Update in combined musculoskeletal and vascular injuries of the extremities
lNTRODUCTlON
A complex extremity injury that, in addition to a fracture, dislocation or even crush, involves a vascular injury represents a rare trauma pattern. It is a part of combined extremity injury or mangled extremity,and an emergency condition in which multidisciplinary approach is ato ensure life initially and limb viability secondarily[1]. Historically, control of hemorrhage following trauma has been of interest as vascular injury is a leading cause of death and disability. Moreover, limb salvage in patients with combined musculoskeletal and vascular injuries is distinctly dependent on the severity of softtissue injury, duration of limb ischemia and early, accurate diagnosis and treatment of vascular damage[2]. The management of these injuries is challenging and requires a specific algorithm of action, because they are usually characterized by increased morbidity, amputation rate, infection, neurological and functional deficits, and they could be life threatening.
The purpose of this review is to provide an update on diagnosis and treatment of combined musculoskeletal and vascular extremity injuries, from an orthopedic point of view. Combined injuries of the hand, despite possible vascular implication, are not included to this update, due to unique characteristics requiring special treatment and reconstructive pathway.
HlSTORY
For many centuries, the manipulation of any hemorrhagic scenario, especially on the battlefield, was controlled by compressive dressings, styptics, hot iron, raw ligature of vessels and improvised tourniquets[3]. The first arterial repair was performed by Dr. Hallowell in 1759 at Newcastle upon Tyne in England and the case was reported by Dr. Richard Lambert in 1761[4]. At the end of the 19century,in 1896, John B. Murphy carried out an end-to-end anastomosis at Mercy Hospital in Chicago, followed in only one decade by Alexis Carrel and Charles C. Guthrie who established other vascular operative techniques, thus providing a more refined approach in the management of vascular trauma[5-7]. Since a dry and distinct surgical field is necessary for the management of a vascular injury, the gradual widespread use of the tourniquet has greatly helped in the development of surgical techniques.Johannes Friedrich August von Esmarch who was one of the Bernhard von Langenbeck’s assistants,developed in 1873 the famous apparatus widely known as the Esmarch bandage[8,9]. Ligations and amputations have been common practice during the Balkan Wars (1911-1913), the First World War(1914-1918) and until the end of World War II (1939-1945), when the use of effective antibiotics and the presence of blood banking improved significantly vascular injury treatment options[10-12].
When the Prince did not return, poor Hyacinthia wept bitterly and changing herself from a milestone into a little blue field flower, she said, I will grow here on the wayside till some passer-by tramples51 me under foot
The time for the predominance of vascular repair over amputation was initially the Korean War(1950-1953), in which amputation rate was about 13% compared to approximately 49% that followed arterial ligation in World War II, and then the Vietnam War (1955-1975)[8,13-15]. Over the years and reaching the Iraq war, the early amputation rate was about 5%-10%[16,17]. All the techniques of vascular rehabilitation and the management algorithms of multiple-trauma patients have been further improved until early 21century (expanded Advanced Trauma Life Support protocol, utilization of tourniquet, temporary intraluminal shunts, medical air evacuation, high quality intensive care units,sophisticated pharmaceutical agents) and extended recording, statistical analysis, long-term follow-up and publishing of data in recent decades both from the battlefields (Iraq and Afghanistan) and the major urban centers provided significant help in that direction[18-22].
During the following months I watched Rebekah struggle with the ravages9 of chemotherapy. Her hospital stays became frequent and she worried about her children. Meanwhile I continued to contend with raising my own kids. They always seemed either out or holed up in their rooms. I missed the days when they were as attached to me as Rebekah s little girls were to her.
