Predicting factors for the need of extracorporeal membrane oxygenation for suicide attempts by cardiac medication: a single-center cohort study
David Vandroux , Thomas Aujoulat , Bernard-Alex Gaüzère, Bérénice Puech , Bertrand Guihard, Olivier Martinet
1Intensive Care Unit, Félix Guyon Hospital, University Teaching Hospital of La Réunion, 97400 Saint Denis, Reunion Island, France
2Cardiosurgical Intensive Care Unit, Dupuytren II Hospital, University Teaching Hospital of Limoges, 87042 Limoges, France
3UMR 1094 Neuro-épidémiologie Tropicale, University of Limoges, 87042 Limoges, France
4Cardiovascular Anesthesia Department, Félix Guyon Hospital, University Teaching Hospital of La Réunion, 97400 Saint Denis, Reunion Island, France
5Service d’Aide Médicale d’Urgence, Félix Guyon Hospital, University Teaching Hospital of La Réunion, 97400 Saint Denis, Reunion Island, France
Corresponding Author: David Vandroux, Email: vandroux.david@gmail.com
KEYWORDS: Extracorporeal membrane oxygenation; Implementation; Cardiac medication; Overdose; Predicting factor
INTRODUCTION
Several cardiovascular drugs are available for the treatment of hypertension, angina pectoris, arrhythmia, or headaches: beta-blockers (BB), calcium channel blockers (CCB), renin-angiotensin-aldosterone system blockers, digoxin and anti-arrhythmics agents. Unfortunately, these medications can also cause poisoning, which is a global public health problem. In 2018, US Poison Control Centers reported approximately 111,000 human exposures to cardiovascular drugs,corresponding to 192 fatalities for CCB and 140 fatalities for BB. The poison center of two German Länders representing 10 million inhabitants recorded 2,967 cases over ten years.Among them, 684 cases were BB single-substance exposures, including 483 suicide attempts, 144 accidental exposures and 57 cases for other reasons.
Reunion Island is a French rural overseas territory located in the southwest Indian Ocean. The French paradigm of emergency medical care is to provide advanced medical care at the scene of poisoning with a team comprised of a doctor, a nurse, and an ambulance driver. In the event of severe distress, this first medical contact informs the triage center, which coordinates admission to the hospital toward the emergency department or sometimes directly to the intensive care unit (ICU). Our ICU is the largest on Reunion Island and has developed a care network with a mobile circulatory support unit. In addition, our team coordinates the use of extracorporeal life support (ECLS) in other French hospitals throughout the Indian Ocean as well as the medevac to mainland France (Paris) for patients requiring a heart or lung transplant.
Management of patients following an overdose of cardiovascular medication can be complex, and a severe overdose can lead to significant morbidity and mortality. Sometimes intoxication requires more aggressive treatment, such as venous-arterial extracorporeal membrane oxygenation (VA-ECMO).For refractory cardiac arrest or shock, drug intoxication is independently associated with survival,and treatment with VA-ECMO could improve survival.Prompt implementations of ECMO could improve the prognosis.In the last decade, ECMO has been increasingly used for the treatment of poisoning.However, large areas of the United States, almost all rural, reported no cases.The decision to implant ECMO in cardiogenic shock is complex and based on prognostic, clinical, and biological factors. To guide this choice, the Extracorporeal Life Support Organization (ELSO) and the Department of Intensive Care of Alfred Hospital of Melbourne developed the SAVE-score to predict survival after the initiation of ECMO.However, cardiogenic shock by intoxication does not appear in this score. The characteristics of toxic cardiogenic shock are its reversibility and speed of distribution according to the peak plasma level of the toxicant. Thus, no predictive factor for the need for VA-ECMO has been described in this context. Hence, observing these clinical data could unveil crucial information that could help clinicians deliver the necessary management to patients with severe cardiac medication overdoses in a timely manner. In particular, the decision to transfer to an ECMO center should be made early. In the present study, we aim to review the clinical course and laboratory data of patients admitted to the ICU for intentional cardiac drug poisoning and identify early factors (at first medical contact or at ICU admission) that could predict the need for VA-ECMO. We hypothesized that we could identify simple predictive factors of the need for VA-ECMO. The predictors will not determine ECMO initiation but when to refer patients to an ECMO center.
METHODS
We conducted a retrospective study from January 1, 2013 to September 30, 2018 on all patients with cardiac medication overdose admitted to the adult ECMO center ICU of the University Teaching Hospital Félix Guyon in Reunion Island. Cases were defined as an overdose of the following drugs: BB, CCB, reninangiotensin-aldosterone system blockers, digoxin, and anti-arrhythmics including membrane stabilizing agents. Patients with an unintentional overdose were excluded from the analysis.
