Clinical evaluation of prone position ventilation in the treatment of acute respiratory distress syndrome induced by sepsis
lNTRODUCTlON
Acute respiratory distress syndrome(ARDS)is an acute and diffuse inflammatory lung injury disease.It is usually caused by a variety of internal and external pathogenic factors,such as severe infection,trauma,and shock.Clinical manifestation may include respiratory failure,refractory hypoxemia,and respiratory distress,which can cause severe damage to the respiratory system[1,2].Mechanical ventilation is an important clinical intervention for ARDS that improves bodily oxygenation,thus improving survival rate.A lung-protective ventilation strategy has been proposed based on the clinical pathophysiology of ARDS.This strategy mainly involves limiting tidal volume and airway pressure during mechanical ventilation to avoid lung over-inflation while allowing for the partial pressure of carbon dioxide to rise within a certain range.In addition,a higher level of positive end-expiratory pressure is used to improve lung compliance,suggesting that the lung recruitment strategy should be included in the lung-protective ventilation strategy.However,during the clinical application of mechanical ventilation,it was observed that different positioning influenced the effect of the intervention.Prone position ventilation improves oxygenation by changing the patient's position and is an important auxiliary method of mechanical ventilation[3-5].However,few studies have evaluated the effect of prone position mechanical ventilation in patients with ARDS caused by sepsis,which limits its use in clinical practice.To this end,this study retrospectively analyzed the clinical data of patients with ARDS caused by sepsis treated with mechanical ventilation in the prone position and explored the effect of the intervention in this position.
MATERlALS AND METHODS
Baseline data
A retrospective analysis was performed using a sample of 102 patients who were treated with mechanical ventilation for ARDS caused by sepsis in the Intensive Care Unit(ICU)of our hospital from January 2016 to January 2020.All enrolled patients received a lung-protective ventilation treatment strategy.The patients were divided into a control group(
= 55)(undergoing routine treatment)and prone position ventilation treatment group(
= 47)based on their positions during mechanical ventilation.The inclusion criteria were as follows:(1)all patients were diagnosed with ARDS after clinical examination;this diagnosis met the 2012 Berlin Criteria[6]and was caused by sepsis;and(2)the ICU admission time ≥ 24 h.The exclusion criteria were as follows: incidence of(1)pregnancy or lactation;(2)multiple rib fractures;(3)clavicle,spine,and facial fractures;(4)intracranial hypertension;(5)severe cerebral edema;and(6)hemodynamic instability.
Research methods
Patients in the control group were treated with mechanical ventilation in the supine position combined with the lung-protective ventilation strategy while patients in the prone position ventilation treatment group were treated with prone position ventilation combined with the lung-protective ventilation strategy.The mechanical ventilation methods also included sedative and analgesic treatment with fentanyl and midazolam in both groups;patients in the prone position ventilation treatment group received this treatment only after the airway secretions were completely cleared according to the prone position protocol.The Ramsay score was calculated if the patient was beyond 4 or 5 points on the scale.A healthcare provider with extensive clinical experience stood by the patient's head to prevent movement in the central venous line and artificial airway.Two healthcare providers stood on both sides of the patient.When the tubes were properly placed,the patient was required to lean to one side in the lateral decubitus position,and the posture was changed to a prone position.Soft pillows were placed at the chest,ilium,and knees to help minimize the abdominal pressure.Subsequently,for patients with tracheal intubation,the head was tilted to one side,and for those who underwent tracheotomy,the head was placed in the middle with the arms of the patient naturally extended and placed on either side.The ventilation mode remained unchanged in the prone position,with the patient required to remain in the prone position for more than 16 h every day.It was necessary to turn the patient back to a supine position urgently if a large amount of sputum in the airway could not cleared or in cases of hemodynamic instability.Heart rate(HR),mean arterial pressure(MAP),and central venous pressure(CVP)measurements were required for hemodynamic monitoring of arterial and central venous catheterization.A Philips IntelliVue MP40 multifunctional monitor(Royal Philips,Netherlands)was selected to monitor various indicators,and color Doppler echocardiography was performed to assess the left ventricular ejection fraction(LVEF).