EPlDEMlOLOGY
Trauma patterns and the incidence of vascular complications differ greatly between urban centers and war zones, while the existing geographical distribution reflects the impact of high velocity weapons,motor vehicle accidents, industrialization, socioeconomic status and increasing criminality[22-24].Vascular injuries of the upper and lower extremities following trauma are relatively uncommon and represent almost 2%-3% of all civilian trauma including blunt, penetrating and gunshot injuries[24].According to Barmparas[25] vascular trauma occurs in only 0.6% of all pediatric trauma patients and in 1.6% of adults, predominantly young men (Figure 1).
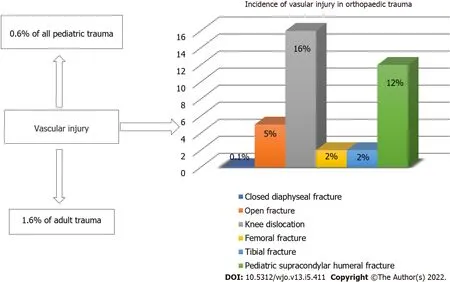
In general, the amount of energy transferred on tissues during an injury increases proportionally the possibility of vascular insult[26]. In patients with severe crush injuries associated with extensive bone(segmental shaft fracture, floating joint) and soft-tissue damage, the index of suspicion for associated arterial injury must be high. Closed diaphyseal long bone fractures carry a reported risk of vascular injury of 0.1% but open fractures have a 3.6-fold increase in the chance of vascular injury[27]. Five percent of open fractures present with a vascular injury requiring repair (type IIIc), with an amputation rate of about 16%[28]. Severe open tibial fractures are associated with a 9% incidence of vascular injury,whereas knee dislocations, especially posterior, have been associated with vascular injury in up to 16%(KD-IV > KD-V > KD-III according to Schenck classification). Femoral and popliteal artery injuries are associated with a fracture in the adjacent bone structures in a percentage of about 2% and injury of the brachial artery can occur in 8%-12% of children suffering from a supracondylar humeral fracture,usually a Gartland III fracture[21,24,26,29].
My parents searched for a cure. At that time, we did not even have a name for what I had. I suffered silently through school until I was ten years old when one in a long string of psychologists had an idea. Having discussed his plan with my parents beforehand, one day in my therapy session I was asked by the psychologist what I wanted more than anything in the world. He explained that I was going to be given an opportunity to work for what I wanted. I couldn t believe my good luck, but I could not answer. I just stood there struggling to verbalize(,) what I wanted more than anything else in the world. Finally, I was permitted to whisper the answer in my mother s ear. A horse, was all I could say.
DlAGNOSlS
Clinical presentation
Clinical diagnosis of combined vascular injuries in musculoskeletal trauma patients represents the first challenging step in an overall demanding treatment pathway. Physical examination is not always able to detect a limb-threatening injury in the absence of obvious signs of vascular impairment[26].
Given the fact that these injuries are in the context of major trauma, in polytrauma patients, the initial approach is performedthe well-established Advanced Trauma Life Support (ATLS) protocols[30]. In case of major bleeding, direct pressure, potential tourniquet application and resuscitation are the initial actions according to ATLS principles. After initial resuscitation and primary evaluation, a detailed clinical examination with neurological and vascular status documentation, is performed during the patient’s secondary evaluation. In this step, palpation of distal pulses, extremity color and temperature,time required for skin capillary refill in the distal digits, and sensory and motor deficits are assessed,compared with the contralateral limb, and recorded. Reassessment is required after any intervention,manipulation, or reduction maneuver to exclude secondary provoked vascular injury[31]. However,high index of suspicion and low threshold for vascular imaging is required because vascular injury might be present in the first place, with normal pulse palpation in a rate of 5%-15%[32].
