MS patients, as those taking anti-CD20 drugs, may be at higher risk both for SARS-CoV-2 infection and for COVID-19-related complications (Reder et al., 2021). A recent study reported a higher incidence of COVID-19 in an MS cohort compared to the general population, despite most patients did not require hospitalization and had a positive outcome (Sepúlveda et al., 2021). On the other hand, PwMS who died of COVID-19 were at a high risk for developing severe COVID-19 complications because of individual factors such as age, comorbidity, or severe disability (Barzegar et al., 2021). The evidence has confirmed that there is no difference in the infection rate among drugnaïve PwMS and those receiving IFN-β, glatiramer acetate, and fingolimod. Whereas second-line treatment options, such as cladribine, alemtuzumab, and hematopoietic stem cell transplantation, have been related to the highest risk of infection (Rostami and Ghasemi-Kasman, 2021). For all these reasons, PwMS are considered a vulnerable group in many countries and have been given priority in the administration of the vaccine. As of January 2022, more than 20 vaccines with different mechanisms of action (mRNA, viral vector, and recombinant protein subunit vaccine) have been approved worldwide (No author listed, 2022c). In many countries, policymakers decided to make mRNA vaccines the first choice for vulnerable people, including PwMS, because of their safety profile, the low production cost, the ready availability, and their higher efficacy (Polack et al., 2020). For this reason, most of the data presented in this review refers to mRNA vaccines (Moderna mRNA-1273 and Pfizer/BioNTech BNT162b2). In December 2021, a new vaccine was approved in Europe, developed by Novavax (NVX-CoV2373) and described as both a protein subunit vaccine and a virus-like particle vaccine (Woopen et al., 2021). At present, there are no reports of serious immune-mediated or neurological events with NVX-CoV2373 (Keech et al., 2020). This is in line with the well-known evidence on the efficacy and safety of subunit vaccines for other conditions (i.e., Hemophilus influenzae B Hib, hepatitis B, human papillomavirus, whooping cough, pneumococcal disease, meningococcal disease, and shingles) in MS patients (Mailand and Frederiksen, 2017). In the next few months, MS international societies may now consider NVX-CoV2373 a preferable vaccine for MS patients over those mRNA-based (Heath et al., 2021). Aim of this review is to summarize the main findings of the safety, efficacy, and acceptability of COVID-19 vaccination for MS patients.
Search Strategy and Selection Criteria
The current review considers articles published from 2020 to 2022. The manuscripts were searched electronically using PubMed and Google Scholar databases. We used a combination of the following keywords/terms: COVID-19, SARS-CoV-2, multiple sclerosis, vaccine, safety, efficacy, acceptability, willingness, immunogenicity, side effects, disease-modifying therapies, humoral response, and cellular response.
COVID-19 Vaccine and Multiple Sclerosis
Safety and side effects
Reported side effects of mRNA vaccines in the general population were mildto-moderate, and included injection-site pain, short-lived febrile symptoms, fatigue, and headache (Polak et al., 2020; Baden et al., 2021). Overall, literature data showed roughly the same short-term side effects in the MS population. Achiron et al. (2021) first described the safety profile of Pfizer/BioNTech BNT162b2 vaccine in a group of 555 PwMS. All the adverse events reported were mild-to-moderate, more evident in younger patients, and more frequent in patients with lower disability (expanded disability status scale ≤ 3) and after the second dose (Achiron et al., 2021). An Italian study on 140 PwMS who received both types of mRNA-based vaccines reported similar data. In particular, patients experienced pain at the injection site, fatigue, myalgia, and fever as short-term side effects, especially after the second dose. In this study, no severe side effects requiring hospitalization or unusual adverse events were reported (Capone et al., 2021).