The following data were collected from medical files and were edited into a spreadsheet (Microsoft Excel 2007) by two of the authors (DV, TA): age, gender, body mass index (BMI), co-morbidities (cardiac, psychiatric or other), single or multiple drug overdoses, coingestion of others drugs including antidepressants, antiepileptics, acetaminophen or alcohol, quantity assumed to be ingested, time between ingestion and first medical contact, theoretical plasma peak and ICU admission, prehospital, emergency room and ICU admission clinical data, routine laboratory data, severity scores (Simplified Acute Physiology Score [SAPS II] based on the most abnormal parameters within 24 h of admission and Sequential Organ Failure Assessment [SOFA] score), prehospital treatments, emergency room treatments and treatments in the ICU including conventional mechanical ventilation (CMV), noninvasive positive pressure ventilation, VA-ECMO, continuous renal replacement therapy (CRRT), inotropic or vasoactive hemodynamic support, and baseline echocardiographic findings. Central nervous system dysfunction was defined as a Glasgow coma score < 14 or a seizure. The theoretical plasma peaks for each drug are given in supplementary Table 1. The first medical contact was defined as prehospital care by the emergency doctor or by the care in the emergency room if the patient was directly admitted to the hospital without prehospital management. Admission was direct if the prehospital team transferred the patient directly to the ICU without management in the emergency room. The use of catecholamines was defined as the administration of norepinephrine, epinephrine, isoprenaline, or dobutamine. The administration of intravenous calcium, glucagon, or insulin was reported.
Categorical variables were expressed as frequencies and percentages with 95% confidence intervals (95% CI). Quantitative variables were expressed as the mean with standard deviation or as the median and 1and 3quartiles, as appropriate. Missing data were omitted from the analysis and reported. Percentages were compared using Chi-square test or Fisher’s exact test, as appropriate. Quantitative variables were compared using the Mann-Whitney U test. All statistical tests were conducted at the two-tailed level of 5%. Analysis was performed using JASP 0.10.2 (University of Amsterdam, Netherlands) and GraphPad Prism 8 (GraphPad Software, USA). Our main objective was to define which early factors could predict the need for ECMO. Potential predictors with a P-value<0.05 at first medical contact were retained as candidate predictors for the multivariable analysis. At admission to the ICU, we selected the SAVE-score factors (pulse pressure, diastolic blood pressure, neurological dysfunction, metabolic acidosis) as a potential factor, as well as three criteria for routine use: heart rate, left ventricular ejection fraction (LVEF), and blood lactate levels. We did not test for delayed laboratory parameters such as creatinine or bilirubin. We then performed a logistic regression for the significant factors in univariate analysis. Multivariable logistic regression with forward stepwise selection was used to identify predictors of ECMO requirement. We compared these models based on corrected Akaike information criterion (AICc) values and chose the model with the lowest AICc value. Receiver operating characteristic (ROC) curves for independent parameters were drawn, and the areas under the ROC curves (AUROCs) were calculated. For a specific parameter, the cut-off level that resulted in the highest sensitivity and specificity was considered an optimal value for prognostication.
The study was approved by the institutional ethics committee/review board of the Comité d’éthique pour la recherche en anesthesie-réanimation (CESAR, IRB00010254-2018-169, Société française d’Anesthésie et de Réanimation), and the requirement for informed patient consent was waived in view of the retrospective nature of the study. The database of this study was registered at the Commission Nationale de l’Informatique et des Libertés.
RESULTS
A total of 60 consecutive cases with available complete medical records and diagnosed with cardiac medication overdose were hospitalized in our ICU between January 2013 and September 2018. These 60 admissions correspond to 58 patients because two patients repeated their suicide attempts during the study period. These two patients died during their second suicide attempt. Eleven admissions were excluded for non-intentional overdoses, and 49 were suicide attempts (Figure 1). The characteristics of this cohort are presented in supplementary Table 2, and the usual treatment of the patient is presented in Supplementary Table 3. In the ICU, the most commonly used treatments were norepinephrine (25, 51.0%), glucagon (17, 34.7%), epinephrine (16, 32.7%), dobutamine (12, 24.5%), isoprenaline (6, 12.2%) and temporary intravenous pacemaker (4, 8.2%). Hyperinsulinemic euglycemia therapy (HET) was administered to two patients who also required norepinephrine.