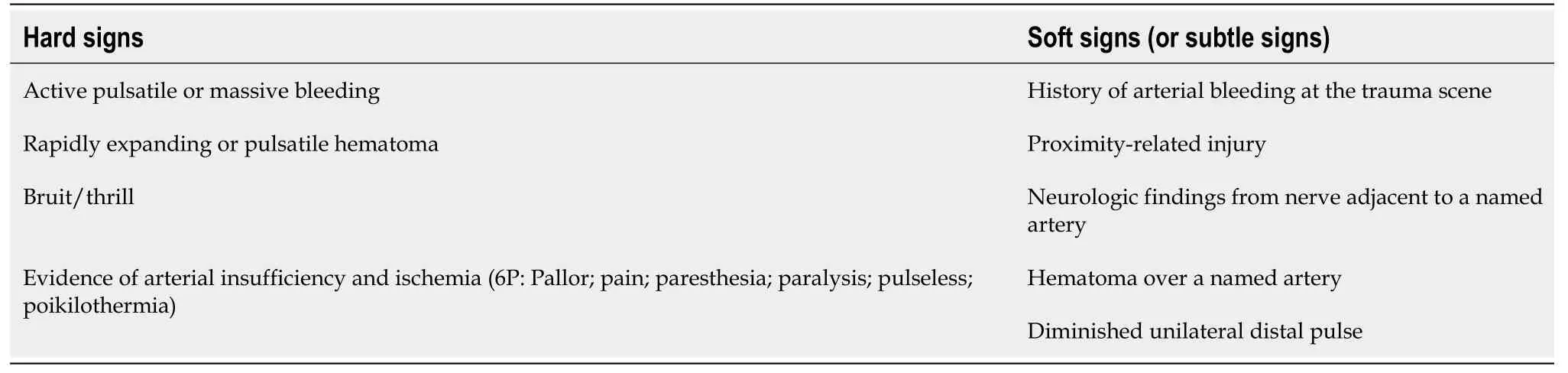
To establish an objective approach and clinical criteria for further treatment, findings of the physical examination are classified into hard and soft signs of extremity for vascular injury (Table 1). Hard signs include massive bleeding, presence of rapidly expanding hematoma, detection of one classic sign of arterial occlusion (6Ps: Pulselessness, pallor, paresthesia, pain, paralysis and poikilothermia), palpable thrill or audible bruit[33]The presence of hard signs has 92%-95% sensitivity for incidence of vascular injuries requiring surgical intervention with a positive predictive value of 95%[34,35]. In these cases,immediate operative intervention - injury site exploration in the presence of any hard sign - is strongly suggested by the literature without further delay for additional advanced vascular imaging [computed tomography (CT) or conventional angiography] (Figure 2)[36,37]. Soft signs for vascular injury include history of arterial bleeding at the accident scene or during transit to the hospital, proximity of penetrating or blunt injury to an artery of the limb, small, no pulsatile hematoma over a named artery,and presence of neurological deficit affecting nerves with proximity to a named artery. In these cases,incidence of vascular injuries ranges from 3% to 25%depending on which one or which soft sign combination exists (Figure 2)[38,39].
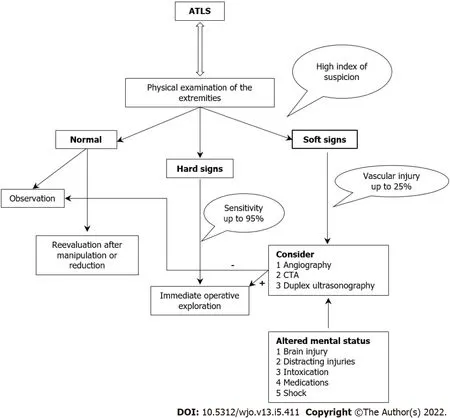
Besides physical examination, an arterial pressure index (API) or injured extremity index (IEI)(analogous to the ankle-brachial index - ABI) should be performed. The API/IEI is the ratio of the highest systolic occlusion pressure in the injured extremity at the level of the dorsalis pedis, posterior tibial or radial/ulnar arteries divided by the systolic pressure in a proximal vessel in an uninjured extremity (most often the brachial artery)[40,41]. Normal API values (> 0.9) are highly specific for exclusion of vascular injury in cases of blunt and penetrating injuries, making further vascular imaging unnecessary[42,43]. In cases with diminished peripheral pulses or API < 0.9 an imaging study, typically arteriography, should be performed.
