Comparison of clinical and immunological profiles in coronavirus disease 2019 and influenza patients: a case control study
Zhao-di Wang, Cong-ying Song, Da-gan Yang, Yun-mei Yang, Yuan-qiang Lu
1Department of Geriatric and Emergency, the First Affiliated Hospital of Zhejiang University School of Medicine, Hangzhou 310003, China
2Key Laboratory for Diagnosis and Treatment of Aging and Physic-chemical Injury Diseases of Zhejiang Province, Hangzhou 310003, China
3Department of Laboratory Medicine, the First Affiliated Hospital of Zhejiang University School of Medicine, Hangzhou 310003, China
Corresponding Author: Yuan-qiang Lu, Email: luyuanqiang@zju.edu.cn
The pandemic caused by the SARS-CoV-2 coronavirus is still looming worldwide, and the pandemic has challenged health care delivery and health care systems internationally.The epidemic of seasonal influenza would occur in the winter months. Since coronavirus disease 2019 (COVID-19) and influenza share many clinical symptoms,it is difficult to distinguish these two respiratory infections in the early stage.Although nucleic acid testing was the gold standard to identify different virus infected diseases, false-negative nucleic acid results were reported frequently in COVID-19,and its diagnostic sensitivity is less optimal. Therefore, the aim of our study is to explore and compare the clinical characteristics of COVID-19 and influenza, which could deepen the understanding of these two diseases and provide some guidance for clinicians to make a diff erential diagnosis.
METHODS
We recruited COVID-19 patients in the First Affiliated Hospital of Zhejiang University School of Medicine from January 20 to February 19, 2020 (COVID-19 group), and laboratory-confirmed influenza patients from January 3, 2019 to December 8, 2020 (influenza group). Exclusion criteria were: (1) patients with age ≤18 years or pregnant women; (2) patients who had received mechanical ventilation or any treatment for more than 7 d in other hospitals before admission; (3) patients having severe medical conditions, including malignant tumor, liver cirrhosis, chronic renal dysfunction, or multiple organ failure; (4) patients with immune-related diseases or long-term immunomodulatory treatment; (5) patients were not hospitalized or their treatment could not be tracked; and (6) patients with important information deficits. Laboratory data used in this study were the first inhospital results right after admission. We calculated a simplified version of clinical pulmonary infection score (CPIS) and computed tomography (CT) severity score to assess the severity degree of lung infection. Parameters with<0.05 in the univariate analysis between the two groups were considered as the candidate factors being included into the further multivariate logistic regression to identify independent risk factors of COVID-19 or influenza. Collinearity and clinical significance were also taken into consideration when selecting included variables.
RESULTS
Seventy-nine COVID-19 patients and 75 influenza patients were included in the study. As shown in Table 1, there was no significant difference in age (P=0.082)and gender (P=0.670) between the two groups. Fever,cough, and expectoration were the most common clinical symptoms. The higher proportions of patients in the influenza group presented cough and expectorationthan those in the COVID-19 group. Influenza patients also presented more proportions of headache and chill. Patients in the influenza group had a higher maximum body temperature (T) during the out-hospital phase and also a higher body temperature at hospital admission. CPIS and CT scores showed no significant difference between the two groups. We also provided information about coexisting disorders, and all of them showed no significant diff erences.
There were numerous diff erences in laboratory findings between the two groups. Patients with influenza had a higher level of monocyte and procalcitonin (PCT). Immune cell count and inflammatory factors were collected to explore the immune status of the patients. COVID-19 patients had a lower level of immune cell count than influenza patients, including total T cell (293.0 [216.0-632.0]×10/L vs. 617.0 [415.0-1,063.0]×10/L, P<0.001), CD4T cell (227.7 [130.0-300.3]×10/L vs. 366.0 [220.0-630.0]×10/L, P<0.001), CD8T cell (188.0 [117.0-225.0]×10/L vs. 246.0 [139.0-374.0]×10/L, P=0.008), and B cell count (118.3 [85.0-152.0]×10/L vs. 137.0 [96.0-216.0]×10/L, P=0.040) (Figure 1). As for inflammatory cytokines, patients with COVID-19 had higher levels of interleukin-2 (IL-2), interleukin-4 (IL-4), tumor necrosis factor alpha (TNF-α), and interferon-gamma (IFN-γ).
Nine factors, including cough, expectoration, T, monocyte, CD4T cell, CD8T cell, B cell, IL-2, and PCT were entered into multivariate logistic regression analysis to identify the independent risk factors for COVID-19 or influenza (COVID-19 was defined as 1, and influenza as 0). As shown in supplementary Table 1, we found COVID-19 patients were more prone to have lower CD4T cell counts (odds ratio [OR]=0.996, P=0.001) and higher IL-2 (OR=4.346, P<0.001). Influenza patients had a greater tendency to present expectoration (OR=0.091, P<0.001) and a higher T(OR=0.632, P=0.049).
