Preterm neonate with a large congenital hemangioma on maxillofacial site causing thrombocytopenia and heart failure:A case report
lNTRODUCTlON
Hemangiomas occurring in the neonatal period are typically benign and the underlying pathogenetic mechanisms are not well characterized[1].Congenital hemangiomas(CHs)are uncommon entities[2]accounting for < 3% of all hemangiomas.CHs have a predilection for occurring in the cranio-maxillofacial region and lower limbs,while suboccipital neck,elbow,and knees are the other reported sites of occurrence[3].CH typically present within the first month of life,and exhibit an accelerated growth phase followed by involution[1].CHs develop
,are fully grown at birth,and do not show continual growth after birth[1].Thrombocytopenia,coagulation dysfunction,heart failure,and hemorrhage are some of the complications of CH[4].According to the 2019 guidelines for the diagnosis and treatment of hemangiomas and vascular malformations,CHs are classified into three types: Rapidly involuting CH(RICH),noninvoluting CH(NICH),and partially involuting CH(PICH)[5,6].NICH is rarer than RICH.Surgery is often required for NICH as conservative treatment may not yield a satisfactory outcome[3].In this work,we report a rare case of CH in the right maxillofacial region causing thrombocytopenia and heart failure.With close multidisciplinary collaboration,the CH was successfully resected with good results.
CASE PRESENTATlON
Chief complaints
A female neonate was brought to the Department of Neonatology at our hospital immediately after birth with the chief complaint of a facial tumor.
History of present illness
The gestational age of the fetus at the time of delivery was 36 wk and the mother of the patient had a cesarean scar pregnancy.The patient was delivered by cesarean section due to cephalopelvic disproportion and noninitiation of labor.Apgar scores at 1 min and 5 min were 9 and 10,respectively.The birthweight was 2630 g.Routine antenatal imaging examination performed at the gestational age of 32 wk revealed a maxillofacial tumor on the right side;the cardiothoracic area ratio of the fetus was 0.39;the superior vena cava was dilated with tricuspid regurgitation;and umbilical artery pulsatility index was 1.25.At the time of admission to our department,the neonate had not been breastfed,and had not passed meconium or urine after birth.
Gretel is not the only fairy tale sister to rescue her brother. Also read Brother and Sister and The Six Swans on SurLaLune to read tales in which sisters rescue their brothers from spells or death.
History of past illness
The past medical history of the mother was unremarkable.
Personal and family history
There was no significant family history.
Physical examination
At admission,the general state of the neonate was poor with skin cyanosis.The anterior fontanelle was flat(approximately 2.5 cm × 2.5 cm)with no tension.Physical examination revealed a 7 cm × 7 cm × 3 cm hard,tense,dull purple-colored mass at the right maxillofacial region with prominent surface telangiectasias(Figure 1A-C).The mass was warm to the touch and had a palpable thrill.The boundary of the mass was well defined and the color did not fade on application of pressure.The respiratory rate was 40 breaths/min,and the three concave sign was negative.On chest auscultation,the breath sounds were harsh with no rales or rhonchi.Apical impulse was not palpable over the precordial region.The heart rate was 149 beats/min and there were no murmurs.Abdominal wall was soft with no peristaltic wave.There was no splenomegaly or hepatomegaly and the bowel sounds were decreased.Hypomyotonia was found in four extremities,and the primitive reflexes were attenuated.The estimated gestation age was 36 wk.
She need not have worried. The moor seemed to welcome her back like a long-lost friend and her spirits rose. Taking a deep breath of the clear air, Maggie deftly8 took a bag from her pocket and started to pick, stopping every now and then to straighten her back and enjoy the familiar view. With stained fingers and scratched hands to show for her efforts, the bag slowly filled with the dark, plump fruit.

Laboratory examinations
Tumor mass ultrasound showed a huge cystic-solid mixed echo mass on the right maxillofacial region and the right neck subcutaneously.The size of the lesion was approximately 7.1 cm × 5.3 cm × 3.1 cm.The interior of the mass was filled with dense point-like low echo,and abundant blood flow signals were visible inside and around the lesion.There was no obvious abnormality in thyroid ultrasonography.
