Anterior vertebral body tethering for idiopathic scoliosis in growing children: A systematic review
lNTRODUCTlON
The management of idiopathic scoliosis (IS) in skeletally immature patients should aim at threedimensional (3D) deformity correction, without compromising the spinal and chest growth and complete lung development[1-3]. In order to achieve all these goals, besides the classic conservative treatments for IS in growing children -bracing[4-6] and serial casting - several growth-friendly surgical procedures have been introduced in clinical practice in recent years[7]. These include growing rods[8,9], Shilla procedure[10], vertebral body stapling[11], posterior dynamic deformity correction device[12] and anterior vertebral body tethering (AVBT)[11-16].
AVBT for IS correction, in skeletally immature patients, relies on the asymmetric inhibition of vertebral growth, by applying the Hueter-Volkmann principle[17-21]. Each vertebral body grows both in length,endochondral ossification, and in circumference, by appositional growth[22-25]. The subsequent compression of the growth plate on the curve convexity inhibits vertebral body growth,while the concomitant distraction on the curve concavity promotes vertebral body growth[15]. This dynamic phenomenon finally limits the curve progression and, ideally, reduces deformity without affecting spinal growth and mobility.
After preclinical studies performed in animal models[26-28], in 2010 Crawford and Lenke[16]reported the first case of an 8-year-old child, with a 40° right thoracic curve successfully managed through AVBT. In the following years, based on these encouraging results, different spinal surgeons started the use of off-label devices and the first case series describing the use of AVBT were published by Samdani[24,29].
In 2019, the US Food and Drug Administration (FDA) approved the first instrumentation system for AVBT, under a Humanitarian Device Exception, for skeletally immature patients with curves having a Cobb angle between 35° and 65°[30]. Since then, several clinical trials focusing on AVBT have been published[8-12]. However, some controversies still exist about this emerging surgical technique and few data are available about the long-term results.
This systematic review aimed to summarize the current evidence about the efficacy and safety of AVBT in the management of IS in skeletally immature patients. Particular attention was given to surgical indications, clinical and radiological outcomes, postoperative complications, re-intervention rates and conversion rates to posterior spinal fusion (PSF).
MATERlALS AND METHODS
The study was conducted with methods described in PRISMA[31]. It was registered in PROSPERO (ID:CRD42020183915) before the data extraction and analysis.
29.Assist him in herding geese: From hence we get the story s title and temporary name of the protagonist. The princess has been brought low and made a goose girl.Return to place in story.
Literature search and study eligibility
Scopus, Web of Science, Springer Link, Ovid Medline, Embase, Cochrane Library, Google Scholar and PubMed were searched from January 2014 to January 2021 to identify relevant papers for further analysis. The main keywords were: “anterior vertebral body tethering (AVBT)” or “tethering” and“scoliosis” and “growing spine” or “growing child” or “immature patients”. A manual search of the reference lists of the selected publications was also performed to identify additional studies for potential inclusion. Due to the paucity of studies on AVBT, both retrospective and prospective studies were included in the present systematic review. The following exclusion criteria were applied: (1) < 24 mo of follow-up; (2) Lack of surgical intervention description; and (3) Dropout > 20% at the final follow-up.The review was restricted to articles published in English. When multiple papers from the same centre or trial were depicted, the most thorough publication was selected. Two review authors (Bizzoca D and Piazzolla A) analysed the titles and abstracts. Potentially relevant articles were acquired for full-length text and authors were contacted when the full text was not available.
Data extraction
The preoperative workup for patients undergoing AVBT includes upstanding and supine full spine films in anteroposterior and lateral projections, supine bending films and full spine and brain magnetic resonance imaging. Buyuk[13], in a retrospective study recruiting 51 patients, confirmed preoperative bending radiographs provide a reasonable estimate of postoperative correction for patients undergoing AVBT. An increase of the major Cobb angle, however, is expected on first upstanding spine radiographs, compared to intraoperative X-rays. Spine levels are typically instrumented from upper to lower vertebra; tension should be applied on the tether, to bring the tilted discs into neutral alignment where possible[14].