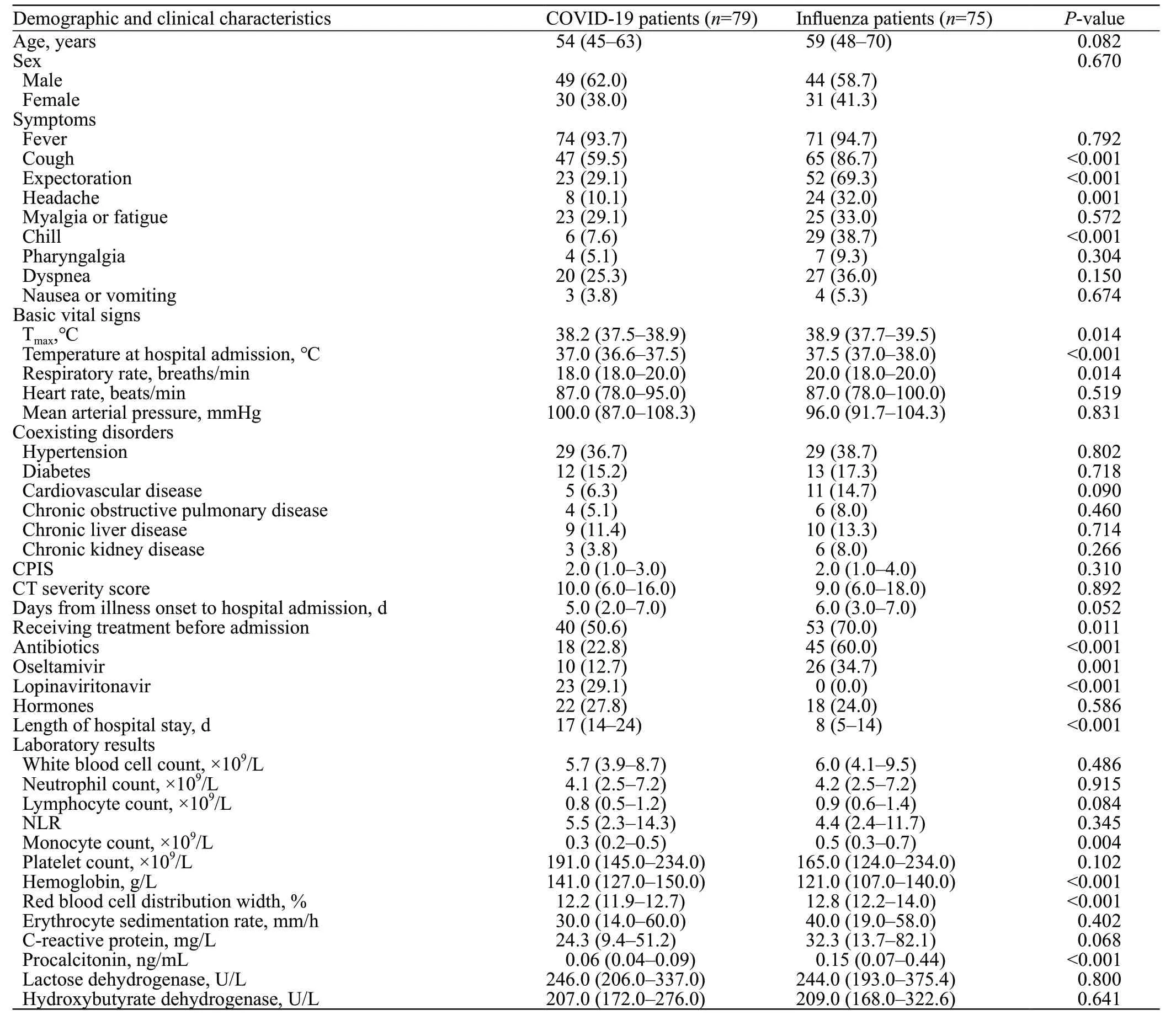
Table 1. Comparisons of characteristics between COVID-19 and influenza patients
DISCUSSION
In our study, we found more severe immune dysregulation in COVID-19 patients, presenting as immunosuppression combined with an active inflammatory response. Total T cell count, T cell subset (CD4T cell and CD8T cell), and B cell count were all lower in COVID-19 patients than in influenza patients. Among them, decreased CD4T cell was the independent risk factors for COVID-19. Existing evidence indicated that SARS-CoV-2 act on T lymphocytes, especially CD4T cells.Lymphocytes were recruited into infected sites by chemokines and cytokines to kill virus. Subsequent infection and chronic stimulation of lymphocytes might lead to T cell apoptosis and exhaustion.COVID-19 patients had higher levels of inflammatory cytokines, including IL-2, IL-4, TNF-α, and IFN-γ. The cytokine storm, a hyperactive immune presenting as a massive release of inflammatory cytokines, played an important role in the progression of COVID-19.However, it was reported that the increased levels of inflammatory cytokines in COVID-19 were significantly lower than those in previously reported patients with typical acute respiratory distress syndrome (ARDS).We also found that the elevated levels of inflammatory cytokines were limited in COVID-19, which was distinct from typical ARDS cases. For these reasons, the term cytokine storm in the mechanism of COVID-19 has been thrown into doubt. Recent studies indicated that immunosuppression, endothelial dysfunction, and direct invasion of SARSCoV-2, rather than cytokine storm, induced severe organ dysfunction and unfavorable outcomes.