Imaging examinations
Blood parameters at admission were as follows: Hemoglobin(Hb)120 g/L(normal range 170-210 g/L);platelet count(PLT)34 × 10
/L(normal range 220× 10
-360 × 10
/L);prothrombin time(PT)17.0 s(normal range 10.1-15.9 s);thrombin time(TT)24 s(normal range 11-17 s);fibrin degradation products(FDPs)66.5 μg/mL(normal range 0.0-5.0 μg/mL);international normalized ratio(INR)1.48(normal range 0.8-1.2);D-Dimer 29.74 μg/mL(normal range 0-1 μg/mL);andthyroid-stimulating hormone(TSH)17.7 mIU/L(normal range 0.72-13.10 mIU/L).Thromboelastography findings were as follows: Alpha angle 37.2(normal range 53-72);the clot formation speed(K)6.5 min(normal range 1.0-3.0 min);and maximum amplitude(MA)35.5 mm(normal range 50-70 mm).The above results showed decreased levels of Hb and PLT and increased levels of PT and TT beyond the normal range.In addition,there was significant increase in INR,FDP,and D-Dimer levels.Alpha angle,MA,and K were also elevated above the normal range.TSH level was significantly increased.On the second day of admission,the total bilirubin levels were increased beyond the normal range,mainly indirect bilirubin.
The bed sheets that were in contact with the skin of the patient were replaced once a day.
FlNAL DlAGNOSlS
He looked at the kid again and knew what he had to do. He forced himself back into the bone?chilling cold outside to walk to his truck. He grabbed the Christmas stocking out of the cab and hurried back to the warmth of the cafe.
TREATMENT
Management of the tumor on the maxillofacial region
The temperature of the tumor was monitored and compared with that of the surrounding skin.If a temperature difference was identified,the attending physician would be informed of the situation.The position of the patient was changed every 2 h.The tumor was thoroughly examined and the presence of redness,swelling,or corrosion was evaluated;the intensity of the fluctuation of the tumor surface was carefully palpated.Since the tumor was large and close to the neck,and the neck of the newborn is short,the tumor and the neck of the patient were separated by oil gauze or silver sulfadiazine dressing.Oil gauze or silver sulfadiazine was placed over the skin around the tumor,and sterile gauze was placed on the side of the intact skin.
13.Will you give me your youngest daughter?: Here we have one of the first motifs57 which make this tale very similar to Beauty and the Beast. A beast asks for the youngest, beautiful daughter. The implication is that he wants to marry her, although a wedding ceremony is usually not acknowledged or detailed until the end of the tale once the enchantment58 has been broken.Return to place in story.
Cardiac ultrasound showed an echo separation at the oval fossa of the atrial septum approximately 2.4 mm;tricuspid regurgitation signal was detected,the area was approximately 0.9 cm
,the maximum reflux velocity was 389 cm/s,pressure gradient(Pg)was 61 mmHg,and the estimated pulmonary artery pressure was 71 mmHg.The findings suggested patent foramen ovale,which needed to be differentiated from atrial septal defect,large tricuspid regurgitation,and pulmonary hypertension(severe).Xray film indicated that the cardiac shape was full and the cardiothoracic area ratio was 0.52.
Specific treatment
Owing to the detection of anemia,thrombocytopenia,and abnormal coagulation function,40 mL cell suspension was administered within 4 h,40 mL platelet was administered within 1 h,and 40 mL plasma was administered within 4 h.Besides,oral prednisone was administered(4 mg/kg/d,divided into two equal doses)and the intended use was for 6 wk;propranolol was also administered(2 mg/kg/d,divided into two equal doses)and was adjusted based on the changes of CH.Levothyroxine was administered(7 μg/kg/d,once a day)and the dose was adjusted based on the level of TSH.Vitamin K1 was administered at 1 mg/time.Milrinone was administered
intravenous infusion(0.5 μg/kg/min for 24 h).In addition,the tumor was closely monitored for any change in the tension in order to avoid rupture.
Repeat blood tests performed on day 2 of admission showed no increase in PLT;thus,40 mL platelet and 40 mL plasma were administered along with vitamin K1,1 mg STAT.At the same time,phototherapy(intermittent blue light radiation)was administered to reduce jaundice.
On day 3 of admission,PLT had further decreased,and 40 mL platelets was administered within 1 h.