Observation items
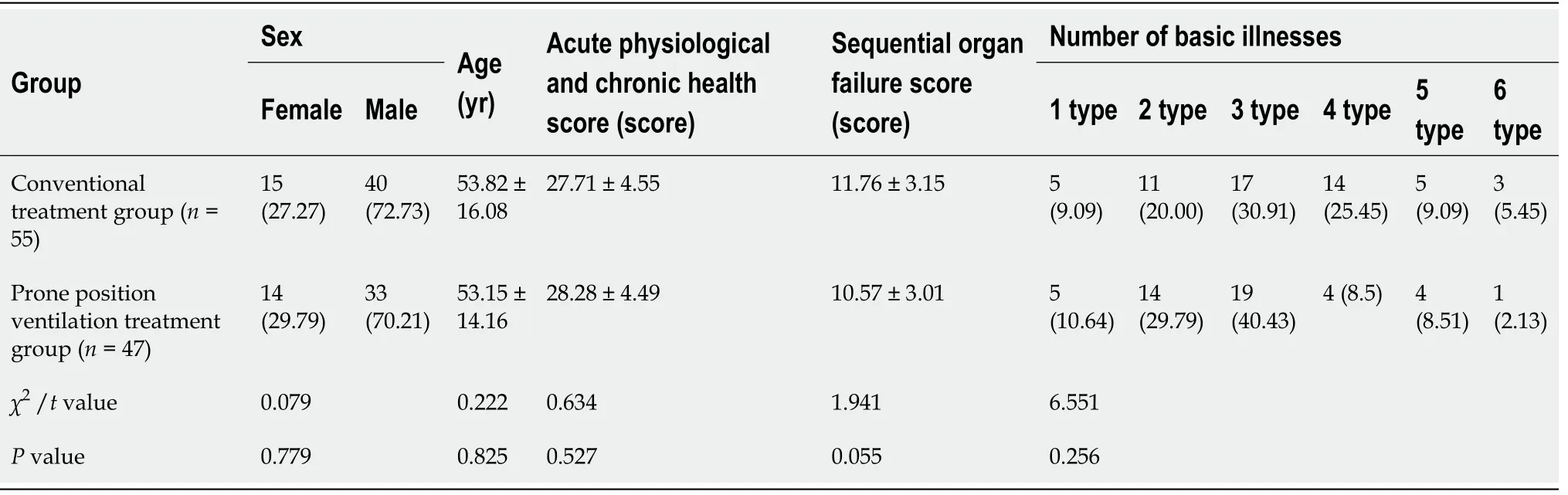
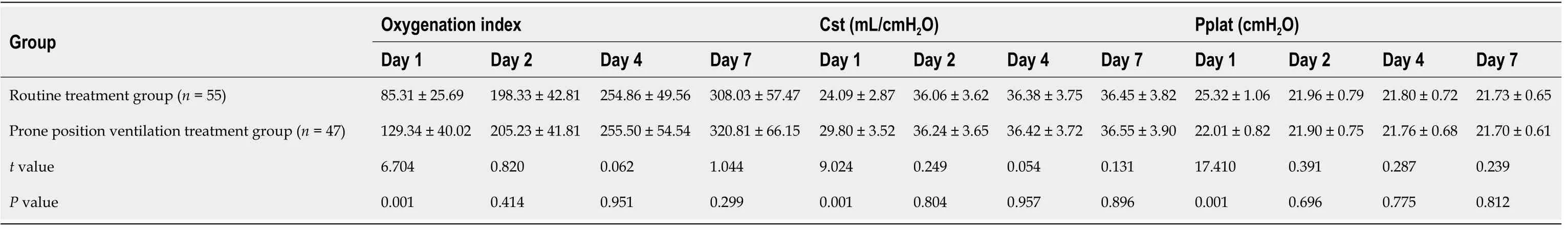
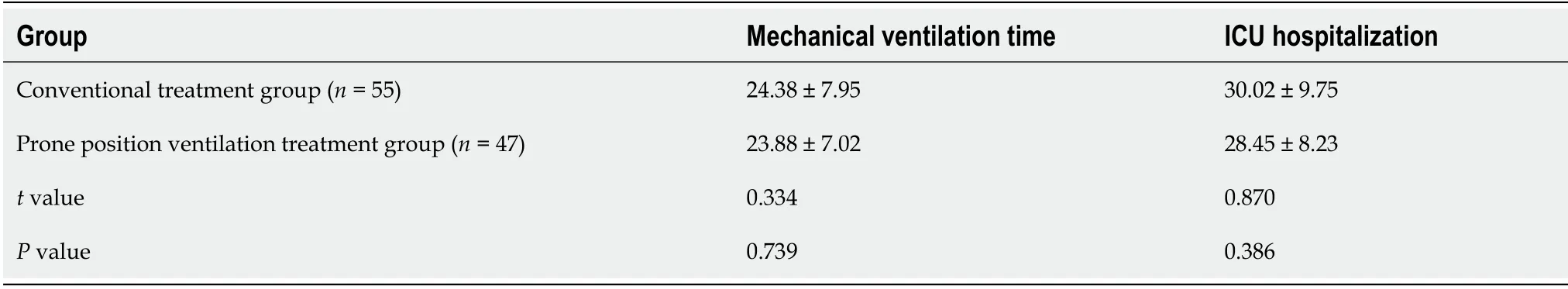
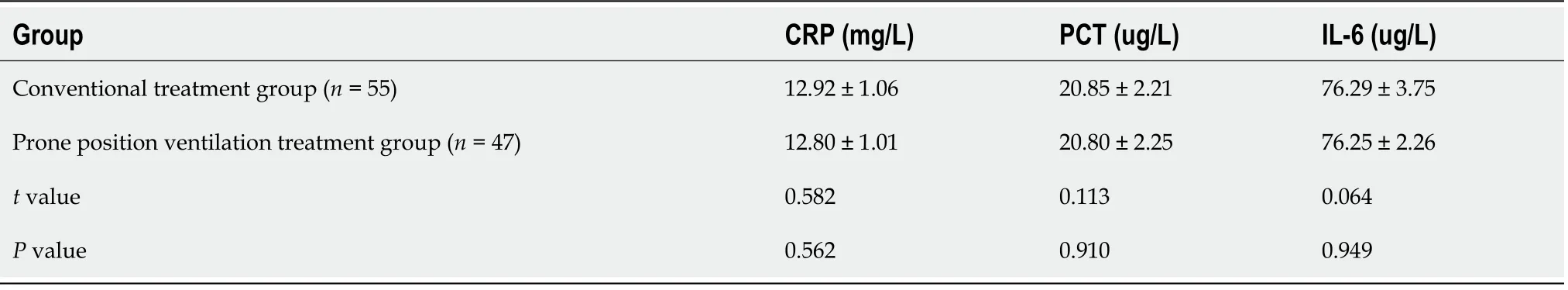
Baseline characteristics,including age,sex,acute physiological and chronic health score(score),sequential organ failure score,and number of comorbid illnesses of the patients in the two groups were compared.Next,we compared respiratory mechanical indices,such as aerobic fitness index,lung compliance(Cst),and platform pressure(Pplat)between the two groups on days 1,2,4,and 7 after ventilation.We also compared hemodynamic indices between the groups,including HR,MAP,CVP,and LVEF,one day after ventilation.Clinical outcomes were also assessed between the two groups,including duration of mechanical ventilation and ICU stay of the patients.We also compared laboratory assessments between the two groups including levels of C-reactive protein(CRP),procalcitonin(PCT),and interleukin-6(IL-6)on the first day after ventilation.Finally,the mortality rate was compared between the two groups on days 28 and 90.
There were no significant differences in duration of mechanical ventilation or length of ICU stay between the two groups(
> 0.05)(Table 4).
Statistical analysis
All statistical analyses were performed using SPSS 22.0 software.Continuous variables were summarized as means and standard deviations and compared between groups using a
-test.Categorical variables were reported as percentages,and compared between the two groups using the
test.Statistical significance was set at
> 0.05.
RESULTS
Comparison of baseline characteristics of patients between the two groups
There were no significant differences in HR,MAP,CVP,and LVEF on the first day after ventilation between the two groups(
> 0.05)(Table 3).
In contrast, a deep-learning algorithm that is meant to classify pictures as "cat" or "not cat" only needs to be given many cat pictures. It will create its own rules to determine how to detect cats in pictures and performs much better than previous methods that involved a lot of manually written features. In 2012, researchers from the University of Toronto used deep learning for the first time to win a famous computer-vision competition and improve the field by a large margin. Deep learning has since found its way into many other fields, including voice recognition, natural language processing, fraud detection and arts.