A specific cause for concern in PwMS is the risk of reactivation of disease induced by COVID-19 vaccines. Indeed, anecdotal reports suggest that such vaccines might be associated with central and peripheral nervous system inflammation. A first case series reported the clinical and MRI features of seven individuals who received SARS-CoV-2 mRNA vaccines who developed neurologic symptoms and MRI findings consistent with active central nervous system (CNS) demyelination (3 new-onset demyelinating diseases and 4 exacerbations of MS) (Khayat-Khoei et al., 2022). A recent systematic review has identified 32 cases of CNS demyelination following the administration of different types of COVID-19 vaccine. Demyelinating syndromes were more frequent after administration of mRNA-based vaccines, especially following the first dose. The clinical presentation was heterogeneous, including transverse myelitis, MS onset, acute disseminated encephalomyelitis, and neuromyelitis optica spectrum disorders. More than half of the cases had a history of immune-mediated diseases, with favorable outcomes in most cases (Ismail and Salama, 2022a).
On the other side, studies specifically designed to evaluate the safety of COVID-19 vaccines in people with a previous diagnosis of demyelinating disease, including MS, demonstrated that the incidence of new symptoms or the worsening of symptoms was relatively low and the relapse rate was comparable to that reported in non-vaccinated people (Lotan et al., 2021). A more detailed study conducted in a larger cohort of MS patients (324 PwMS) who received the Pfizer/BioNTech BNT162b2 vaccine showed that the incidence of relapses in the 2 months before and after vaccination was not statistically different (Di Filippo et al., 2021). Epstein et al. (2022) have collected data from 1164 patients with neuroinflammatory diseases including MS, neuromyelitis optica spectrum disorders, neurosarcoidosis, and myelin oligodendrocyte antibody-mediated disease. Their results suggested that SARS-CoV-2 vaccines in these patients are safe, and it seems unlikely they could worsen the underlying disease activity, both from the clinical and radiological viewpoint (Epstein et al., 2022). No data are available regarding the booster jabs. Thus, in absence of definite guidelines, the management of vaccination schedules in high-risk MS patients should be decided on a caseby-case basis. Finally, the risk of neuroinflammation induced by COVID-19 itself should be considered. A recent review has described 102 cases of CNS demyelination putatively associated with SARS-CoV-2 infection from January 2020 until June 2021 (Ismail and Salama, 2022b). This is in line with the robust evidence in the literature reporting a higher risk of inflammatory neurologic complications after COVID-19 than neurologic adverse events following immunization (Garcia-Grimshaw et al., 2021). To maintain the protection against SARS-Cov-2, a third and a fourth dose of vaccine are currently being administered worldwide. To date, few studies have investigated the safety of booster jabs in PwMS.
Available data (Achtnichts et al., 2021; Dreyer-Alster et al., 2022; König et al., 2022) suggest that the safety profile is similar to that reported following the first and second doses. Moreover, the frequency of MS symptoms worsening and acute relapses within the first 30 days after the third dose is similar to that reported after the second dose (Achtnichts et al., 2021).
In conclusion, based on available data, COVID-19 vaccination should be recommended in all PwMS, because the risk of morbidity, mortality, and neuroinflammation associated with COVID-19 largely outweighs the low percentage of serious neurologic and non-neurologic adverse events associated with vaccines. Surely, long-term post-marketing surveillance is necessary to confirm the safety of COVID-19 vaccines also in real-life scenarios.
