Brain and spinal cord trauma: what we know about the therapeutic potential of insulin growth factor 1 gene therapy
María Jose Bellini, Florencia Labombarda
Abstract Although little attention has been paid to cognitive and emotional dysfunctions observed in patients after spinal cord injury, several reports have described impairments in cognitive abilities. Our group also has contributed significantly to the study of cognitive impairments in a rat model of spinal cord injury. These findings are very significant because they demonstrate that cognitive and mood deficits are not induced by lifestyle changes, drugs of abuse, and combined medication. They are related to changes in brain structures involved in cognition and emotion, such as the hippocampus. Chronic spinal cord injury decreases neurogenesis, enhances glial reactivity leading to hippocampal neuroinflammation, and triggers cognitive deficits. These brain distal abnormalities are recently called tertiary damage. Given that there is no treatment for Tertiary Damage, insulin growth factor 1 gene therapy emerges as a good candidate. Insulin growth factor 1 gene therapy recovers neurogenesis and induces the polarization from pro-inflammatory towards anti-inflammatory microglial phenotypes, which represents a potential strategy to treat the neuroinflammation that supports tertiary damage. Insulin growth factor 1 gene therapy can be extended to other central nervous system pathologies such as traumatic brain injury where the neuroinflammatory component is crucial. Insulin growth factor 1 gene therapy could emerge as a new therapeutic strategy for treating traumatic brain injury and spinal cord injury.
Key Words: cognitive impairments; gene therapy; hippocampus; insulin growth factor 1; microglial cells; neurodegeneration; neurogenesis; neuroinflammation; spinal cord injury; traumatic brain injury
Introduction 253 Cognitive and Emotional Consequences after Spinal Cord Injury 254 Hippocampal Abnormalities after Spinal Cord Injury 254 Insulin Growth Factor 1 Gene Therapy for Treating the Encephalopathy Caused by Spinal Cord Injury 255 Insulin Growth Factor 1 Therapy Associated with Traumatic Brain Injury 255 Conclusion 256
Introduction
Spinal cord injury (SCI) leads to permanent motor, sensory and autonomic dysfunction given the inability of the central nervous system (CNS) to regenerate. Mechanic SCI occurs when the spinal cord is severely bruised, compressed, lacerated, or severed as a result of the traumatic impact. The mechanic impact leads to primary damage which involves cellular death, extracellular matrix changes, edema formation, and blood-brain barrier breakdown. This primary damage drives to the well-known secondary damage characterized by microglia and astrocyte reactivity, periphery immune cell invasion, inflammation, and oxidative stress. These events result in neuron and oligodendrocyte death, which generate a loss of function (Ahuja et al., 2017).
Traditionally, SCI investigation was focused on pathophysiological changes in the spinal cord with efforts being made to recover sensorimotor function and relief neuropathic pain. In this regard, several studies have shown anterograde and retrograde axonal degeneration, which lead to the atrophy of the deafferented sensorimotor cortex (Wrigley et al., 2009; Freund et al., 2013). However, studies considering brain areas other than the sensorimotor system are scarce although humans suffer from cognitive and emotional impairment (Murray et al., 2007; Lazzaro et al., 2013; Craig et al., 2015). Interestingly, animal models have shown that SCI results in cognitive deficits and depressive-like behavior, which correlate with hippocampal neurodegeneration, neurogenesis reduction, and neuroinflammation (Wu et al., 2014a, b; Jure et al., 2021). Long-distal areas after SCI have been ignored for many years. Fortunately, this scenario has been changing lately. Compelling evidence suggests that SCI spreads to the brain affecting rostral distal areas and producing progressive neurodegeneration and neuroinflammation (Wrigley et al., 2009; Freund et al., 2013; Jure et al., 2021). In this regard, our group has defined this distal and rostral damage as Tertiary Damage.