Comparison of respiratory mechanical indices of patients between the two groups on days 1,2,4 and 7 after ventilation
On the first day after ventilation,the oxygenation index and Cst in the routine treatment group were lower and the Pplat level was higher than that of the prone position ventilation group(
< 0.05).There were no significant differences in oxygenation index,Cst,and Pplat levels between the two groups on the 2
,4
and 7
day after ventilation(
> 0.05)(Table 2).
Comparison of hemodynamic indicators of patients between the two groups on the first day after ventilation
We did not observe any significant differences in baseline characteristics between the two groups(
> 0.05)(Table 1).
Comparison of mechanical ventilation time and ICU stay of patients between the two groups
39. Old witch: Belief in witches exists in nearly every culture worldwide (Leach 1949). In Jungian psychology, the witch is a personification of evil which eventually consumes itself. The witch symbolizes the destructive power of the unconscious (Luthi 1976).
Comparison of the levels of inflammatory factors in patients of each group on the first day afterventilation
There were no significant differences in the levels of CRP,PCT,and IL-6 between the two groups on the first day after ventilation(
> 0.05)(Table 5).
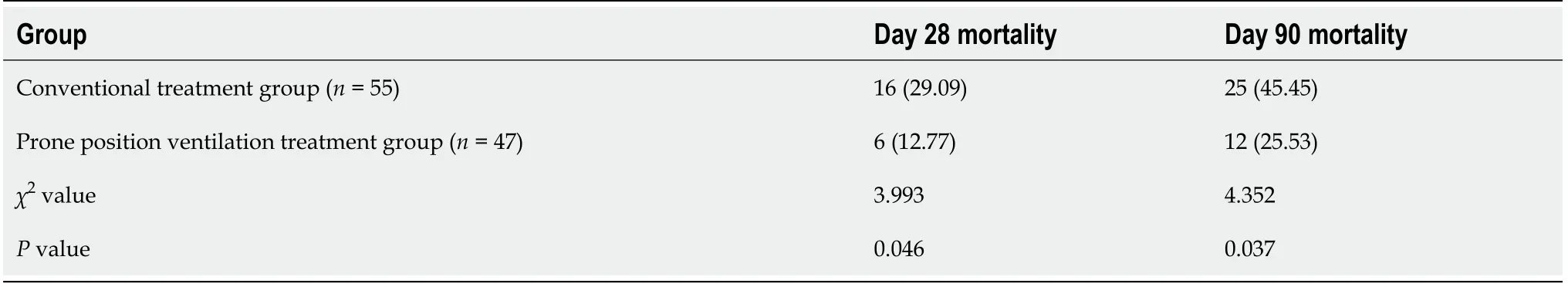
Comparison of day 28 and day 90 mortality in each group
The mortality on the 28
and 90
days was higher in the control group than in the prone position ventilation treatment group(
< 0.05)(Table 6).
A KING1 was once hunting2 in a great wood,3 and he hunted the game so eagerly that none of his courtiers4 could follow him. When evening came on he stood still and looked round him, and he saw that he had quite lost himself. He sought a way out, but could find none. Then he saw an old woman with a shaking head coming towards him; but she was a witch.5
A CERTAIN man had a donkey,2 which had carried the corn-sacks to the mill3 indefatigably1 for many a long year; but his strength was going, and he was growing more and more unfit for work. Then his master4 began to consider how he might best save his keep; but the donkey, seeing that no good wind was blowing, ran away and set out on the road to Bremen.5 There, he thought, I can surely be town-musician. 6 When he had walked some distance, he found a hound lying on the road, gasping2 like one who had run till he was tired. What are you gasping so for, you big fellow? asked the donkey.

DlSCUSSlON
ARDS is a hypoxic,progressive,and acute respiratory failure caused by indirect or direct factors.Patients may experience dyspnea and tachypnea.Arterial blood gas analysis in patients with this condition shows that all indicators fail to reach the normal level,and hypoxemia is often difficult to treat.Therefore,close attention should be paid to the correction of hypoxemia in the clinical intervention for ARDS.Symptomatic intervention using ventilation treatment with auxiliary ventilation instruments such as ventilators is common in clinical practice[7-9].ARDS is also characterized by lung injury caused by the action of local alveolar inflammatory factors on the alveoli and capillaries,resulting in increased lung permeability,exudation of substances such as plasma protein into the alveolar cavity and mesenchyme and leading ultimately to dyspnea[10,11].Therefore,correction of dyspnea is particularly important in ARDS treatment.