On day 7 of admission,the patient developed shortness of breath and hypouresis.Physical examination revealed increased heart rate and bilateral pitting edema in the lower extremity;in addition,liver was palpable approximately 4 cm below the rib.Therefore,digoxin(0.01 mg/kg/d,divided into two equal doses),milrinone(0.5 μg/kg/min for 24 h),and furosemide(0.5 mg/kg/time,once or twice a day)were administered.
for Rapunzel had wonderful long hair,22 and it was as fine as spun10 gold.23 Whenever she heard the Witch s voice she unloosed her plaits,24 and let her hair fall down out of the window about twenty yards25 below, and the old Witch climbed up by it.
Once upon a time there lived a man who had two sons but they did not get on at all well together, for the younger was much handsomer than his elder brother who was very jealous of him
On day 14 of admission,the patient showed stable breathing,normal volume of urine,heart rate within normal range,and no lower extremity edema;thus,digoxin and milrinone were withdrawn.
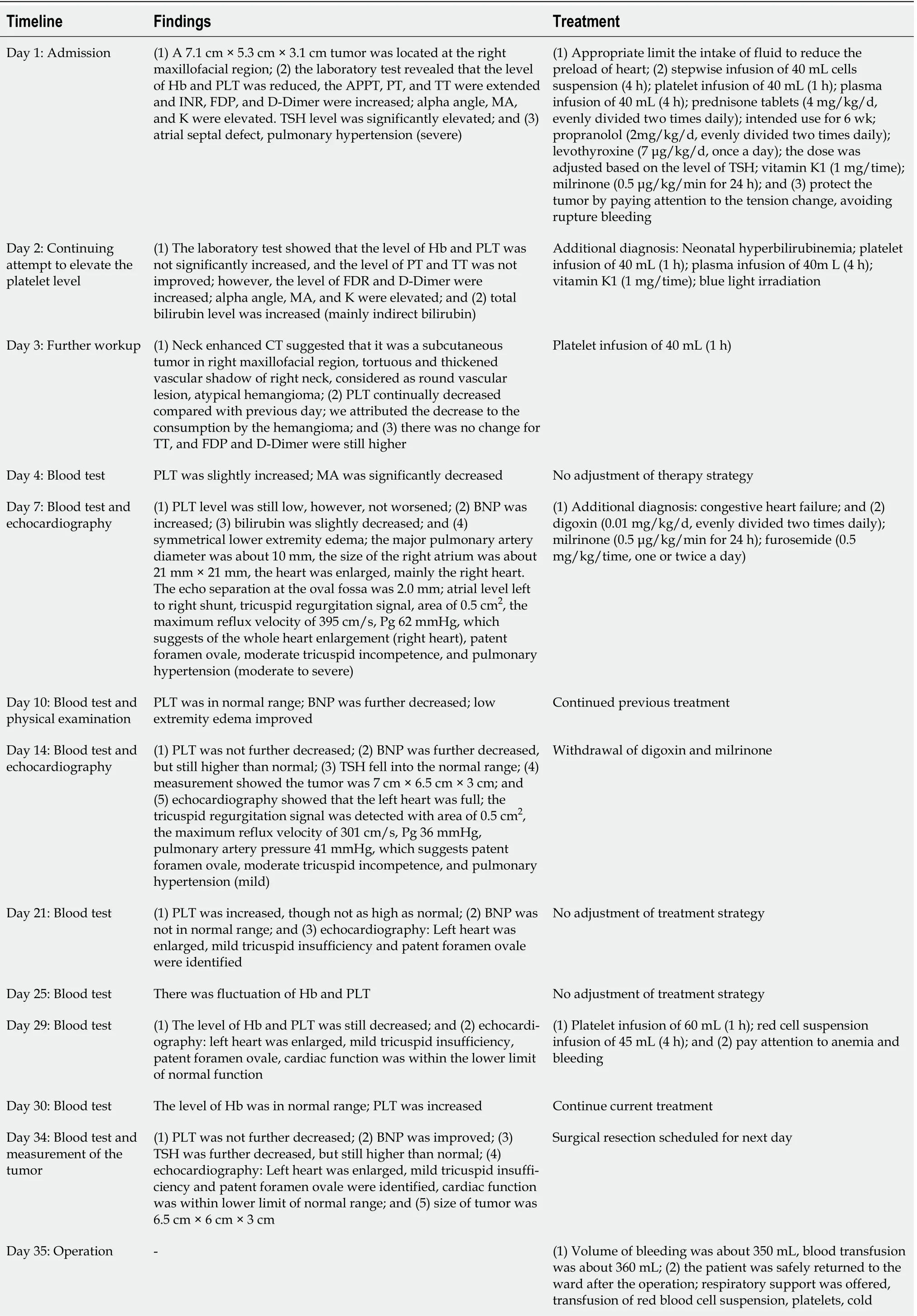
On day 44 of admission,C-reactive protein levels were within the normal range,and cefepime was withdrawn.On day 51 of admission,the laboratory indices were within the normal range;the patient had recovered and was discharged.The following treatment was prescribed at discharge:(1)Propranolol was divided into two equal doses(1.5 mg/kg/d);(2)regular monitoring of biochemical parameters,serum blood glucose levels,myocardial enzymes levels,electrocardiogram,and echocardiography;and(3)withdrawal of drugs: When the clinical evidence showed that the tumor disappeared and local B ultrasound showed tumor regression and no blood supply,gradual drug withdrawal to complete withdrawal can be considered within 1 mo(Table 1).