Immunogenicity and efficacy
The immunogenicity of a vaccine (i.e., inducing the immune response) is a key factor in determining its efficacy. In PwMS, several factors could influence the immunogenicity of COVID-19 vaccines and should be considered. First of all, MS is an autoimmune disease, thus the alteration of immune system functioning could impair vaccine immunogenicity. To test this hypothesis, several studies have investigated the humoral response following SARSCov-2 vaccination in MS patients naïve to disease-modifying therapies (DMTs) (Achiron et al., 2021; Capone et al., 2021; Pitzalis et al., 2021; Sormani et al., 2021a; Tallantyre et al., 2022). All of them found anti-SARS-CoV-2 antibody levels comparable to those observed in healthy people, thus confirming that MS is not associated per se with an increased risk of developing an attenuated response to SARS-CoV-2 vaccines.The DMTs act on the immune system and could influence the response to vaccinations. Therefore, several studies have investigated how the use of different DMTs could influence the development of post-vaccination immunity against SARS-Cov-2 (Table 1
). Most of them have measured the humoral response to vaccination while the cellular response is still little investigated.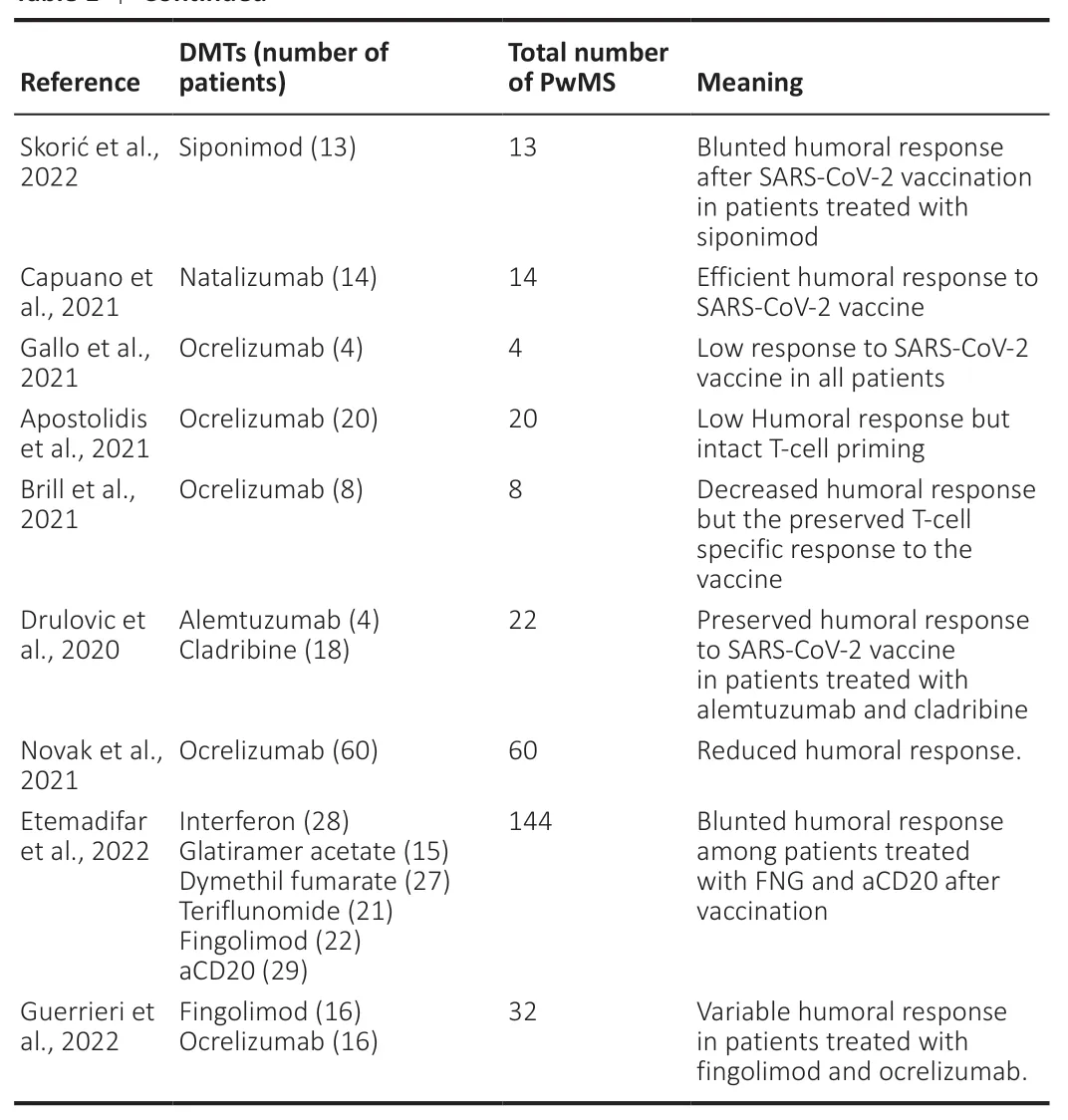
Table 1 |Continued
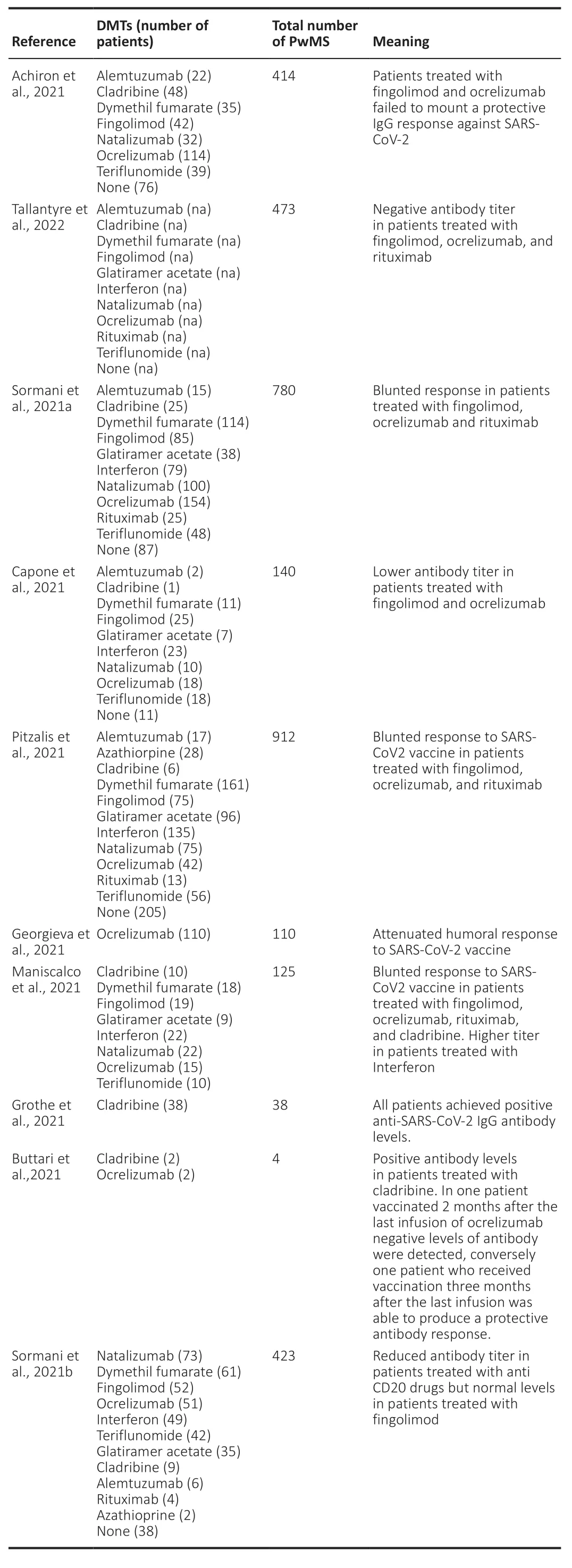
Table 1 |Studies on SARS-CoV-2 vaccination in MS patients treated with different DMTs
To date, all studies on the immunogenicity of the anti-SARS-CoV-2 vaccines in patients treated with interferon, dimethyl fumarate, glatiramer acetate, and teriflunomide have demonstrated an adequate antibody response (Achiron et al., 2021; Capone et al., 2021; Georgieva et al., 2021; Pitzalis et al., 2021; Sormani et al., 2021b; Tallantyre et al., 2022).
Interestingly, one study shows that patients treated with interferon have a higher IgG titer compared to healthy subjects (Maniscalco et al., 2021). The authors suggested that this finding could be linked to the interferon mechanism of action that does not involve peripheral lymphocytes.