Traumatic brain injury (TBI) pathophysiology also includes primary and secondary events. Primary injury is the consequence of the mechanical forces producing diffuse or focal damage. Secondary injury results from this early insult and it is characterized by a complex network of biochemical events that culminate in white matter damage and neurodegeneration contributing to behavioral morbidity. Curiously, glial alterations observed during Tertiary Damage resemble changes described in the brain after TBI. Indeed, chronic neuroinflammation is an important pathophysiological mechanism underlying neurodegeneration following TBI and it is associated with neurological, cognitive, and psychiatric disorders (Rodgers et al., 2014). The persistence of pro-inflammatory neurotoxic microglia might explain the progressive neuronal loss and chronic brain atrophy described after TBI (Loane et al., 2014).
Given that chronic neuroinflammation and microglial activation are associated with chronic neurodegeneration and cognitive deficits, therapeutic strategies designed to modulate these processes should be addressed. In this regard, therapies based on insulin growth factor 1 (IGF-1) could be a promising possibility. IGF-1 is a hormone protein that plays an important role during development and adulthood as it is involved in the regulation of growth and cellular proliferation. This growth factor is predominantly released by the liver and its synthesis is stimulated by growth hormone. However, a variety of tissues produces IGF-1 at distinctive times. Particularly, in the CNS, it has neurotrophic and neuroprotective functions, playing an important role in neuronal rescue during neurodegenerative processes (Acaz-Fonseca et al., 2015; Labandeira et al., 2017).
Gene therapy appears as a fascinating option to treat CNS trauma and neurodegenerative diseases. This therapy potentially leads to neuroprotection, neurorestoration, and the correction of pathogenic mechanisms by inducing the expression of specific proteins (Sudhaker et al., 2019). Furthermore, gene delivery to the CNS using adenovirus results to be safe and well-tolerated (O`Connor et al., 2015). In this sense, a recombinant adenoviral construct harboring the cDNA of rat IGF-1 (RAd-IGF1) has been used to treat neuroinflammation in aged rats and after experimental SCI (Falomir-Lockhart et al., 2019; Jure et al., 2021).
Firstly, in this review, we will discuss not only cognitive and emotional impairments observed after SCI but also evidence on hippocampal abnormalities. Secondly, IGF-1 gene therapy to treat behavioral and hippocampal alterations after SCI will be considered. Finally, the possibilities of IGF-1 gene therapy to deal with TBI will be analyzed.
Search Strategy and Selection Criteria
Studies cited in this review were published from 2000 to 2021 and they were searched on the PubMed and Google scholar databases using the followings keywords: brain and spinal cord injury, IGF-1 gene therapy and IGF-1 and traumatic brain injury.
Cognitive and Emotional Consequences after Spinal Cord Injury
Although little attention has been paid to cognitive and emotional dysfunctions observed in patients after SCI, several reports have described impairments in executive functioning, concentration ability, memory function, attention, learning, and processing speed impairment (Murray et al., 2007; Lazzaro et al., 2013; Craig et al., 2015). Cognitive impairments were underestimated by the scientific community because sixty percent of spinal cord injured patients suffer from depression, anxiety, and neuropathic pain (Li et al., 2020). Certainly, all these conditions contribute to decreasing quality of life, reducing social participation, and affecting cognition (Craig et al., 2015). Therefore, it is very complex to discern what the causes of their cognitive deficits are. It is crucial to develop animal models to study the biological changes in the brain after SCI that lead to cognitive changes and behavioral alterations.
In this regard, Faden’s work is very significant because it demonstrates for the first time that SCI causes emotional and cognitive deficits in rodents (Wu et al., 2014a, b). In their work, mice received a moderate contusion injury in the thoracic segment of the spinal cord to let animals perform tests, which implied locomotion. Contextual and emotional memory was evaluated using the step-down fear-avoidance test. Results show that lesioned mice decreased latency in the testing phase demonstrating impaired memory related to aversive experience. The authors also have explored depression-like behavior using the tail suspension and sucrose preference tests, neither of which related to locomotion. Injured mice were found to increase immobility time in the tail suspension tests and to reduce sweet water consumption during the sucrose preference, indicating depression-like behavior (Wu et al., 2014a).