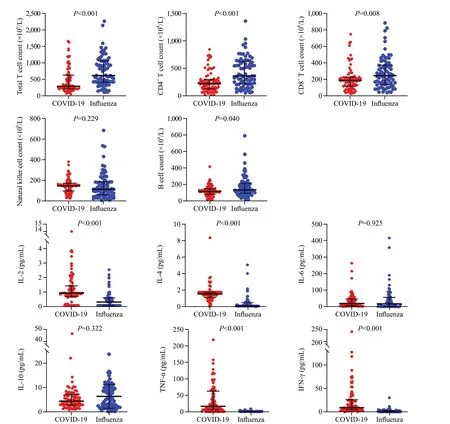
Figure 1. Immune status in coronavirus disease 2019 (COVID-19) patients and influenza patients. Immune cell counts and inflammatory cytokines were compared between COVID-19 patients and influenza patients. COVID-19 patients had lower levels of total T cell, CD4+ T cell, CD8+ T cell, B cell and higher levels of IL-2, IL-4, TNF-α, and IFN-γ than influenza patients. IL-2: interleukin-2; IL-4: interleukin-4; TNF-α: tumor necrosis factor alpha; IFN-γ: interferon-gamma.
The period of receiving medical treatments before admission was quite short in the two groups. In addition, the hormones were used in small doses and for very short periods of time (usually for 1 d or 2 d). Thus, we thought the influence brought by different intervention before admission were minimized.
There were also some limitations in our study. This was a retrospective case-control study, and selection bias might exist. To reduce this kind of bias, we selected patients strictly following the inclusion and exclusion criteria. Secondly, the sample size was limited and the single-center study might result in regional limitations.
CONCLUSIONS
Influenza patients presented more frequently cough, expectoration, headache, and chill. And influenza patients had fever with higher temperature than COVID-19 patients. More severe immune dysregulation was found in patients infected by SARS-CoV-2, presenting as immune cells exhaustion, especially CD4T cell, and active inflammatory response. These clinical findings could help clinicians distinguish these two diseases better and guide treatment.
Funding: This research was supported by a grant from the Foundation of Key Discipline Construction of Zhejiang Province for Traditional Chinese Medicine (2017XK-A3) and National Key R&D Program of China (2018YFC2001405).
Ethics approval: This study was approved by the Ethical Committee of the First Affiliated Hospital of Zhejiang University School of Medicine (code number IIT20200025A). Written informed consent was obtained from each patient or his/her authorized representatives following a full explanation of the study.
Conflicts of interests: The authors have no competing interests.
Contributors: ZDW and CYS contributed equally to this work. YMY and YQL conceived and designed the study. ZDW and CYS collected and analyzed the data. CYS and DGY contributed to the writing of the manuscript.
All the supplementary files in this paper are available at http://wjem.com.cn.
 World Journal of Emergency Medicine2022年4期
World Journal of Emergency Medicine2022年4期
- World Journal of Emergency Medicine的其它文章
- Comparing the precision of the pSOFA and SIRS scores in predicting sepsis-related deaths among hospitalized children: a multi-center retrospective cohort study
- Neutrophils inhibit CD8+ T cells immune response by arginase-1 signaling in patients with sepsis
- One-step laparoscopic pancreatic necrosectomy verse surgical step-up approach for infected pancreatic necrosis: a case-control study
- Predicting factors for the need of extracorporeal membrane oxygenation for suicide attempts by cardiac medication: a single-center cohort study
- Global research trends in cardiac arrest research: a visual analysis of the literature based on CiteSpace
- An online survey of non-compressible torso hemorrhage: training is needed