Besides, even patients treated with cladribine (Achiron et al., 2021; Capone et al., 2021; Georgieva et al., 2021; Grothe et al., 2021; Pitzalis et al., 2021; Sormani et al., 2021b; Tallantyre et al., 2022), alemtuzumab (Drulovic et al, 2020; Achiron et al., 2021; Capone et al., 2021; Georgieva et al., 2021; Pitzalis et al., 2021; Sormani et al., 2021b; Tallantyre et al., 2022), and natalizumab (Achiron et al., 2021; Capone et al., 2021; Ciotti et al., 2020; Georgieva et al., 2021; Pitzalis et al., 2021; Sormani et al., 2021b; Tallantyre et al., 2022) have an adequate humoral response. Only one study involving 10 patients treated with cladribine found a lower level of serum antibodies compared with healthy subjects or MS patients treated with other DMTs (Maniscalco et al., 2021).
Because of their mechanism of action, sphingosine l-phosphate receptor modulators and anti-CD20 antibodies can reduce the immunogenicity of vaccinations. Accordingly, these drugs have been the object of specific interest in several recent studies.
The sphingosine l-phosphate receptor modulators (fingolimod, ozanimod, siponimod) act by regulating lymphocyte egress from lymphoid tissues into the circulation. It is well-known that patients treated with fingolimod develop a lower level of antibodies after flu vaccination (Ciotti et al., 2020). This observation has been also confirmed for SARS-CoV-2 vaccination (Achiron et al., 2021; Achtnichts et al., 2021; Capone et al., 2021; Pitzalis et al., 2021; Sormani et al., 2021b; Konig et al., 2022; Tallantyre et al., 2022). Only one study (Sormani et al., 2021b) showed an adequate immune response in patients treated with fingolimod. To date, no data are available for ozanimod while only one article has evaluated the humoral response in patients treated with siponimod (Skorić et al., 2022). In this paper, 13 patients with secondary progressive MS treated with siponimod were tested for SARS-CoV-2 antibodies in comparison to 11 healthy subjects. Although the sample size is small, results consistently show that patients treated with siponimod have a blunted humoral response to SARS-CoV-2 vaccination.
Ocrelizumab and ofatumumab are anti-CD20 antibodies that deplete circulating immature and mature B cells but spare CD20-negative plasma cells. Most studies have shown that patients treated with ocrelizumab have an insufficient humoral response after SARS-CoV-2 vaccination (Bar-Or et al., 2020; Ciotti et al., 2020; Achiron et al., 2021; Gallo et al., 2021; Maniscalco et al., 2021; Novak et al., 2021; Pitzalis et al., 2021; Sormani et al., 2021b; Etemadifar et al., 2022). These data could be explained if we consider the strong depletion of CD20 cells induced by the drug. Only one study (Guerrieri et al., 2021) suggests a different outcome in patients treated with ocrelizumab. Up to now, there are no data about the effect of ofatumumab on the immunogenicity of the SARS-CoV-2 vaccines.
Since the protection against coronavirus cannot be explained entirely by humoral immunity, the cellular response has also been investigated in patients treated with anti-CD20 therapies. Apostolidis et al. (2021) found that the mRNA vaccines provide a strong immune cellular response in patients treated with ocrelizumab although most of those do not develop an optimal level of antibodies (Apostolidis et al., 2021). This conclusion is supported by the presence of high levels of functional Th1 and CD8 T-cells in most of the subjects, even in those patients in which the anti-CD20 therapy altered significantly the antigen-specific T follicular helper cells response. Brill et al. (2021) show similar results demonstrating that patients treated with ocrelizumab develop a SARS-CoV-2 specific T-cell response comparable with healthy controls despite a lower level of serum antibodies (Brill et al., 2021). Those data suggest that patients treated with ocrelizumab can benefit from the administration of SARS-CoV-2 vaccine as well.
In the last months, some studies have investigated the humoral response to the third dose of the SARS-CoV-2 vaccine in PwMS.
Dreyer-Alster et al. (2022) have evaluated, in a cohort of 211 PwMS, the safety of the third dose of Pfizer BNT162b2 vaccine. Moreover, in a subgroup of 55 patients treated with different DMTs, they also measured the level of anti-SARS-CoV-2 IgG antibodies before and after the administration of the third dose. They found a 21-fold increase in IgG titers following the booster jab (Dreyer-Alster et al., 2022).