On day 34 of admission,there was no further decrease in PLT,and the brain natriuretic peptide level was improved.TSH level was further decreased,but still higher than the normal range.Echocardiography displayed left heart enlargement,mild tricuspid insufficiency,and patent foramen ovale.Cardiac function was within the lower limit of normal range.An operation was scheduled for the next day.
He bought a nice, big fat cat and let him stay there. The cat had a nice time hunting the mice and killing1 them. The mice could not move freely now. They were afraid that anytime the cat would eat them up.
At 4 mo of follow-up,the patient showed good prognosis.There were no adverse drug effects and no signs of recurrence after drug withdrawal.The patient showed quick recovery and her growth and development were within the normal range.
On postoperative day 1,the patient presented with coarse breath sounds and bubbling sounds in both lungs,along with worsening of lower extremity edema.Therefore,fluid intake was restricted;plus human hemoglobin was administered at 5 mL/kg once;furosemide 0.5 mg/kg/time,twice;and cefepime 30 mg/kg/time,Q12H.In addition:(1)The patient was closely monitored for blood oozing from the surgical wound and signs of impaired circulation at the surrounding skin site of the compression bandage;the color and volume of the drainage fluid was also monitored;(2)the dressing was changed every day and a compression bandage was applied;and(3)12 d after the operation,the surgical sutures were intermittently removed and 16 d after the operation,the surgical sutures were completely removed.The wound had recovered(Figure 1D).
On day 29 of admission,Hb level was 95 g/L and PLT was 19 × 10
/L;therefore,60 mL platelets was administered within 1 h,and 45 mL red blood cell suspension was administered within 4 h.
OUTCOME AND FOLLOW-UP
On day 35 of admission,the parents of the patient consented for surgical resection of the tumor.The patient was placed in the supine position.After tracheal intubation,a pillow was placed under the shoulders and the right side of the face and neck were disinfected with strong iodine and a surgical drape was placed.A giant purple-red hemangioma was seen on the right side of the face,approximately 8 cm in diameter.The skin surrounding the hemangioma showed tortuous blood vessels.There was local surface rupture and slight visible oozing.An incision was made at 2 cm from the lower margin of the tumor.There was ejection of dark red blood and a compress was used to stop bleeding.The tumor was separated along its lower margin,dissociated from the right facial artery and vein(the main blood supply vessel),ligated and disconnected.A subcutaneous incision was made 2 cm away from the edge of the tumor and the tumor was quickly removed.The bleeding was fully stopped after washing the operating cavity.The area was scraped and trimmed of facial skin and a Y-shaped suture was done.The subcutaneous tissue and skin were sutured layer by layer.A drainage tube was placed and pressure bandages were applied.The volume of intraoperative bleeding was approximately 350 mL,and 360 mL blood was transfused.The patient was safely returned to the ward after the operation.Respiratory support was provided,along with transfusion of red blood cell suspension,platelets,cold precipitation,and plasma to prevent infection.Symptomatic treatment was administered as necessary.
DlSCUSSlON
CH is rarely encountered in clinical practice.Correct diagnosis requires detailed obstetric history and antenatal color Doppler ultrasound.The intrauterine growth of the tumor should be monitored.A key characteristic of CH is that the tumor grows
,and the growth is completed after birth,which is different from common hemangiomas.It is possible to determine the blood flow and blood supply in the tumor by combining imaging with ultrasound findings.CHs need to be differentiated from teratomas,granulomas,and Kaposi-like hemangioendothelioma.