AVBT should be carried out using a strict lateral decubitus position, with the convex side of the thoracic deformity facing upward, on a radiolucent table. The patient is induced under general anaesthesia,using a double-lumen endotracheal tube, thus allowing the anaesthetist to deflate the right lung (or left lung, in presence of left-sided thoracic curves) during the procedure, to access the anterior thoracic vertebral bodies. Care should be taken to protect the brachial plexus by placing a soft gel roll under the axilla[39]. The right arm should be placed on an armrest, and a soft gel pad should be used to protect the ulnar nerve. The patient is finally secured with tape. Intraoperative neuromonitoring, with somatosensory evoked potential and transcranial motor evoked potentials should be used to monitor spinal cord function during surgery and assess upper and lower extremities. All the vertebral bodies to be instrumented should be identified under fluoroscopic guidance and marked on the skin. The right lung(left lung in left-sided thoracic curves) should be deflated by the anaesthetist before starting surgery.After standard skin preparation and draping, anterior surgical access is performed; thoracoscopic, miniopen and traditional open access have been described.
Study quality assessment and bias risk of the included studies
The quality of the analysed papers was evaluated following the American Academy of Orthopedic Surgeons (AAOS) clinical practice guidelines and review methodology version 2[32]. We assessed the following features: Inclusion and exclusion criteria description; sample size and features; number of patients lost to follow-up; prognostic factors evaluation; outcome evaluation; appropriate statistical analysis; references of the study; data evaluation; presence of bias; presence of confounding factors; and follow-up duration. Based on the study design and the depicted flaws, the quality of each study included in this systematic review was defined as follows: High (< 2 flaws); moderate (≥ 2 and < 4 flaws); low (≥ 4 and < 6 flaws) and very low (≥ 6 flaws). Two authors (Bizzoca D and Piazzolla A)independently evaluated all the studies. In case of disagreement between them, a new combined evaluation was performed. Two senior authors (Moretti B and Solarino G) finally approved the quality assessment procedure. Publication bias could not be assessed by a funnel plot considering the low number of patients in each study.
Primary, secondary and tertiary outcomes
The primary outcome was to assess the success of AVBT at skeletal maturity, with a minimum 24-mo follow-up, in patients managed with this growth-friendly technique. The secondary outcome was to identify the rate of perioperative complications, re-interventions and conversions to PSF, in patients who underwent AVBT. The tertiary outcome was to depict the correct indications for AVBT and the correct preoperative workup, as well as to describe the main feature of the surgical procedure.
About a month passed. The whole thing had started to fade from my mind when the military mailboy suddenly stumbled into my office, laden15 with several sacks of packages.
RESULTS
Study selection
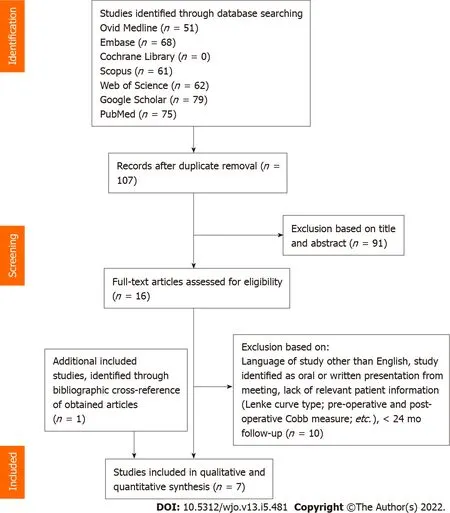
The Scopus, Springer Link, Web of Science, Ovid Medline, Embase, Cochrane Library, Google Scholar and PubMed database searches provided a total of 396 studies for potential inclusion in the review(Figure 1). After adjusting for duplicates, 107 studies remained. Of these, 91 studies were discarded after reading titles and reviewing abstracts. The full text of the remaining 16 studies was examined in greater detail. Of these, 10 studies did not meet the inclusion criteria. One additional study was identified through a bibliographic cross-reference of obtained articles. A total of seven articles were finally included in this systematic review.
She was brought to the vet to be put to sleep because her owners didn t want her anymore. I thought Minnie had a sweet personality, though. No one should judge her by her looks, I thought. So the vet spayed her and gave her the necessary shots. Finally, I advertised Minnie in the local paper: Funny-looking dog, well behaved, needs loving family.