Interestingly, none of the patients included in this sample was in treatment with ocrelizumab or fingolimod, which have been associated, as previously said, with blunted humoral response to the SARS-CoV-2 vaccine.
This issue was specifically addressed in two subsequent studies. Kӧnig et al. (2022) measured the levels of anti-SARS-CoV-2 IgG titer after the third dose in 130 MS patients with a weak humoral immune response after 2 doses of mRNA COVID-19 vaccines. Among them, 100 patients were treated with rituximab, 1 patient with ocrelizumab, and 29 patients with fingolimod (Kӧnig et al., 2022).
They found out that the anti-SARS-CoV-2 IgG titer increased significantly in all patients after the third dose. The proportion of patients that developed protective humoral immunity after the third dose was 24.8% in the group on anti-CD20 treatment and 6.9% in the group on fingolimod.
Similarly, even Achtnichts et al. (2021) investigated the humoral response after the third dose of SARS-CoV-2 mRNA vaccination in 16 MS patients on anti-CD20 therapies that previously failed to reach adequate IgG antibodies levels with the second dose (Achtnichts et al., 2021). Differently from Kӧnig et al. (2022), in this cohort, only one patient developed a protective humoral immune response after the booster jab.
To date, few data on the incidence of breakthrough COVID-19 among vaccinated PwMS are available in the literature (Chilmuri et al., 2021; Januel et al., 2021; Rose et al., 2021). Rose et al. (2021) described the cases of SARS-CoV-2 infection in 669 fully vaccinated patients with Moderna, Pfizer, or Janssen vaccines. Breakthrough COVID-19 was relieved in 13 patients, 10 in treatment with anti-CD20 therapy, and 3 with fingolimod. Only two of them required hospitalization. The interpretation of these results is limited by the absence of available SARS-CoV-2 antibody titers (Rose et al., 2021). A recent case-series report shows 18 cases of mild COVID-19 after two doses of BNT162b2-vaccination, 13 of which were treated with anti-CD20 therapy, 4 with fingolimod, and 1 with interferon beta (Januel et al., 2021). However, it should be noted that in this report, some patients on anti-CD20 treatment received vaccination during the maximum cell-depletion interval after administration and probably did not develop a valid seroconversion (Chilmuri et al., 2021).
Willingness
Despite the use of vaccines for the prevention of SARS-CoV-2 infection is universally recognized as one of the key factors in the fight against the pandemic, some people are still in doubt about vaccination. Several studies have assessed the willingness of the general population to receive the vaccine and the related determinants of this choice (Bell et al., 2020; Neumann-Bӧhme et al., 2020; Reiter et al., 2020). This issue is particularly relevant for vulnerable people that are at risk to develop severe COVID-19 complications. The first study that focused on MS patients was the one by Ehde et al. (2021), a cross-sectional study that assessed the willingness to receive COVID-19 vaccination in an U.S. population of 486 MS patients. The study was based on an online survey with a response on a 5-point scale (1 = not at all willing, 2 = a little willing, 3 = moderately willing, 4 = very willing, and 5 = extremely willing). They also assessed demographic data, MS disease-related features, and disease severity, together with measures of psychological distress. Moreover, they collected data on patients’ perceived risk of being infected, of being hospitalized for or dying from COVID-19 along with information on where they got informed about COVID and the trust in official communication about the pandemic. The results showed that during the early phase of the COVID-19 pandemic (between 10 April 2020 and 06 May 2020) about 66% of participants wanted to be vaccinated and, among all the factors included in the analysis, those most related to willingness were the school degree and the higher perception of being at risk for SARS-CoV-2 infection. One year later, the same authors conducted a follow-up survey in the period from January to February 2021, following the approval of COVID-19 vaccines (Ehde et al., 2021). They found that about 20% of the participants were vaccine-hesitant and the major concerns referred to the long-term effects of the vaccine, the vaccine approval process, and the potential impact of the vaccine given their own health conditions/history. Compared with the previous survey, the authors found that people who were in the “willing” or “undecided” groups became more willing but people who