One day the woman stood at the window3 overlooking the garden, and saw there a bed full of the finest rampion:4 the leaves looked so fresh and green that she longed to eat them.5 The desire grew day by day, and just because she knew she couldn t possibly get any, she pined away and became quite pale and wretched. Then her husband grew alarmed and said:
The study was reviewed and approved by the ethics committee of Jiangxi Provincial People’s Hospital Affiliated to Nanchang University Institutional Review Board(Approval No.2016ED13).
Prone position ventilation can reduce the regional heterogeneity of lung ventilation and optimize the regional distribution of transpulmonary pressure in the lung,thus improving gas exchange and reducing the risk of mechanical lung injury[21].The multicenter PROSEVA trial found that the prone position significantly improved survival and shortened mechanical ventilation time compared with the supine position[22].Unlike many previous trials,the PROSEVA trial included only patients with moderate or severe ARDS(PaO
/FiO
< 150 mmHg),using prone position early in the treatment process,requiring patients to maintain a prone position for at least 16 h a day,customizing a rehabilitation plan for the patient,and using low tidal volume ventilation,which are potential necessary conditions for achieving the final therapeutic effect 3[23].Therefore,most recommendations now require patients with severe ARDS to be treated in the prone position for a long time[24].
CONCLUSlON
Prone position ventilation in patients with ARDS caused by sepsis can improve respiratory mechanics and reduce patient mortality on the first day after ventilation and does not cause significant fluctuations in patients’ hemodynamic indicators and inflammatory factor levels,thus playing an important role in ARDS treatment.
ARTlCLE HlGHLlGHTS
Research background
Previous studies have shown prone position ventilation(PPV)to be associated with improvement in oxygenation.However,its role in patients with acute respiratory distress syndrome(ARDS)caused by sepsis remains unknown.
Research motivation
This study analyzed the clinical effects of PPV in patients with ARDS caused by sepsis.
26.May not be idle: The Devil finds work for idle hands is a proverb that appeared in print in English in the early 18th century. Return to place in story.
Research objectives
The study aimed to investigate whether PPV treatment can significantly improve patients’ heart rate(HR),mean arterial pressure(MAP),central venous pressure(CVP),left ventricular ejection fraction(LVEF),mechanical ventilation time and intensive care unit(ICU)stay.And reduced post-ventilation Creactive protein(CRP),procalcitonin(PCT)and interleukin-6(IL-6)Levels and mortality.
Research methods
All enrolled patients received a lung-protective ventilation treatment strategy.The patients were divided into a control group(
= 55)(undergoing routine treatment)and prone position ventilation treatment group(
= 47)based on their positions during mechanical ventilation.Patients in the control group were treated with mechanical ventilation in the supine position combined with the lungprotective ventilation strategy while patients in the prone position ventilation treatment group were treated with prone position ventilation combined with the lung-protective ventilation strategy.HR,MAP,and CVP measurements were required for hemodynamic monitoring of arterial and central venous catheterization.The length of mechanical ventilation time and ICU stay,and levels of CRP,PCT,and IL-6 after ventilation.Finally,mortality rate was also compared between the two groups.
Research results
On the first day after ventilation,the oxygenation index and Cst were higher and Pplat level was lower in the PPV group than in the conventional treatment group.There were no significant differences in oxygenation index,Cst,and Pplat levels between the two groups on the 2
,4
,and 7
day after ventilation.There were no significant differences in HR,MAP,CVP,LVEF,duration of mechanical ventilation and ICU stay,and the levels of CRP,PCT,and IL-6 between the two groups on the first day after ventilation.There were significant differences on days 28 and 90 mortality in the PPV and control groups.
Science and Technology Plan of Jiangxi Provincial Health Commission,No.202130095.
Research conclusions
Finally,PPV was not shown to cause any adverse effects on hemodynamics and inflammation indices.
Research perspectives
We will continue to investigate the improvement effect of prone position ventilation on other pulmonary function diseases.