Figure 1. Flow diagram of a cohort of 60 consecutive cardiac medication overdoses admitted in ICU in Reunion island. ECLS: extracorporeal life support.
For the most severe patients, ten were implanted with ECMO. Cannulations were accomplished in a femoro-femoral configuration with cannula for distal leg perfusion and connected to a CARDIOHELP (Maquet Cardiovascular, USA). Systemic heparin was used to prevent clotting in the circuit with an objective of Xa activity between 0.2 and 0.4 U except for two patients. These two patients presented with local bleeding complications. The time between ingestion was 4 [2-7] h and the duration of ECMO was 4 [2-5] d. ECMO was started 3 [(-1)-5] h after the theoretical peak plasma level. The mean of the SAVE-score was -6, the mean survival predicted by the SAVE-score was 30%, but the observed survival was 70%. No patient died before ECMO was initiated. By comparing the VA-ECMO patients with the other cases (Table 1), the severity factors at the first medical contact were: heart rate, systolic, mean arterial pressure, and pulse pressure (PP). The best model (supplementary Table 4) combined PP and HR (AUROC=0.89) in multivariate analysis (Figure 2), but only PP appeared significant. The AUROC of the initial PP for predicting ECMO was 0.84. The cut-off point maximizing the sum of sensitivity and specificity was PP < 35.5 mmHg (1 mmHg=0.133 kPa), with 100% sensitivity (95% CI: 70%-100%) and 62% specificity (95% CI: 45%-76%). Blood-glucose measurement at first medical contact did not differ between the two groups (4.95 mmol/L vs. 8.25 mmol/L, P=0.79), but there were many missing data (67%). The severityassociated factors at admission to the ICU were: SAPS II and SOFA scores, heart rate, PP, arterial blood lactate levels, proteins level (probably as a witness of fluid therapy), transaminases, and LVEF. Measurements of arterial pressure or heart rate were less discriminating against unfavorable development than during the first medical contact, probably because treatments were already underway. In multivariate analysis, the most relevant model with the combination of LVEF, PP, and HR (supplementary Table 4) produced an AUROC of 0.90. As independent factors, the AUROCs for HR, PP, and LVEF were 0.74, 0.76 and 0.85, respectively. For LVEF, a cut-off of 50% had a sensitivity of 90% (95% CI: 59%-100%) and a specificity of 51% (95% CI: 35%-67%). LVEF < 20% and LVEF < 30% had a specificity of 97% (95% CI: 87%-100%) and 92% (95% CI: 78%-98%), respectively, to predict a severe course. For LVEF < 20%, the positive predictive value was 69%, the negative predictive value was 93%, and the Youden index was 0.47. Arterial lactate concentration and aspartate aminotransferase at admission were not significant in multivariate analysis, and the models integrating them were not sufficiently parsimonious.