Our group also has contributed significantly to the study of cognitive impairments after SCI. Recognition and working memory were evaluated using a compression model of spinal lesions, which let rats walk (Jure et al., 2021). Spatial working memory was evaluated by the Y-Maze spontaneous alternation test. Lesioned rats displayed a reduction of spontaneous alternation, indicative of dysfunctional spatial working memory (Jure et al., 2021). On the other hand, recognition memory was evaluated by the Novel object recognition test (NOR) and results showed that lesioned rats spent less time exploring the novel object in the recognition phase than sham ones demonstrating that injured rats were not able to discriminate between the novel and the familiar object, an indicative of impaired recognition memory (Jure et al., 2021).
These findings are very significant because they demonstrate that cognitive and mood deficits are not induced by lifestyle changes, drugs of abuse, and combined medication. They are related to changes in brain structures involved in cognition and emotion, such as the hippocampus.
Hippocampal Abnormalities after Spinal Cord Injury
Hippocampal neurons
The hippocampus has an impressive capacity for adaptive plasticity since neuronal circuits undergo constant modifications in dendritic complexity. Numerous reports describe that hippocampal dysfunction generates cognitive impairment in hippocampal-dependent learning such as retention and spatial memory (Belarbi et al., 2012; Li et al., 2016). In this regard, hippocampal failures are associated with low NOR and Y-maze performances (Broadbent et al., 2010). In line with these findings, depressive-like behaviors are reported using the sucrose preference and the force swim test after hippocampal ischemia in mice (Luo et al., 2019).
Since cognitive and emotional impairment described in humans and rodents after SCI is related to hippocampal-dependent functions, one of the aims of our laboratory is to study the impact of SCI on this structure. We have recently demonstrated that SCI increased hippocampal vulnerability in mice. The number of mature neurons of both the dorsal granular cell layer (GCL) and pyramidal cell layer 1 (CA1) remained unchanged during the acute phase, but neural density declined in the chronic phase following SCI (Jure et al., 2022). Faden’s group has also shown that the number of total hippocampal neurons remained unchanged in the acute phase and decreased in the chronic phase (Wu et al., 2014b).
Neurogenesis
The subgranular zone (SGZ) of the dentate gyrus of the hippocampus is one of the brain regions where the generation of new neurons continues throughout life due to the persistence of a neural stem cell (NSC) population (Toda and Gage, 2018). Normally NSCs are activated and produce highly proliferative transit-amplifying neural progenitors (ANPs). ANPs mostly die by apoptosis during their transition to immature neurons (Sierra et al., 2010). The surviving ANPs differentiate into DCXimmature neurons first and then become mature neurons that integrate into the hippocampal circuitry. Adult-born neurons provide plastic properties, which are crucial in information processing (Toda and Gage, 2018).
The effect of SCI on neurogenesis during the acute phase is controversial. Our results, in accordance with a previous study (Felix et al., 2012), have described a reduction in the number of doublecortin (DCX) cells during the first week after SCI (Felix et al., 2012; Jure et al., 2022). However, recent evidence has shown that neurogenesis increases after complete spinal cord transection two days post-injury but reaches control values after 3 months (Dehler et al., 2018). The use of different lesion models could explain the discrepancy in the results since transection lesions are usually characterized by a less rostral spread of secondary injury compared to the compression model used in our experiments (Beattie et al., 2000).
During the acute phase, NSC and ANP proliferation are unaltered, but the number of ANPs decreases. The reduction of the ANP population might be due to ANP death as the number of ANPs with abnormal nuclear morphology, indicative of cellular death, increases in lesioned mice (Jure et al., 2022). Acute stress could explain the reduction of neurogenesis in the acute phase because glucocorticoids are well-known inhibitors of neurogenesis (Lucassen et al., 2015) and they are up-regulated during the first week after SCI (Popovich et al., 2001)
Long term effects of SCI on neurogenesis are less controversial. In agreement with Faden’s group, we have described a reduction in the number of immature neurons (DCXcells) in the SGZ after moderate and severe SCI during the chronic phase (Jure et al., 2017, 2022). Noteworthy, the reduction of DCXcells coincided with the expression of endoplasmic reticulum stress markers (Wu et al., 2016). In this regard, endoplasmic reticulum stress is related to newborn neurons´ death after traumatic brain injury (Hood et al., 2018).