were “unwilling” in the first survey remained “unwilling” in the second survey. The authors concluded that vaccine hesitancy has decreased in the MS community during the COVID-19 pandemic, and the public effort should be targeted at the undecided population. Serrazina et al. (2021) tried to assess willingness to receive the COVID-19 vaccine in the European population affected with MS. They performed an observational, cross-sectional, hospital-based, singlecenter study, on 337 MS patients, using an online survey in the period between 21December 2020 and 3January 2021. They found that the 80.9% of MS participants were either definitely (35.2%) or probably willing (45.7%) to receive a COVID-19 vaccine whilst the 19.1% of patients said they definitely (2.7%) or probably (16.4%) would not get a COVID-19 vaccine (Serrazina et al., 2021). Another interesting piece of information was that a considerable number of patients prefer to postpone vaccination probably because of the concerns about the safety of COVID-19 vaccines. A third study was performed by Yap et al. (2021) based on a single-center Irish population of 105 MS patients, trying to assess the pneumococcal, influenza, and SARSCoV-2 vaccine attitude. They found that 91.5% of the participants were willing to receive the SARS-CoV-2 vaccination (Yap et al., 2021). This percentage was higher than that reported in other studies on COVID-19 vaccination (Ehde et al., 2021a; Ehde et al., 2021b; Serrazina et al., 2021), and higher than that obtained in the same study for influenza and pneumococcal vaccines (~80%). In this study, the most common reason for COVID-19 vaccine hesitancy was the safety concern. The authors concluded that the increased acceptability of COVID-19 vaccines among people with MS reflects the enormous public effort to emphasize the socio-economic benefits linked with the vaccination against SARS-CoV-2.
Discussion
To date, an estimated 2.8 million people are living with MS worldwide (No author listed, 2022d). COVID-19 pandemic poses an important challenge for all these people and for their caregivers. Surely, vaccination represents the key factor in the global strategy against the COVID-19 pandemic but, at the same time, several considerations should be done for vulnerable people such as PwMS.
In this review, we have briefly summarized the main available findings of COVID-19 vaccination in MS. In particular, we have reviewed data about the safety, efficacy, and acceptability of COVID-19 vaccines, in patients with MS, with a particular focus on the effects of DMTs.
Overall, in PwMS, COVID-19 vaccination is safe, and the profile of short-term side effects (in terms of frequency, symptoms, and severity) is similar to the general population (Achiron et al., 2021). A matter of specific concern for MS is the potential risk of disease reactivation induced by COVID-19 vaccination. Although few cases of CNS inflammation associated with vaccination have been described (Ismail and Salama, 2022a), available data suggest that, PwMS, is unlikely to observe a reactivation of disease, both clinically and radiologically. However, we have to acknowledge that only Class III evidence, coming from case reports, case-series and retrospective observations, is available. Further studies with a prospective design and larger samples are warranted.
Regarding booster jabs, few data are currently available about the administration of the third dose in PwMS. However, at present, no specific safety alerts have emerged.
Measuring the efficacy of vaccination in real-life poses different methodological problems. Indeed, most studies have measured the immunogenicity of the COVID-19 vaccine as a proxy of vaccination efficacy, whilst only a few studies have measured the number of people who got infected by SARS-CoV-2 after vaccination. Overall, the results of both approaches are similar and demonstrate that MS itself does not influence the efficacy of COVID-19 vaccination while the use of some DMTs may numb the immune response.
Evidence has clearly shown an adequate immune response for PwMS taking first-line DMTs such as interferon, dimethyl fumarate, glatiramer acetate, and teriflunomide, with a post-vaccination SARS-CoV-2 infection incidence rate equal to the general population. Treatment with natalizumab, cladribine, and alemtuzumab does not numb seroconversion to vaccines and offers protection against breakthrough COVID-19 as well. Conversely, patients in treatment with anti-CD20 therapies or sphingosine l-phosphate receptor modulators can have a reduced immune humoral response after COVID-19 vaccination.