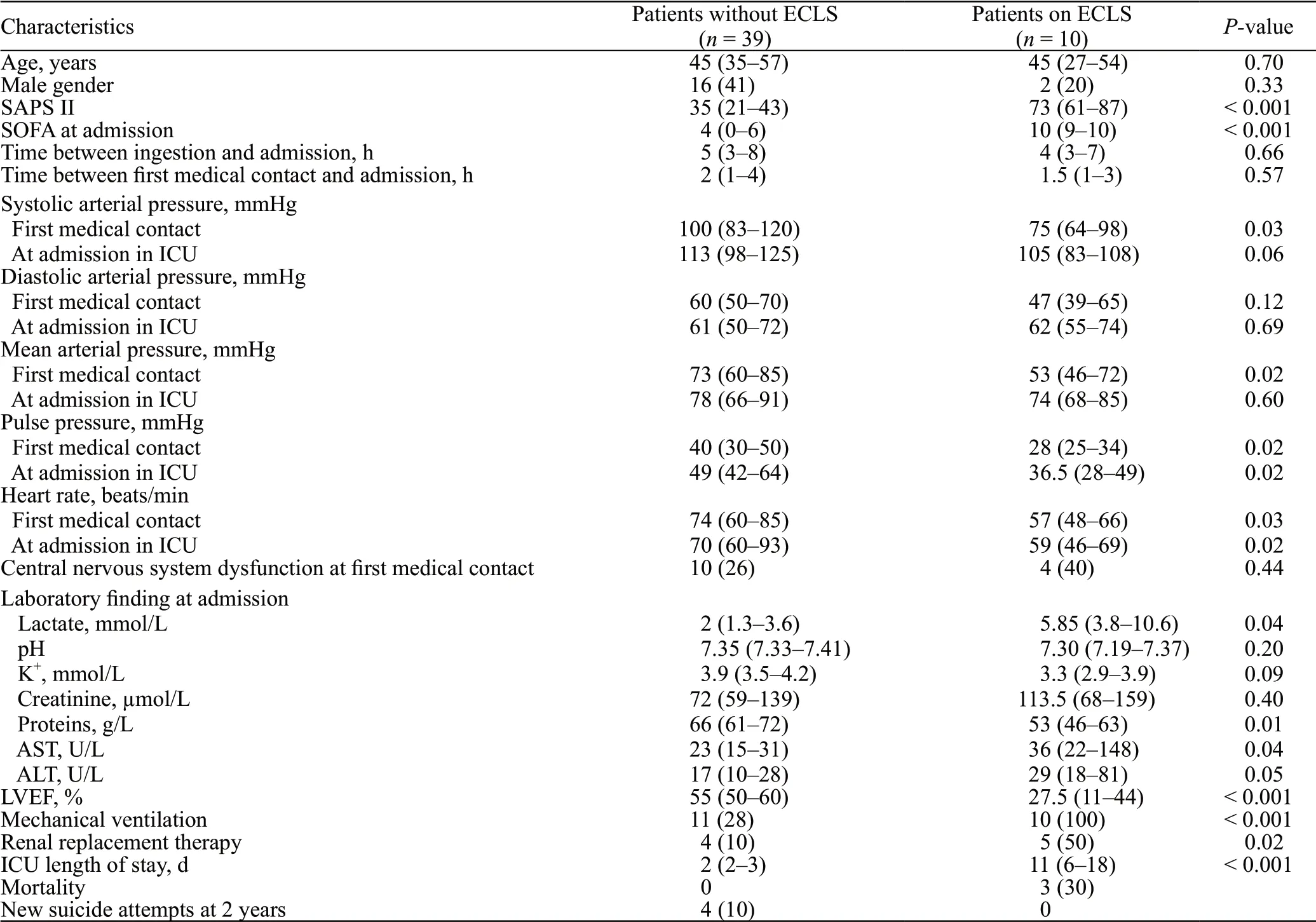
Table 1. Baseline characteristics and outcome in 49 consecutive patients after admission in ICU for cardiac drugs poisoning
The three deceased patients were poisoned with verapamil, bisoprolol-amlodipine and lercanidipineacebutolol. Pre-ECMO SOFA scores were 9, 12, and 15, respectively. One of these patients required a prehospital external cardiac massage and ECMO implanted by our mobile unit. One of the patients presented an intracavitary thrombus. The intervals between admission and death were 3, 3 and 19 d. Among the surviving patients under ECMO, one had cognitive sequelae and a leg amputation. Two other patients presented with femoral thrombosis after explantation. There were no infectious complications.
DISCUSSION
In most cases of poisoning by cardiac medication, supportive treatments and supplementation of failing organs are usually efficient, but VA-ECMO is required in patients not responding to conventional therapies.The scores predicting survival under ECMO are numerous, but predicting the need for circulatory support is more complicated. Our study aimed to provide clinicians with simple predictors to organize circulatory support before refractory cardiac arrest in this specific context. The most relevant predictive factors for VA-ECMO in our cohort were: PP at first medical contact and LVEF at admission to the ICU. PP is approximately proportional to stroke volume, i.e., the amount of blood ejected from the left ventricle during systole, and inversely proportional to the compliance of the aorta.The causes of diminution of PP are reduction of left ventricular stroke volume, severe systolic dysfunction, or aortic valve stenosis.Voluntary poisoning patients are generally young, with normal aortic compliance and without valve disease. In the context of suicide attempts with cardiac medications, the decrease in PP was thus strongly related to a decrease in preload and/or a reduction in contractility. Some drugs, especially CCB, induce vasodilation that decreases preload, so fluid therapy and a vasopressor are usually sufficient treatments. However, in our cohort, PP at the first medical contact predicted a poorer outcome than PP on admission to the ICU. We suggest that a PP < 35 mmHg at first medical contact should alert to possible ECLS.