Data obtained long term after injury indicates that the number of total NSCs is unchanged, suggesting the survival of these cells long term after SCI. However, dividing NSCs are down-regulated indicating their inactivation in the neurogenic niche (Jure et al., 2022). NSC quiescence is usually permanent and is related to neurodegenerative diseases, seizures, and aging (Sierra et al., 2014). Regarding ANPs, the number of both dividing and non-dividing precursor cells decreases probably as a consequence of the inhibition of their proliferation and/or the reduction of NSC activation (Jure et al., 2022). Changes in ANP proliferation are frequently transient and reversible such as those observed in exercise, deep brain stimulation, fluoxetine treatment, and acute stress (Sierra et al., 2014; Lucassen et al., 2015).
Any condition that provokes impairment of hippocampal neurogenesis is likely to have an impact on cognitive performance and emotional behavior. In fact, the inhibition of neurogenesis by irradiation, pharmacological and genetic tools impairs spatial-related memory and learning, pattern separation, and responses to fear and stress (Bergami et al., 2008; Oomen et al., 2014). Studies in mice that ablate adult-generated neurons have demonstrated that these neurons are crucial to form and endure spatial and contextual fear memories evaluated by Morris Water Maze and fear conditioning test (Arruda-Carvalho et al., 2011). On the other hand, several reports have described that neurogenesis up-regulation alleviates anxiety and reduces depressive-like behavior assessed by the elevated plus-maze, sucrose preference, and forced swim tests (O’Leary and Cryan, 2014).
Hippocampal neuroinflammation
Microglial cells alongside astrocytes manage the inflammatory response in the CNS. Microglia and astrocytes are plastic cells that respond to several kinds of molecules generating a different spectrum of functional phenotypes (Tang and Le, 2016). Homeostasis recovery after injury depends on the fine-tuning polarization of microglia and astrocytes from pro-inflammatory towards anti-inflammatory phenotypes. Microglia are maintained in a surveillant state of activation through several inhibitory signaling between microglia and other cells (Frank et al., 2018).
Neurogenic niches are modified by surrounding microenvironments and pathological conditions. Indeed, neuroinflammation has been extensively reported to impair hippocampal neurogenesis (Sierra et al., 2014). In fact, neurogenesis decreases with aging, chronic stress, and neurodegenerative diseases, all conditions where neuroinflammation is a common landmark. For instance, pro-inflammatory cytokines such as interleukin (IL)-1β, tumor necrosis factor-alpha (TNFα) reduce the proliferation and survival of NSCs and ANPs (Kuzumaki et al., 2010). The recruitment of new neurons to hippocampal circuits associated with encoding spatial information is also decreased during chronic inflammation leading to cognitive impairment in rodents (Sierra et al., 2014).
Chronic neuroinflammation also generates hippocampal dysfunction altering synaptic plasticity, decreasing cognitive performance such as retention and spatial memory, and inducing depressive-like behavior (Belarbi et al., 2012). In this regard, treatment with anti-inflammatory drugs such as minocycline, cannabinoids, or TNFα inhibitors improves recognition memory evaluated by NOR and spatial memory assessed by the Y-maze (Belarbi et al., 2012; Li et al., 2016). In addition, anti-inflammatory drugs improve fear memory, reduce anhedonia measured by the sucrose preference test and decrease immobility time in the force swimming test (Troubat et al., 2021).