Study quality
The process of quality assessment, performed according to the AAOS clinical practice guidelines and review methodology version 2, gave the following results: Five[14,20-23] studies out of seven (71.43%)were classified as high quality, whereas the remaining two[17,24] studies out of 10 (28.57%) were classified as moderate quality (Table 1).


Study characteristics
The features of the included papers are summarised in Table 1. Seven clinical trials,one retrospective comparative study (level III)[22], two prospective observational studies (level IV)[21,23] and four retrospective studies[14,17,20,24], recruiting 163 patients were included in the present review. Only one of the included studies (14.3%) compared the outcomes between patients managed with AVBT and a matched cohort of patients treated with PSF and instrumentation[22]. The number of patients, gender,age, minimum follow-up length, clinical and radiological outcomes at the final follow-up and the successful AVBT rate are reported in Table 1. The patients undergoing AVBT had the following scoliosis pattern distribution, according to Lenke’s classification: Lenke 1 (= 140; 85.9%), Lenke 2 (= 10;6.13%), Lenke 3 (= 3; 1.84%), Lenke 5 (= 9; 5.52%), Lenke 6 (= 1; 0.61%). A total of 151 of 163 AVBT procedures were performed in the thoracic spine, whereas the remaining 12 were in the lumbar spine.Perioperative complications, number of tether revisions and conversion to PSF of the AVBT procedures are reported in Table 2.

Main indications for AVBT
AVBT is a promising emerging technique for the surgical treatment of IS in growing patients[36]. It mainly aims for 3D correction of the scoliotic deformity, without reverting to spinal fusion or delaying the need for PSF[15,36]. In 2019, the first instrumentation system for AVBT received FDA clearance,under a Humanitarian Device Exemption, based on the results of a Phase 2A pilot study, performed by Wong[23]. Although AVBT has shown encouraging results in the treatment of IS in growing patients, there is a paucity of published data about this growth-friendly procedure and long-term results are not yet available. This systematic review aimed to summarise current evidence about the efficacy and safety of AVBT in the management of IS in skeletally immature patients.
Age and skeletal maturity
AVBT has been used in boys and girls aged mainly from 8 to 16 years. Besides biological age, however,skeletal maturity should be carefully evaluated, to estimate the potential curve progression entity, aswell as to allow the asymmetrical modulation of the spinal growth via the Hueter-Volkmann principle.The ideal skeletal age for AVBT is defined by a Risser score[33] of ≤ 2 and a Sanders score[34] of 3-4. It is important to note Sanders score has shown a strong correlation with the probability of curve progression[35], hence it should be always performed in children eligible for AVBT. Indeed, if the vertebral tethering is performed too early, a higher risk of curve overcorrection should be considered. If it is performed in an almost skeletal mature patient, there will not be enough remaining growth, thus leading to the lack of a relevant curve correction and relevant risk of tethering rupture[36].
Curve aetiology
AVBT has been proposed for idiopathic curves only, since patients with syndromic scoliosis may not respond as predictably, compared with IS. In this kind of patient, the growth of the untethered portion of the spine may be unpredictable, thus potentially increasing the re-intervention rate. Similarly, leftsided thoracic curves are not an absolute contraindication for AVBT, but the surgeon must rule out the presence of a syndromic condition, before recommending AVBT. Finally, the surgeon should be aware the left-sided approach might be high-demanding, from a technical point of view, since segmentary vessels lie closer to the aorta, compared with the right side, thus ligation could be more difficult.