According to the 2020 diagnosis and treatment advances of CH,NICH presents as a mass with prominent round-to-ovoid shape,in variable shades of pink to purple.The lesions are well delineated and show prominent telangiectasias and central and peripheral pallor[1].The lesions are warm on palpation[4].The clinical findings of our patient are similar to those of NICH.It is important to differentiate NICH from early RICH since the treatment focus for these two hemangiomas is different.RICH is frequently treated by conservative treatment with a good prognosis(almost 100% cure)[7].RICH can also be treated by surgical resection if the patient develops complications such as thrombocytopenia,coagulation disfunction,or heart failure[8].
Seventeen summers ago, Muriel and I began our journey into the twilight1. It s midnight now, at least for her, and sometimes I wonder when dawn will break. Even the dreaded2 Alzheimer s disease isn t supposed to attack so early and torment3 so long. Yet, in her silent world, Muriel is so content, so lovable. If she were to die, how I would miss her gentle, sweet presence. Yes, there are times when I get irritated, but not often. It doesn t make sense to get angry. And besides, perhaps God has been answering the prayer of my youth to mellow4 my spirit.
It is reported that NICH can be treated with propranolol alone with no significant side effects[2];however,conservative treatment did not work for our patient[1].
The patient was diagnosed with CH accompanied with thrombocytopenia and coagulation dysfunction.Considering the large size of the tumor and presence of aberrant vessels inside the tumor,there was a risk of intravascular coagulation or local microthrombosis.Platelets were consumed after the formation of thrombus,resulting in abnormal coagulation function[4].In this setting,the conventional treatment strategy for thrombocytopenia cannot be followed.There is a need to treat the primary disease and monitor concurrent hemorrhagic diseases[8,9].
Congestive heart failure resulted from the changes in intratumoral hemodynamics and high-output heart failure was caused by an arteriovenous shunt and excessive cardiac load.Cardiac failure can occur in infants with hemangiomas > 7 cm[4,10].Our case confirms this point.In patients with congestive heart failure,due attention should be paid to fluid management.Our patient falls into the NICH type ofCH.Conservative treatment did not work in our patient and she developed heart failure;therefore,we decided to perform surgical resection.The postoperative clinical course and echocardiography findings indicated good results.Before surgical resection,we had considered topical application of ethanol to induce necrosis of local vessels in order to reduce local blood supply and cause tumor shrinkage;this would also have reduced the blood loss during surgical resection.However,local application of ethanol may cause severe side effects in neonates.There are no available reports on the application of local ethanol for the reduction of hemangioma and its effectiveness needs further data.
The patient was diagnosed with CH,prematurity,anemia,thrombocytopenia,abnormal coagulation function,atrial septal defect,pulmonary hypertension,hypothyroidism,neonatal hyperbilirubinemia,and congestive heart failure.
Close multidisciplinary collaboration was instrumental in the successful surgical resection of the large hemangioma in this patient.There was sizable intraoperative blood loss given the small blood volume of preterm neonates.Supplementing the neonate with blood products does not correct the hypovolemia;on the contrary,it is likely to cause cardiac dysfunction or renal dysfunction.Therefore,it is important for the surgeon to identify the major blood vessels after the surgeon opens the skin,in order to maintain the vitals and remove the tumor as quickly as possible.Close collaboration among experienced head and neck surgeons,experienced nurses from the Department of Neonatology,and an expert anesthesiologist can help prevent complications such as hypovolemic shock,acute renal damage or failure,and/or cerebral hypoperfusion.
CONCLUSlON
CHs are significantly different from typical hemangiomas in terms of the clinical manifestations,staging,pathology,and imaging findings.CHs are of different types,NICH,RICH,and PICH.The treatment strategies,incidence of complications,and long-term prognosis are also different.Therefore,it is crucial to determine the type of CH based on the clinical characteristics,color Doppler ultrasonography,and imaging.The treatment strategy should be guided by the specific type.Common complications of CH include intralesional hemorrhage,thrombocytopenia,abnormal coagulation function,and congestive heart failure
In our patient,we focused on limiting the liquid intake,inhibiting further growth of the hemangioma,alleviating the congestive heart failure,improving heart function,supplementing Hb,preventing bleeding,and selecting the timing for the surgery.Furthermore,close multidisciplinary collaboration,meticulous care of the tumor,surgical planning,and postoperative care were instrumental in averting postoperative complications.