There is compelling evidence demonstrating that SCI induces microglial changes in rodents (Wu et al., 2014a; Jure et al., 2017, 2021, 2022). For instance, our group has described that the number of microglial cells increased during the acute phase in the hilus, molecular layer, and GCL + SGZ of the dentate gyrus in mice. However, mRNA levels of pro-inflammatory cytokines remained unaltered in this phase (Jure et al., 2022). In agreement with these results, Faden’s group has shown an increase in the number of microglial cells concurrent with the up-regulation of mRNA expression of cycle genes (cyclin A1, A2, D1) (Wu et al., 2014b). Moreover, they described that microglial cells change their morphology from ramified to hypertrophic and bushy, indicative of microglia activation. Nevertheless, coinciding with our results, mRNA levels of pro-inflammatory cytokines experimented with no modifications 7 days post-injury (Felix et al., 2012; Wu et al., 2014b).
During the acute phase, microglial cells proliferate and acquire the morphology of an active cell although there is no production of proinflammatory cytokines. These characteristics are the hallmark of primed microglia, which has been described in a number of conditions such as infection, stress, and neurodegeneration (Frank et al., 2018).
The scenario definitely changes during the chronic phase. In agreement with Faden´s results, we have shown that mRNA levels of pro-inflammatory cytokines such as IL-1β, TNFα, IL-18, and IL-6 were up-regulated. Furthermore, microglial cells presented an activated morphology displaying hypertrophic and bushy forms instead of the surveillant ramified phenotype in the Hilus, molecular layer, and SGZ + GCL (Jure et al., 2021). A further analysis using the expression of arginase 1 (ARG), an enzyme associated with a non-inflammatory profile, showed that these hypertrophic microglia in the hippocampus belonged to a pro-inflammatory phenotype after SCI (Jure et al., 2021).
Microglial activation might be due to neuron release of chemokines after SCI. In this regard, some studies have shown that CA1, CA3, and hilar neurons increased the expression of CCL2, CCR2, CCL3, and CCL21 in the chronic phase (Li et al., 2020). The effects of CCL2 and CCL21 on microglial activation and the key role of these chemokines on neuron-glia communication are wellknown (Zhang et al., 2017). On the other hand, astrocytes also play a critical role in regulating neuroinflammation, and the number of activated cells increases in the hilus, molecular layer, and SGZ + GCL after both acute and chronic SCI (Jure et al., 2022).
Neuroinflammation in the chronic phase could also be responsible for the death of hippocampal neurons since it is common to various neurological disorders such as epilepsy, degenerative diseases, and multiple sclerosis where several neurons are usually lost. In fact, pro-inflammatory microglia releases TNFα, nitric oxide, and reactive oxygen species, which produce neuronal death (Kaindl et al., 2012).
Based on this evidence, chronic neuroinflammation and the activation of hippocampal glial cells could cause neurogenesis reduction and neurodegeneration, which lead to cognitive and emotional impairment in hippocampal-dependent behaviors after SCI.
It is important to clarify that although both cognition and emotional behavior involve the hippocampus, these functions also depend on other brain regions such as the amygdala, the hypothalamus as well as the prefrontal and perirhinal cortices (Spellman et al., 2015).
Insulin Growth Factor 1 Gene Therapy for Treating the Encephalopathy Caused by Spinal Cord Injury
Gene therapy appears as an interesting option to treat CNS trauma, especially when clinical treatment implies a constant supply of any peptide. Modified associate adenovirus is used to deliver genes of interest to the brain. Delivery methods in the CNS include intraparenchymal injection (directly into the brain or spinal cord) or injection into the cerebrospinal fluid either intracerebroventricular (ICV) or intrathecal. The delivered gene can target the specific gene causing the disease or can modify the underlying pathogenic mechanism. In the second case, neurorestorative therapies are focused on attempting to restore cellular functions affected by the disease. This strategy has involved the delivery of genes that code for growth factors, such as glialderived neurotrophic factor, nerve growth factor, and IGF-1 (Sudhakar et al., 2019). Indeed, the delivery of these genes is a powerful tool for treating neurodegenerative diseases such as amyotrophic lateral sclerosis, Parkinson’s disease, and Alzheimer’s disease. In this regard, an associated adenovirus coding for glial-derived neurotrophic factor applied to the striatum and substantia nigra resulted in better clinical scores in a model of Parkinson’s disease (Sudhakar et al., 2019). In addition, IGF-1 gene therapy administered into the lateral ventricle of the amyotrophic lateral sclerosis animal model delayed motor decline and extended survival (O´Connor et al., 2015). On the other hand, for treating SCI gene therapy focuses on growth factors that enhance axonal regeneration, increase the plasticity of the spare tissue and stimulate the intrinsic regenerative programs of injured neurons in the spinal cord (Franz et al., 2012).