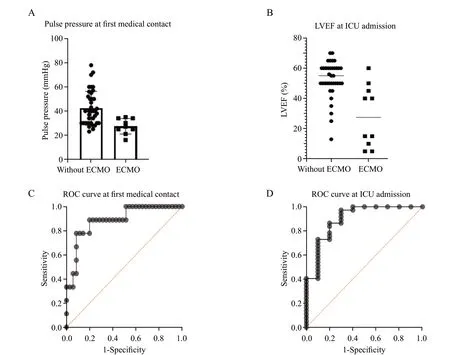
Figure 2. Prediction of extracorporeal membrane oxygenation (ECMO) requirement in intentional intoxication by cardiac medication. A: pulse pressure at first medical contact in 49 patients admitted in the Intensive Care Unit (ICU) for cardiac medication intentional poisoning; B: left ventricular ejection fraction (LVEF) by echocardiography at admission to ICU; C: receiver operating characteristic (ROC) curve of multivariate model including pulse pressure and heart rate at first medical contact. D: receiver operating characteristic curve of multivariate model including LVEF, heart rate and pulse pressure at admission in the ICU.
High blood lactate levels indicate tissue hypoxia due to increased lactate production via anaerobic glycolysis. High blood lactate levels have been correlated with fatality in acute BB poisoning.Despite significantly altered hemodynamic parameters, lactate elevation is relatively moderate on ICU admission for BB overdose, and Mégarbane et aldefined a cut-off of 3 mmol/L as a predictor of fatality. However, in our cohort, lactate concentrations could not be considered a predictor. Our cohort included several patients on metformin, which could modify the evaluation of this potential predictor.
LVEF assessed by echocardiography at admission seems to be a relevant indicator of an unfavorable outcome and ECLS initiation. Other cohorts of patients on VA-ECMO for drug intoxication revealed a mean LVEF of 18% ± 8%or LVEF< 30%.We believe that LVEF < 20% has high sensitivity and specificity to contact an ECMO center.
The use of ECMO to treat patients who have decided to take their own life and who have recalcitrant psychiatric illness or suicidality can be questionable. As ECMO is a sparse resource and with complications, the decision to offer ECMO is based on a risk/benefit assessment that includes any preexisting psychiatric comorbiditythat may limit future options and longterm outcomes. However, suicidality, even if recurrent, is not irreversible. The repeated suicide attempt rate was only 9% in our cohort, including two deaths. In our practice, any suicide attempt requires evaluation by the psychiatric team before discharge from the ICU, and twothirds of the patients followed by our tertiary hospital were transferred to the psychiatric unit to decrease the risk of suicide.
This retrospective single-center study has several limitations. The data collection was limited by the quality and completeness of the data recorded in the medical files. The missing data of the main variables were reported in supplementary Table 5. Implementation was at the discretion of the medical team in the absence of set protocols. However, as evidenced by the severity criteria, the patients were severely affected, and the patients probably would not have survived without VA-ECMO. Thus, the variability in ECMO utilization was probably insignificant. We have recorded the arterial lactate concentration on arrival at the emergency department, but these data were available for only 12 patients. The low proportion of treatment with hyperinsulinemiceuglycemic therapy or lipid emulsion may limit the relevance of our assistance decisions by ECLS. However, ECLS was implemented as an emergency in most cases, making survival unlikely under conventional treatment. Due to the missing data and the heterogeneity of the measures and drugs, we could not assess blood glucose as a predictor of severity. Nevertheless, serum glucose concentrations correlate directly with the severity of CCB intoxication.The intervals between the plasma peak and ingestion depended on the pharmacokinetic parameters of the therapeutic doses. However, the pharmacokinetic parameters could be modified according to the initial dose. Therefore, the elimination and toxicity of both amlodipine and metoprolol may be prolonged after a massive overdose and a second peak may appear depending on gastrointestinal perfusion.Finally, given our sample size and our wide confidence intervals, our results must be validated by a larger cohort.
CONCLUSION
This study supports early VA-ECMO as a therapeutic option in severe cardiac medication poisoning. It is crucial to consider ECMO before the onset of cardiac arrest. We suggest that a transfer to an ECMO center should be considered for PP < 35 mmHg at the prehospital time or LVEF < 20% at admission to the ICU. However, these results deserve to be evaluated in other cohorts of patients.
ACKNOWLEDGMENTS
The authors thank Jessica Vanderwal and Harry Flint for their translation skills and Romane Vandroux for graphic design.
Funding: None.
Ethical approval: This study was approved by the institutional ethics committee/review board of the Comité d’éthique pour la recherche en anesthesie-réanimation (CESAR, IRB00010254-2018-169, Société française d’Anesthésie et de Réanimation), and the requirement for informed patient consent was waived in view of the retrospective nature of the study.
Conflicts of interest: The authors received no financial support for the research, authorship and/or publication of this article and declare no conflict of interest.
Contributor: DV, TA, and BP collected the data. DV and TA proposed the study and wrote the first draft. All authors read and approved the final manuscript.
All the supplementary files in this paper are available at http://wjem.com.cn.