Curve location, size, flexibility and 3D features
AVBT has been largely studied in idiopathic flexible thoracic curves, Lenke type 1, with a Cobb angle between 35° and 65°, according to FDA IDE criteria[37]. Published and ongoing clinical trials have also focused on other Lenke types,types 2, 3C and 5[38]; the Cobb angle for lumbar curves should be <35°. Although lumbar curves are not contraindications for AVBT, this technique has been described for thoracic curves; consequently, particular caution should be taken when performing surgery of the lumbar spine (open laparotomy or mini-laparotomy could be needed to access the lumbar spine)[39]. Furthermore, as suggested by Newton[15], tethering more than one curve potentially reduces the predictability of the outcome. Curve flexibility should be preoperatively assessed on supine bending radiographs; a curve showing a 50% flexibility is an ideal candidate for AVBT[15]. Thoracic kyphosis >40°[29] is a relative contraindication for AVBT, since this growing-friendly technique, by involving the tethering of the most anterior portion of the spine, could improve the patient’s kyphosis[39]. Finally, a careful preoperative evaluation of the patient’s sagittal profile, spinopelvic and 3D parameters can help reduce the risk of flat back or decreased lordosis[39].
Preoperative planning
Information was extracted from each study by two review authors (Bizzoca D and Piazzolla A) and finally checked by two other authors (Moretti B and Solarino G), including: (1) Characteristics of study participants (age, gender, preoperative Cobb angle); (2) Study inclusion; (3) Surgical approach; (4)Clinical outcome; (5) Radiological outcome; (6) Percentage of successful AVBT procedures; (7) Perioperative complication rate and type; (8) Re-intervention rate; and (9) Number of conversions to PSF.Disagreements were resolved by discussion between them.
Surgical technique
Although I was an avid5 New York Yankee fan one of my favorite baseball players, Roy Face was a star relief pitcher6 for the Pirates and I was hoping to get his autograph. My father bought me a brand new baseball just in case. I could hardly contain myself on the drive to Cincinnati.
PSF and instrumentation is the gold standard for the treatment of patients with scoliotic curves > 45°[40,41]. Newton[22] in a retrospective comparative study, have recently compared outcomes of patients with immature IS, who underwent AVBT, with those of a matched cohort of patients treated with PSF,at a minimum 24-mo follow-up. Although the post-intervention patient-reported outcomes (PROMs)were similar in both groups, at the final follow-up, the AVBT group had a significantly higher residual deformity, compared with patients receiving PSF (< 0.001). In the AVBT cohort, only 52% of patients were successful in having curves of < 35° at skeletal maturity. In the PSF cohort, no patient needed revision surgery, whereas in the AVBT group, five of 23 (21.74%) patients underwent one AVBT revision and the other two patients (8.7%) needed two AVBT revisions procedures. A broken tether was observed in 12 of 23 (52%) patients. Three of 23 patients needed surgical conversion to PSF and an additional three were indicated for PSF, but they had not yet undergone PSF within the study period(overall conversion rate to PSF: 26%). Finally, the proposed advantages of tethering, including progressive postoperative curve correction and maintenance of spinal motion, were not demonstrated in the AVBT group.
Although video-assisted thoracoscopy surgery (VATS) usually allows vertebral instrumentation from T4 to L2, in some cases, the diaphragmatic attachments may make the instrumentation of the vertebrae distally to T12 more technically demanding. An additional open or mini-open retroperitoneal approach is usually needed to instrument the vertebrae distally to L2. VATS is generally performed using two anterior viewing portals of 1 cm in length, placed on the anterior axillary line, and two/three posterior instrumentation portals of about 3 cm in length, placed on the posterior axillary line, overlying the vertebral bodies.
In deep dissection, the parietal pleura is opened over the spine and segmental vessels should be ligated on the convex side. Once vertebral dissection and exposure are completed, under fluoroscopic guidance, a staple and a bicortical screw are implanted in each instrumented vertebra. The entry point for the staple and the screw is just anterior to the rib head in the vertebral body. After completing all levels of instrumentation, the polyethylene cable is installed. Tension on the cable is applied on each instrumented level; care should be taken to maximally tighten the tether at the curve apex, while minimal tension should be applied at the upper and lower instrumented vertebrae, to avoid screw plough and adding-on. However, there is no consensus about the exact amount of tension to be applied.
Before wound closure, the thoracic cavity should be irrigated with saline and accurate haemostasis should be performed. The lung is reinflated, and a chest drainage tube is typically placed and set to suction. All wounds finally undergo layered sutures. The chest tube should be put on suction for 48 h with daily radiographic control; on postoperative day 3, if there is no residual pneumothorax, the tube should be put off suction and then removed on postoperative day four.