Given that patients present cognitive impairments, it is important to find therapies to reverse the hippocampal abnormalities described after chronic SCI. The fine-tuning polarization from pro-inflammatory towards antiinflammatory microglial phenotypes represents a potential strategy to treat the neuroinflammation that supports tertiary damage. In this regard, IGF-1 arises as a good candidate because it induces the polarization of microglial cells towards neuroprotective and anti-inflammatory phenotypes (Labandeira-Garcia et al., 2017). In addition, IGF-1 is considered a pleiotropic molecule with both neuroprotective and regenerative potential. IGF-1 has critical implications in regulating brain plasticity and it is important in maintaining axonal and dendritic morphology and improving synaptic function (Bianchi et al., 2017). IGF-1 exerts its neuroprotective actions under different conditionsin vitro
(Bellini et al., 2011) andin vivo
and it has been described as a potent anti-inflammatory molecule reducing reactive gliosis after brain injury (Labandeira et al., 2017; Morel et al., 2017). Furthermore, this factor has been used successfully as a therapeutic agent in different experimental models of neurodegeneration and neuronal damage (Pardo et al., 2016; Falomir-Lockhart et al., 2019; Herrera et al., 2021). Among the variety of functions regulated by IGF-1, metabolic functions, cell proliferation, neuron survival effects, and neurite outgrowth are significant in the context of brain damage (Zheng et al., 2017).In this regard, the use of a recombinant adenovirus vector (RAd) overexpressing the cDNA coding for rat IGF-1 (RAd-IGF-1) results in an effective approach to reduce negative outcomes related to aging, neuroinflammation, and reactive gliosis after TBI and SCI (Nishida et al., 2011; Morel et al., 2017; Falomir-Lockhart et al., 2021; Herrera et al., 2021; Jure et al., 2021).
ICV IGF-1 gene therapy has resulted in an effective route of IGF-1 administration since the RAd-IGF-1 vector transduces brain ependymal cells with high efficiency releasing IGF-1 to the cerebrospinal fluid (Herenu et al., 2007). Compelling evidence has demonstrated that this route of administration regulates glial and neuron function in the brain parenchyma (Pardo et al., 2016; Morel et al., 2017; Falomir-Lockhart et al., 2019).
Our laboratory has shown that RAd-IGF-1 gene therapy applied during the chronic phase after SCI reverts the inhibition of neurogenesis (Jure et al., 2021). Recently, as we have already mentioned, neurogenesis reduction results from the inactivation of NSCs (Jure et al., 2022). On this subject, IGF-1 enhances NSCs proliferation and differentiation by acting through the IGF-1 receptor (Yuan et al., 2015; Zhao and Zheng, 2017). These results agree with the rise in the number of DCXcells induced by IGF-1gene therapy in the aged hippocampus (Pardo et al., 2016).
Surveillance ramified microglia turns into activated hypertrophic microglia after SCI (Jure et al., 2021). This morphological transformation is accompanied by the loss of ARG expression. ARG- hypertrophic microglia is normally related to neuroinflammation, aging, and neurodegenerative diseases (Stratoulias et al., 2019). Our data clearly shows that RAd-IGF-1 therapy, applied during the chronic phase after SCI, polarizes microglia to an anti-inflammatory, neuroprotective phenotype, stimulating ARG- hypertrophic microglia to switch to ARG-expressing ramified cells (Jure et al., 2021). Curiously, in the neurogenic niche, RAd-IGF-1 administration increases the number of hypertrophic microglia, which expresses ARG. However, neuroprotective actions of hypertrophic microglia have been demonstrated (Mathieu et al., 2010; Kiyota et al., 2012). Therefore, ARGactivated microglia could release pro-neurogenic factors to neural stem cells and recover neurogenesis. In line with this result, reactive microglial cells in the striatum are increased and motor deficits are reduced by RAd-IGF-1 treatment in aged rats (Nishida et al., 2011; Falomir-Lockhart et al., 2019).