FOOTNOTES
Xia WH and Li QG designed this retrospective study,Xia WH and Yang CL wrote the manuscript;Xia WH,Yang CL,Chen Z,Ouyang CH and Ouyang GQ were responsible for sorting the data.
But after he had got a good breakfast, and tasted well of the king s wines, he undertook to go on guard again the third night, but he would not do it for less than the half of the kingdom, he said, for it was a dangerous post, and the king had to agree, and promise him this
Mechanical ventilation treatment for patients can improve lung volume;however,if used improperly,it can lead to excessive expansion of lung tissue,repeated opening and closing of the alveoli,and subsequently,ventilator-associated lung injury[12,13].Patients are usually in the supine position for ventilation using a ventilator.In the supine position,under the influence of gravity,the blood flow may remain distributed on the dorsal side,and the proportion of ventilated blood flow becomes imbalanced.Thus,the supine position may be ineffective for ventilation in patients with severe lung consolidation in gravity-dependent parts[14,15].In a study by Walter
[16],prone position ventilation for patients with ARDS resulted in significant improvement in lung compliance,shortening of mechanical ventilation time,and improvement in oxygenation.Therefore,Walter
[16]believed that prone position ventilation could be effective for oxygenation capacity and hypoxia.In this study,on the first day after ventilation,the oxygenation index and Cst level in the prone position ventilation treatment group were higher than those in the control group.The prone position ventilation treatment group had a lower Pplat level compared to the control group(
< 0.05).From our results,it can be inferred that the prone position may have improved oxygenation by the following mechanisms:(1)the volume of the lung tissue is reduced as it is compressed by the heart;(2)the ventilation/blood flow ratio is further improved in the prone position as compared to that in the supine position,thus significantly reducingpulmonary shunting;and(3)when the gravitational intrapleural pressure gradient is changed,the gravity-dependence of pulmonary edema fluid is redistributed.Furthermore,during prone position ventilation treatment,the curvature of the dorsal diaphragm is significantly reduced compared with that of the ventral diaphragm,which is affected by tension.When the posture of the patient changes,the pressure-forming direction of the abdominal contents also change correspondingly.In the supine position,the pressure from the abdominal contents mainly acts on the dorsal diaphragm,thus counteracting the pressure of the ipsilateral diaphragm and keeping the diaphragm position unchanged[17,18].In the prone position,the pressure acting on the dorsal diaphragm is reduced.Subsequently,the diaphragm position changes,leading to an increase in the functional residual air volume,redistribution of the air in the lungs along with the blood flow,and improvement in the ventilatory blood perfusion ratio in line with bodily requirement;thus,it is effective for the oxygenation capacity and hypoxia[19].Prone position ventilation may also impact hemodynamics[20].However,the findings of the present study showed that there were no significant changes in the hemodynamic indicators and inflammatory factor levels on the first day after ventilation in either group.In this study,the 28- and 90-day mortality were lower in the prone position ventilation group than in the control group(
< 0.05).Analysis of the results of the study reveal that the development of prone position ventilation therapy can reduce patient mortality.When patients’ oxygenation capacity is improved,conditions such as hypoxemia and respiratory failure are also significantly improved,leading to a reduced disease mortality rate.
All study participants,or their legal guardian,provided informed written consent prior to study enrollment.
The authors have nothing to disclose.
To this, the little boy reached down and rolled up his pant leg to reveal a badly twisted, crippled left leg supported by a big metal brace7. He looked up at the store owner and softly replied, “Well, I don’t run so well myself, and the little puppy will need someone who understands!”
No additional data are available.
This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial(CC BYNC 4.0)license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is noncommercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
China
Wen-Han Xia 0000-0001-5742-8591;Chun-Li Yang 0000-0001-6858-6587;Zhi Chen 0000-0002-9467-9151;Cheng-Hong Ouyang 0000-0002-7389-2527;Guo-Quan Ouyang 0000-0002-5359-1479;Qiu-Gen Li 0000-0001-9151-5453.