Clinical outcome and complication rates
The clinical success of AVBT is defined as the achievement of a nonprogressive scoliosis curve -Cobb angle < 35° - at skeletal maturity, avoiding PSF. Patients who needed one or more revision procedures were considered successful if they finally presented a stable curve at skeletal maturity. Only 117 of 163 (71.8%) patients carried out a nonprogressive curve at skeletal maturity. The success rate of AVBT also showed a wide heterogeneity in the analysed studies, ranging from 52%[22] to 95.24%[21].
When the King saw the snake shut itself into a room with his daughter, he said to his wife, Heaven be merciful to our child, for I fear it is all over with her now
A postoperative complication rate of 17.8% was observed, and complications were also observed in patients that achieved a successful outcome at skeletal maturity. Postoperative complications included pulmonary complications (= 12; 7.4%), including atelectasis (= 5; 3.07%), pneumonia (= 2; 1.23 %),pneumothorax (= 4; 2.45%) and chylothorax (= 1; 0.6%). All these complications were successfully managed conservatively.
Twenty-three of 163 (14.11%) patients required unplanned revision surgery within the follow-up period. The main indications for AVBT revision were: Curve overcorrection (= 11; 6.75%); broken tether with curve progression (= 8; 4.9%); adding-on (= 2; 1.23%); and progression of the untethered curve (= 2; 1.23%). Overcorrection was defined by a reduction of the preoperative Cobb angle progressing beyond the neutral axis, and was recorded as a negative number. Broken tethers, identified as a change in screw angulation > 5° on consecutive standing spine radiographs, were not an indication for revision surgery. A re-intervention was needed when curve progression was detected because of the tether breakage. Adding-on,postoperative loss of correction due to curve progression, was managed with tether extension.
Untethered curve progression is another concern of AVBT. Hoernschemeyer[20] described the combined use of thoracic tether and lumbar brace in eight patients with larger main thoracic curves and smaller lumbar curves. In this subset of patients, a significant decrease in all the three measured curves,from preoperatively to the latest postoperative follow-up was observed[20]. This therapeutic strategy,combining thoracic AVBT with a lumbar brace, could be useful in the management of scoliosis in growing children.
Conversion to PSF was performed in 18 of 163 (11%) patients during follow-up. In these patients,AVBT gave no significant advantages, since the patients could not avoid PSF surgery, within 24-mo after tethering.
AVBT versus PSF
26. Coffin of glass: Snow White in the glass coffin is like a butterfly in the chrysalis stage, awaiting to emerge as an adult. The coffin is glass so her body is on display and continues to be an object of male desire. IRReturn to place in story.
He placed the biggest and best-looking peach on the small plate in front of the girl, and then took the flawed peach and began to remove the skin. When he had half the skin off the peach he ate that side, neither of them talking, both of them just being there, and not being excited or anything—no plans, that is.
DlSCUSSlON
Currently, there is still not a universal consensus on AVBT indications, about Lenke type, curve size and remaining skeletal growth at the time of surgery. Clinical trials showed the features of the ideal patient for vertebral tethering, but the rate of postoperative complications and the lack of long-term results should be carefully considered when recommending AVBT. Krakow[30], in a retrospective analysis of 359 patients treated between 2016 and 2019 at a large paediatric centre, showed 75 patients (20.9%)could have been tethered in the years preceding approval FDA approval of AVBT device, by applying the FDA IDE criteria. Nonetheless, all the following points should be carefully assessed before considering this growth-friendly surgical procedure.
Although there is still not a universal consensus on AVBT indications, clinical trials have shown the features of the ideal patient for vertebral tethering,a skeletally immature patient, with a primary and flexible idiopathic thoracic curve. More recent clinical studies[14,17,20] have also investigated the role of AVBT in scoliosis patterns other than Lenke 1. Baker[17] in a retrospective study analysing the results of 19 AVBT procedures performed in 17 patients, compared 13 thoracic AVBT procedures to lumbar ones. The two groups had comparable demographic features in terms of gender, body mass index and skeletal age. These authors observed in lumbar AVBTs a greater immediate percentage correction and a higher correction rate per level per month compared with the thoracic cohort.Nonetheless, one revision procedure only (8%) was performed in the thoracic group, whereas three revision surgical procedures were needed in lumbar AVBT (50%).