Interestingly, our laboratory has recently demonstrated that the reversion of hippocampal abnormalities after RAd-IGF-1 therapy is accompanied by the restoration of cognitive abilities. Indeed, the administration of RAd-IGF-1 during the chronic phase recovered recognition and functional working memory measured by the Y-Maze and NOR (Jure et al., 2021). These results are consistent with previous studies showing that RAd-IGF-1 gene therapy improves spatial and recognition memories in aged rats (Pardo et al., 2016; Morel et al., 2017). Correlation studies show a positive relationship between the number of ARGmicroglia, cognitive function, and neurogenesis. These results indicate a relationship between ARGmicroglia and the improvement of hippocampal functions.
Concerning IGF-1 mechanism of action, several reports have described that IGF-1 is necessary for the expression of ARG and full adoption of the microglial anti-inflammatory phenotype via the activation of the STAT6/Akt signaling pathway (Barrett et al., 2015). On the other hand, the IGF-1 receptor is expressed in different cell types beyond microglia (Martinez-Rachadell et al., 2019), thus, pleiotropic mechanisms of action should be considered.
Insulin Growth Factor 1 Therapy Associated with Traumatic Brain Injury
There is extensive literature particularly focused on TBI and its relation with impaired behavior and neuroinflammation (Kumar and Loane, 2012; Blennow et al., 2016; Hashimoto et al., 2018). Although it is beyond the aim of this work to review all the research related to TBI, we will discuss IGF-1 therapeutical approaches in this pathology.
In this regard, previous research has established that IGF-1 plays an important role in neurogenesis after TBI as conditional IGF-1 overexpression in regions of neuronal damage results in an increase in immature neuron density after cortical injury (Carlson et al., 2014), and it also improves cognitive function (Madathil et al., 2013). Nevertheless, IGF-1 based therapy used after brain injury shows different results. In a model of brain trauma, using PEG-IGF-1 administration to improve IGF-1 stability and half-life, Sama et al. (2018) have found that modified IGF-1 was not effective in ameliorating early neuronal loss after contusion. However, Santi et al. (2018) have proven that peripheral IGF-1 exogenous administration is necessary to fully restore sensorimotor function after TBI.
It is worth mentioning that in a contusion model of TBI, there is a decrease in IGF-1 serum levels after the injury that correlates with hippocampal neuron loss and spatial memory deficits (Ozdemir et al., 2012). In addition, IGF-1 overexpression inhibits apoptosis induced by various stimuli involved in TBI such as hypoxia and excitotoxicity (Madathil et al., 2015). Furthermore, IGF-1 ICV injection after a penetrating brain injury reduces cell death, hippocampal neurodegeneration and promotes neuronal survival after TBI (Madathil et al. 2013).
As we have previously mentioned, IGF-1 has pleiotropic effects in the brain, being a potent mitogen with well-described trophic and anti-apoptotic effects on neurons. IGF-1 promotes projection neuron growth, dendritic arborization, and synaptogenesis. At a mechanistic level, this peptide has pro-survival effects on damaged neurons through the PI3K-AKT pathway (Madathil et al., 2015). Seminal observations established IGF-1-AKT signaling as a key prosurvival route in neurons. Moreover, serum IGF-1 protects neurons against maladaptive inflammation by blocking the action of inflammatory cytokines (Fernandez et al., 2017).