FOOTNOTES
Ren N was the doctor who was in charge of the patient and contributed to the manuscript drafting;Jin CS was the surgeon of the patient and contributed to the manuscript drafting;Zhao XQ and Gao WH analyzed and interpreted the imaging findings and contributed to the manuscript drafting;Gao YX was in charge of the care of the patient and contributed to the manuscript drafting;Wang Y participated in the process of treatment and contributed to the manuscript drafting;Zhang YF was the consultant of the patient and revised and reviewed the manuscript;all authors issued final approval for the version to be submitted.
Informed written consent was obtained from the patients for the publication of this report and any accompanying images.
The authors declare that they have no conflict of interest.
The authors have read the CARE Checklist(2016),and the manuscript was prepared and revised according to the CARE Checklist(2016).
3.Mill:A mill represents the equalizing effect of fate, which provides equal justice in the same way that a mill grinds every grain without prejudice (Biedermann 221-222).Return to place in story.
This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial(CC BYNC 4.0)license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is noncommercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
China
Neng Ren 0000-0002-7298-6740;Chun-Shun Jin 0000-0002-7947-5820;Xiao-Qi Zhao 0000-0002-8308-0194;Wen-Hui Gao 0000-0001-9953-6099;Yu-Xian Gao 0000-0002-7759-6055;Yuan Wang 0000-0002-3773-7220;Yun-Feng Zhang 0000-0002-7889-3967.
Chen YL
In a tiny bay, on the opposite side of the island they found the very thing, which seemed to have been made on purpose for them; and as they were tired with their long walk, they laid themselves down on a bank of moss24 among some birches and prepared to have a good night s rest, so as to be fresh for work next day
Kerr C
However, probably because the unknown things and environment always seem attractive, I had always been distracted1 by the curiosity2 towards the foreign countries
Chen YL
1 Zhang C,Mai HM.Diagnosis and treatment advances in congenital heman-giomas.
2020;18(1): 82-86
2 Fomchenko EI,Duran D,Jin SC,Dong W,Erson-Omay EZ,Antwi P,Allocco A,Gaillard JR,Huttner A,Gunel M,DiLuna ML,Kahle KT.De novo
mutation in congenital scalp hemangioma.
2018;4[PMID: 29903892 DOI: 10.1101/mcs.a002998]
3 Li P.Congenital Hemangioma: Clinical Manifestations and Treatment.
2018;35(5): 518-526
4 Wu XY,Yang B.Research Progress on Congenital Hemangioma.
2015;21(11): 2010-2012
5 Hemangioma and vascular malformation group,Plastic Surgery Branch;Chinese Medi-cal Association.Diagnostic and therapeutic guidelines for hemangioma and vascular mal-formation.
2019;15(5): 277-304
6 Li L,Ma L.Progress in Classification of Hemangioma and Vascular Malformation.
2020;53(7): 569-572
7 Tan MJ,Yuan H,Zou Y.Compression therapy and surgical treatment of 1 case of special non-involuting congenital hemangioma.
2016;51(4): 326-327
8 Lewis D,Hachey K,Fitzgerald S,Vaidya R.Rapidly involuting congenital haemangioma of the liver.
2018;2018[PMID: 29871961 DOI: 10.1136/bcr-2018-224337]
9 Wang RQ,Zhen YJ,Za XX.Ultrasonic diagnosis of fetal facial congenital giant hemangioma : one case report.
2019;35(1): 17-19
10 Shah SS,Snelling BM,Sur S,Ramnath AR,Bandstra ES,Yavagal DR.Scalp congenital hemangioma with associated high-output cardiac failure in a premature infant: Case report and review of literature.
2017;23: 102-106[PMID: 27789620 DOI: 10.1177/1591019916669089]
 World Journal of Clinical Cases2022年17期
World Journal of Clinical Cases2022年17期
- World Journal of Clinical Cases的其它文章
- Occult hepatitis B—the result of the host immune response interaction with different genomic expressions of the virus
- Pulmonary complications of portal hypertension:The overlooked decompensation
- Ethical review of off-label drugs during the COVlD-19 pandemic
- Gut peptide changes in patients with obstructive jaundice undergoing biliary drainage:A prospective case control study
- Longitudinal assessment of liver stiffness by transient elastography for chronic hepatitis C patients
- Clinical evaluation of prone position ventilation in the treatment of acute respiratory distress syndrome induced by sepsis