Hoernschemeyer[20] in a retrospective study recruiting 29 patients, identified five distinct subgroups of skeletally immature patients, each receiving different treatments. Patients with a single,main thoracic curve received thoracic AVBT only. In these patients, the structural curve and both compensatory curves demonstrated continued postoperative improvement and achieved good control at the final follow-up[20]. Patients receiving thoracic AVBT and a lumbar brace also showed postoperative improvement of both curves[20]. Similar findings were observed in patients with left thoracolumbar curves and those with large main thoracic and lumbar curves treated with a combined thoracic and lumbar AVBT[20]. Finally, patients with a long thoracic curve received a single tether and exhibited a decrease in the main thoracic curve at the latest follow-up[20]. The last subgroup of patients,however, should be monitored over time since they have the largest number of consecutive levels tethered[20].
AVBT is a promising growth-friendly technique for the treatment of idiopathic scoliosis in growing patients. However, AVBT has a moderate success rate has perioperative complications, revision and conversion to PSF.
Despite AVBT being a promising growth-friendly surgical procedure, endowed with several potential advantages, it has still a lower success rate and a higher complication rate compared with PSF. Hence,the gathered data of the studies included showed AVBT was successful only in 117 of 163 (71.8%)patients. Moreover, 23 of 163 (14.11%) patients required unplanned revision surgery and 18 of 163 (11%)patients needed conversion to PSF within the follow-up period. A postoperative complication rate of 17.8% was also observed in the studies included in the present review.
This is, to the best of our knowledge, the first systematic review to investigate the effectiveness and safety of AVBT in the management of IS in growing children. The main limitation of the present study was the low level of evidence of the included studies, since no randomised clinical trials have been published on AVBT. Currently, six ongoing clinical trials are available on Clinicaltrials.gov[42]: Four prospective clinical trials focusing on AVBT and one prospective comparative nonrandomised and one randomised clinical trial are aiming to compare AVBT to PSF. The ongoing and future studies should confirm the surgical criteria for AVBT, prove tethering long-term effectiveness and safeness, focus on PROMs, and propose strategies to avoid perioperative complications and long-term implant failures. A more durable, fatigue-resistant cable should be also developed to prevent the high number of broken tethers observed in the published studies.
CONCLUSlON
The analysis of the literature included in this systematic review showed that AVBT is a promising growth-friendly technique for the treatment of IS in growing patients. However, AVBT has a moderate success rate and has perioperative complications, revision and conversion to PSF. Future level I studies,with long-term follow-up, are needed to define the limits and potentials of this emerging surgical technique.
ARTlCLE HlGHLlGHTS
Research background
Anterior vertebral body tethering (AVBT) was originally described in 2010 by Crawford and Lenke[16], who reported the first case of an 8-year-old child, with a 40° right thoracic curve successfully managed with this growth-friendly technique. In 2019, the US Food and Drug Administration approved the first instrumentation system for AVBT, under a Humanitarian Device Exception, for skeletally immature patients with curves having a Cobb angle between 35° and 65°. However, some controversies still exist in this emerging surgical technique.
Research motivation
This systematic review was designed to summarise current evidence about the efficacy and safety of AVBT in the management of idiopathic scoliosis in skeletally immature patients.
Research objectives
The objectives of this systematic review were: (1) To assess the success of AVBT at a minimum 24-mo follow-up; (2) To identify the rate of perioperative complications, re-interventions and conversions to posterior spinal fusion (PSF), in patients who underwent AVBT; and (3) To identify the correct indications for AVBT.
Research methods
The search of electronic databases was performed to identify relevant clinical studies, dealing with AVBT, for further analysis. A total of 107 studies were identified, but only seven of these were included in the present review.
Research results
The pooled data of seven studies with 163 patients showed that AVBT was successful only in 117 patients (71.8%). Moreover, 23 patients (14.11%) required unplanned revision surgery and 18 (11%)needed conversion to PSF within the follow-up period. A postoperative complication rate of 17.8% was also observed.