In line with these findings, our group has reported that both ICV and peripheral IGF-1 gene therapy administration are able to modify hippocampal neuroglia (Pardo et al., 2016; Falomir-Lockhart et al., 2019). As IGF-1 is actively transported from cerebrospinal fluid to the brain parenchyma by an unknown mechanism (Guan et al., 1996; Carro et al., 2000), the ICV route is a convenient strategy to deliver IGF-1 gene therapy to the brain. Coinciding with this affirmation, ICV IGF-1 gene therapy ameliorates neuroinflammation (Nishida Neuroscience, 2011; Falomir-Lockhart 2019) on different experimental models such as aged rodents (Herenu et al., 2007; Falomir-Lockhart et al., 2019; Herrera et al., 2019, 2020) and the encephalopathy caused by SCI (Jure et al., 2021, 2022).
However, peripheral administration emerges as a less invasive route of RAd-IGF-1 delivery. Recently, we have demonstrated that intramuscular IGF-1 gene therapy enhances IGF-1 serum levels and decreases microglia reactivity after cortical stab wound injury, and prevents the concomitant cognitive impairment (Herrera et al., 2021). Similarly, IGF-1 brain increase after TBI is related to the enhanced entrance of circulating IGF-1 (Santi et al., 2018).
All these works strongly support the therapeutic use of IGF-1 based therapies (both systemic and ICV) for preventing the unfavorable outcomes of traumatic damage.
Conclusion
It is time to consider SCI as a brain neurodegenerative disease and not only as an event circumscribed to the spinal cord. Indeed, the hippocampus is deeply and chronically altered as a consequence of spinal cord damage. Alterations in these structures might lead to cognitive and mood disorders seen in rodents and even in humans. This approach is opening a new area in neurobiology since therapeutic strategies are focused on preventing secondary injury and ignoring the encephalopathy that develops at rostral sites. Future rehabilitation strategies should emphasize not only sensorimotor skills but also cognitive function and mood disorders.
In this sense, IGF-1 emerges as a new therapeutic option as it modulates microglia towards an anti-inflammatory phenotype decreasing neuroinflammation and restoring cognitive function in animal models of CNS diseases such as TBI and SCI. In addition, RAd-IGF-1 gene therapy appears as an interesting option for improving IGF-1 stability and half-life. Moreover, the intramuscular administration of RAd-IGF-1 allows extending the treatment to any neuropathology, which includes microglial alteration, neuroinflammation, and cognitive deficits.
Author contributions:
FL and MJB have designed and written the manuscript. Both authors also collected, analyzed and discussed the data, and approved the final version of the manuscript.
Conflicts of interest:
The authors declare no conflicts of interest.
Open access statement:
This is an open access journal, and articles are distributed under the terms of the Creative Commons AttributionNonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
- 中国神经再生研究(英文版)的其它文章
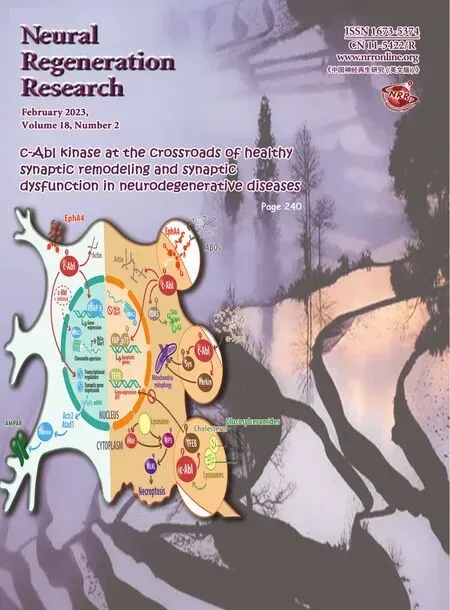
- c-Abl kinase at the crossroads of healthy synaptic remodeling and synaptic dysfunction in neurodegenerative diseases
- The mechanism and relevant mediators associated with neuronal apoptosis and potential therapeutic targets in subarachnoid hemorrhage
- Microglia depletion as a therapeutic strategy: friend or foe in multiple sclerosis models?
- Functions and mechanisms of cytosolic phospholipase A2 in central nervous system trauma
- Cre-recombinase systems for induction of neuronspecific knockout models: a guide for biomedical researchers
- Prenatal programing of motivated behaviors: can innate immunity prime behavior?