Since the protection against the virus strongly relies on cellular immunity, some studies have explored whether such patients could have a protection against Sars-Cov-2 despite low levels of specific antibodies. Available data (Apostolidis et al., 2021; Brill et al., 2021) demonstrate that patients in therapy with ocrelizumab develop a SARS-CoV-2 specific T-cell response compared with one of healthy controls while, to our knowledge, no studies have investigated this effect in patients treated with sphingosine l-phosphate receptor modulators.
Moreover, available data (Rose et al., 2021) suggest that patients treated with anti-CD20 therapies and sphingosine l-phosphate receptor modulators could have a higher risk to develop COVID-19 despite vaccination compared to patients treated with other DMTs.
The administration of additional jabs has been proposed as a strategy to boost the immunity against SARS-COV-2 but there are still a few studies on the matter (Achtnichts et al., 2021; Dreyer-Alster et al., 2022; König et al., 2022).
Overall, available data showed that a small but significant part of PwMS has relevant concerns about vaccination that prevent them from receiving a COVID-19 vaccine. Such attitude also called vaccine hesitancy, is a well-known public health issue regarding the general population and not only PwMS (Zuzak et al., 2008).
Although the acceptability of COVID-19 vaccines has increased over the last year, vaccine hesitancy remains a significant problem with potentially dramatic consequences in vulnerable people such as PwMS.
Due to the importance of vaccination in the global strategy against COVID-19, further studies are warranted to understand why people refuse vaccination and to design more effective communication strategies aimed at increasing compliance with the vaccination campaign.
Conclusions
COVID-19 vaccination in PwMS is strongly recommended, considering their well-established safety profile, immunogenicity, and efficacy against SARSCoV-2 infection. Patients treated with anti-CD20 therapies and sphingosine l-phosphate receptor modulators can have a reduced humoral response and potentially a limited efficacy. In these patients, neurologists should evaluate the appropriate timing for vaccine administration and further studies are necessary to understand the role of cellular immunity and the possible usefulness of booster jabs.
In conclusion, based on available data, COVID-19 vaccination should be certainly recommended in PwMS irrespective of DMTs, because the risk of severe COVID-19 complications largely outweighs the low percentage of serious neurologic and non-neurologic adverse events associated with vaccines. Healthcare providers should unanimously promote vaccine uptake and a specific effort by institutions should be made to convince the undecided population. Surely, the careful post-marketing surveillance is also necessary to confirm the long-term safety of COVID-19 mRNA vaccines. Considering the results of previous studies on protein subunit vaccines, the approval of this kind of vaccine for COVID-19 (such as NVX-CoV2373) could further improve the vaccination coverage among PwMS.
Author contributions:
FC: Conceptualization and original draft preparation. MR, AC, and FM: data search and collection. FP and VDL: analysis and reviewing. All authors approved the final version of the manuscript.
Conflicts of interest:
The authors declare no conflicts of interest.
Availability of data and materials:
All data generated or analyzed during this study are included in this published article and its supplementary information files.
Open access statement:
This is an open access journal, and articles are distributed under the terms of the Creative Commons AttributionNonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
Open peer reviewer:
Elena Giusto, San Camillo Hospital: Ospedale San Camillo, Italy.
Additional file:
Open peer review report 1.
- 中国神经再生研究(英文版)的其它文章
- c-Abl kinase at the crossroads of healthy synaptic remodeling and synaptic dysfunction in neurodegenerative diseases
- The mechanism and relevant mediators associated with neuronal apoptosis and potential therapeutic targets in subarachnoid hemorrhage
- Microglia depletion as a therapeutic strategy: friend or foe in multiple sclerosis models?
- Brain and spinal cord trauma: what we know about the therapeutic potential of insulin growth factor 1 gene therapy
- Functions and mechanisms of cytosolic phospholipase A2 in central nervous system trauma
- Cre-recombinase systems for induction of neuronspecific knockout models: a guide for biomedical researchers