The Caliph and Mansor looked on in surprise for some time; but when at last she balanced herself in a picturesque39 attitude on one leg, and flapped her wings gracefully41 up and down, they could hold out no longer; a prolonged peal42 burst from each of their bills, and it was some time before they could recover their composure
Wang JL
A
Wang JL
1 Thompson BT,Chambers RC,Liu KD.Acute Respiratory Distress Syndrome.
2017;377: 562-572[PMID: 28792873 DOI: 10.1056/NEJMra1608077]
2 Nanchal RS,Truwit JD.Recent advances in understanding and treating acute respiratory distress syndrome.
2018;7[PMID: 30210781 DOI: 10.12688/f1000research.15493.1]
3 Fan E,Brodie D,Slutsky AS.Acute Respiratory Distress Syndrome: Advances in Diagnosis and Treatment.
2018;319: 698-710[PMID: 29466596 DOI: 10.1001/jama.2017.21907]
4 Mauri T,Lazzeri M,Bellani G,Zanella A,Grasselli G.Respiratory mechanics to understand ARDS and guide mechanical ventilation.
2017;38: R280-H303[PMID: 28967868 DOI: 10.1088/1361-6579/aa9052]
5 Tobin M,Manthous C.Mechanical Ventilation.
2017;196: P3-P4[PMID: 28707967 DOI: 10.1164/rccm.1962P3]
6 ARDS Definition Task Force.,Ranieri VM,Rubenfeld GD,Thompson BT,Ferguson ND,Caldwell E,Fan E,Camporota L,Slutsky AS.Acute respiratory distress syndrome: the Berlin Definition.
2012;307: 2526-2533[PMID: 22797452 DOI: 10.1001/jama.2012.5669]
7 Saguil A,Fargo MV.Acute Respiratory Distress Syndrome: Diagnosis and Management.
2020;101: 730-738[PMID: 32538594]
8 Pelosi P,Brazzi L,Gattinoni L.Prone position in acute respiratory distress syndrome.
2002;20: 1017-1028[PMID: 12412699 DOI: 10.1183/09031936.02.00401702]
9 Gattinoni L,Marini JJ,Collino F,Maiolo G,Rapetti F,Tonetti T,Vasques F,Quintel M.The future of mechanical ventilation: lessons from the present and the past.
2017;21: 183[PMID: 28701178 DOI: 10.1186/s13054-017-1750-x]
10 Spieth PM,Güldner A,Gama de Abreu M.[Acute respiratory distress syndrome : Basic principles and treatment].
2017;66: 539-552[PMID: 28677019 DOI: 10.1007/s00101-017-0337-x]
11 Yehya N,Hodgson CL,Amato MBP,Richard JC,Brochard LJ,Mercat A,Goligher EC.Response to Ventilator Adjustments for Predicting Acute Respiratory Distress Syndrome Mortality.Driving Pressure versus Oxygenation.
2021;18: 857-864[PMID: 33112644 DOI: 10.1513/AnnalsATS.202007-862OC]
12 Pham T,Brochard LJ,Slutsky AS.Mechanical Ventilation: State of the Art.
2017;92: 1382-1400[PMID: 28870355 DOI: 10.1016/j.mayocp.2017.05.004]
13 Grübler MR,Wigger O,Berger D,Blöchlinger S.Basic concepts of heart-lung interactions during mechanical ventilation.
2017;147: w14491[PMID: 28944931 DOI: 10.4414/smw.2017.14491]
14 Wang L,Li X,Yang Z,Tang X,Yuan Q,Deng L,Sun X.Semi-recumbent position versus supine position for the prevention of ventilator-associated pneumonia in adults requiring mechanical ventilation.
2016;CD009946[PMID: 26743945 DOI: 10.1002/14651858.CD009946.pub2]
15 Xin Y,Cereda M,Hamedani H,Martin KT,Tustison NJ,Pourfathi M,Kadlecek S,Siddiqui S,Amzajerdian F,Connell M,Abate N,Kajanaku A,Duncan I,Gee JC,Rizi RR.Positional Therapy and Regional Pulmonary Ventilation.