Research conclusions
The anterior approach to the spine needed in the vertebral tethering could be another concern. In the last decades, posterior approaches have largely replaced the anterior access to the spine, therefore several surgeons have not been trained to perform an anterior approach to the spine. However,Baroncini[18] in a retrospective study that recruited 90 patients, have recently observed that AVBT has a rapid learning curve. These authors showed intubation time and surgical time per screw decrease by > 50% for each treated patient; the estimated blood loss per screw decreased by 66% for each surgical procedure; and intubation and hospitalization decreased by 32%.
2. Tumbled out of its ears: This version of the story was sanitized for a Victorian sensibility. In the original story by Charles Perrault, the donkey s feces are gold.Return to place in story.
Research perspectives
Future studies should confirm the surgical criteria for AVBT, prove tethering long-term effectiveness and safety, focus on patient-reported outcomes measures, and propose strategies to avoid perioperative complications and long-term implant failures. A more durable, fatigue-resistant cable should be developed to prevent the high number of broken tethers observed in the published studies.
FOOTNOTES
Bizzoca D and Piazzolla A performed the research and drafted the manuscript; Solarino G and Moretti B revised the work critically; Moretti L and Vicenti G made substantial contributions to data interpretation,and all the authors approved the version to be published.
The authors declared no potential conflicts of interest concerning the research,authorship, and/or publication of this article.
The authors have read the PRISMA 2009 Checklist, and the manuscript was prepared and revised according to the PRISMA 2009 Checklist.
This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
The Cat s master did not build very much upon what he said. He had often seen him play a great many cunning tricks to catch rats and mice,15 as when he used to hang by the heels, or hide himself in the meal, and make as if he were dead; so that he did not altogether despair of his affording him some help in his miserable condition. When the Cat had what he asked for he booted himself very gallantly, and putting his bag about his neck, he held the strings of it in his two forepaws and went into a warren16 where was great abundance of rabbits. He put bran and sow-thistle into his bag, and stretching out at length, as if he had been dead, he waited for some young rabbits, not yet acquainted with the deceits of the world, to come and rummage his bag for what he had put into it.
Trint reached his truck and stopped. Somebody had written Merry X?mas, in the snow on his windshield and hung a candy cane13 on his side mirror. He wondered if it was Melinda or the boy or one of the truckers.
Italy
There was a grocery shop in a town. Plenty of mice lived in that grocery shop. Food was in plenty for them. They ate everything and spoiled all the bags. They also wasted the bread, biscuits and fruits of the shop.
A ring represents continuity, wholeness, marriage, a contract, the female genitals, power, bond, fertility, female love, justice, legitimacy, mourning, and eternity (Olderr 1986).Return to place in story.
Davide Bizzoca 0000-0002-7516-2333; Andrea Piazzolla 0000-0003-2319-2108; Lorenzo Moretti 0000-0003-0106-6215; Giovanni Vicenti 0000-0002-7412-7990; Biagio Moretti 0000-0002-1234-8616; Giuseppe Solarino 0000-0001-6325-9691.
Wang JJ
Again, I bowed in prayer. Honk10, honk, I heard. I almost jumped out of my skin. A neighbor was driving down the street. He waved at me and smiled. I waved back, happy that he cared. I quickly tried once again to settle down, repeating the familiar verse in my mind. Be still and know that I am God.
Kerr C
Wang JJ
 World Journal of Orthopedics2022年5期
World Journal of Orthopedics2022年5期
- World Journal of Orthopedics的其它文章
- Coronal plane deformity around the knee in the skeletally immature population: A review of principles of evaluation and treatment
- Update in combined musculoskeletal and vascular injuries of the extremities
- lnsufficient lateral stem contact is an influencing factor for significant subsidence in cementless short stem total hip arthroplasty
- Distal femur complex fractures in elderly patients treated with megaprosthesis: Results in a case series of 11 patients
- Prevalence and factors of work-related musculoskeletal disorders among hand surgeons
- What factors are important to new patients when selecting an orthopedic oncologist?