2020;133: 1093-1105[PMID: 32773690 DOI: 10.1097/ALN.0000000000003509]
16 Walter JM,Corbridge TC,Singer BD.Invasive Mechanical Ventilation.
2018;111: 746-753[PMID: 30512128 DOI: 10.14423/SMJ.0000000000000905]
17 Katz S,Arish N,Rokach A,Zaltzman Y,Marcus EL.The effect of body position on pulmonary function:A systematic review.
2018;18: 159[PMID: 30305051 DOI: 10.1186/s12890-018-0723-4]
18 Yamada Y,Yamada M,Yokoyama Y,Tanabe A,Matsuoka S,Niijima Y,Narita K,Nakahara T,Murata M,Fukunaga K,Chubachi S,Jinzaki M.Differences in Lung and Lobe Volumes between Supine and Standing Positions Scanned with Conventional and Newly Developed 320-Detector-Row Upright CT: Intra-Individual Comparison.
2020;99: 598-605[PMID: 32640453 DOI: 10.1159/000507265]
19 Smith LJ,Macleod KA,Collier GJ,Horn FC,Sheridan H,Aldag I,Taylor CJ,Cunningham S,Wild JM,Horsley A.Supine posture changes lung volumes and increases ventilation heterogeneity in cystic fibrosis.
2017;12: e0188275[PMID: 29176899 DOI: 10.1371/journal.pone.0188275]
20 Munshi L,Del Sorbo L,Adhikari NKJ,Hodgson CL,Wunsch H,Meade MO,Uleryk E,Mancebo J,Pesenti A,Ranieri VM,Fan E.Prone Position for Acute Respiratory Distress Syndrome.A Systematic Review and Meta-Analysis.
2017;14: S280-S288[PMID: 29068269 DOI: 10.1513/AnnalsATS.201704-343OT]
21 Gattinoni L,Busana M,Giosa L,Macrì MM,Quintel M.Prone Positioning in Acute Respiratory Distress Syndrome.
2019;40: 94-100[PMID: 31060091 DOI: 10.1055/s-0039-1685180]
22 Guérin C,Reignier J,Richard JC,Beuret P,Gacouin A,Boulain T,Mercier E,Badet M,Mercat A,Baudin O,Clavel M,Chatellier D,Jaber S,Rosselli S,Mancebo J,Sirodot M,Hilbert G,Bengler C,Richecoeur J,Gainnier M,Bayle F,Bourdin G,Leray V,Girard R,Baboi L,Ayzac L;PROSEVA Study Group.Prone positioning in severe acute respiratory distress syndrome.
2013;368: 2159-2168[PMID: 23688302 DOI: 10.1056/NEJMoa1214103]
23 Beitler JR,Shaefi S,Montesi SB,Devlin A,Loring SH,Talmor D,Malhotra A.Prone positioning reduces mortality from acute respiratory distress syndrome in the low tidal volume era:A meta-analysis.
2014;40: 332-341[PMID: 24435203 DOI: 10.1007/s00134-013-3194-3]
24 Fan E,Del Sorbo L,Goligher EC,Hodgson CL,Munshi L,Walkey AJ,Adhikari NKJ,Amato MBP,Branson R,Brower RG,Ferguson ND,Gajic O,Gattinoni L,Hess D,Mancebo J,Meade MO,McAuley DF,Pesenti A,Ranieri VM,Rubenfeld GD,Rubin E,Seckel M,Slutsky AS,Talmor D,Thompson BT,Wunsch H,Uleryk E,Brozek J,Brochard LJ;American Thoracic Society,European Society of Intensive Care Medicine,and Society of Critical Care Medicine.An Official American Thoracic Society/European Society of Intensive Care Medicine/Society of Critical Care Medicine Clinical Practice Guideline: Mechanical Ventilation in Adult Patients with Acute Respiratory Distress Syndrome.
2017;195: 1253-1263[PMID: 28459336 DOI: 10.1164/rccm.201703-0548ST]
 World Journal of Clinical Cases2022年17期
World Journal of Clinical Cases2022年17期
- World Journal of Clinical Cases的其它文章
- Occult hepatitis B—the result of the host immune response interaction with different genomic expressions of the virus
- Pulmonary complications of portal hypertension:The overlooked decompensation
- Ethical review of off-label drugs during the COVlD-19 pandemic
- Gut peptide changes in patients with obstructive jaundice undergoing biliary drainage:A prospective case control study
- Longitudinal assessment of liver stiffness by transient elastography for chronic hepatitis C patients
- Three-dimensional arterial spin labeling and diffusion kurtosis imaging in evaluating perfusion and infarct area size in acute cerebral ischemia