But I did. I was so weak my legs trembled. I could never have crossed that squirming deck if Benny hadn t supported me. The kid was stronger than he looked. He helped me down the steps and steered12 me to the bench where Dad was sitting with his head drooping13 on his chest.
Special consideration is required in cases of older diabetic patients with pre-existing peripheral vascular compromise, due to possible Monckeberg’s medial calcific sclerosis with clinically false normal API index of ≥ 1[44]. Recent literature, however, demonstrates high accuracy and good agreement ofankle-brachial index duplex ultrasonography in patients with type 2 diabetes and peripheral artery disease[45].
A specific, well known, clinical scenario is the knee dislocation and its association with popliteal artery injury. In these cases, clinical examination should include assessment of the stability of the knee joint, as laxity may suggest presence of a knee dislocation with spontaneous reduction. For further advanced imaging, current literature data are conflicting, with many authors advocating low threshold for vascular imaging in such an injury pattern and others being against routine imaging after spontaneous or performed reduction of a knee dislocation if normal pulses are present[38,46].
Supracondylar fractures represent another well-known clinical scenario. These fractures are of the most common traumatic fractures seen in children aged 5-7 years, with the urgency depending on whether the hand remains perfused or not, as rich collateral circulation may be sufficient despite vascular injury. In the case of absent distal pulses in supracondylar fractures of the humerus in children,the decision to explore is based on quality of extremity perfusion rather than absence of pulse.Generally, a well-perfused extremity is warm and pink in contrast to a poorly perfused extremity that is cold and pale with an arterial capillary refill > 2 s. Some studies recommend early aggressive surgical intervention for both patterns of vascular compromise in order to prevent limb loss and serious longterm complications such as Volkmann’s ischemic contracture[21,24,25,29].
Imaging
Imaging modalities used in the diagnosis of vascular injuries in musculoskeletal trauma include conventional angiography, computed tomography angiography (CTA) and duplex ultrasound. Conventional catheter-based angiography provides accurate diagnosis of arterial injuries, even in minor injuries such as intimal tears, after intra-arterial or intravenous contrast agent injection[47,48]. As conventional angiography has several disadvantages such as cost, delay, need of specialized team, and possible renal toxicity, it is currently preserved for intraoperative use and not for routine imaging at an Emergency Department basis[49].
Then she seized Hansel with her bony hand and carried him into a little stable, and barred the door on him; he might scream as much as he liked, it did him no good
Limb salvage in patients with combined musculoskeletal and vascular injuries is distinctly dependent on the severity of soft-tissue injury, the duration of limb ischemia and the early, accurate diagnosis and treatment of vascular damage. In general, the amount of energy transferred on tissues during an injury increases proportionally the possibility of vascular insult[26]. In patients with severe crush injuries associated with extensive bone (segmental shaft fracture or floating joint) and soft-tissue damage, the index of suspicion for associated arterial injury must be high. Closed diaphyseal long bone fractures carry a reported risk of vascular injury of 0.1% but open fractures have a 3.6-fold increase in the chance of vascular injury[27]It is therefore clear that the basic principle of early detection of a potentially catastrophic vascular lesion in orthopedic trauma must be secured in advance with the high degree of suspicion on the part of the surgeon.
Magnetic resonance angiography seems to have limited role in the detection of vascular compromise in trauma emergencies. CTA provides better spatial resolution and faster isotropic image acquisition, is more readily available and avoids potential hazards of prolonged imaging[59].
Then the longing29 for his home came upon him with a rush, and in the morning he told the Queen of the Immortals that he must go and see his father and mother once more
TREATMENT
Initial management
As mentioned above, patients with combined musculoskeletal and vascular injuries are approached in the first place according to ATLS principles, having in mind the “life over limb” quote. Current universal guidelines for severely multiple injured patients agree on the early administration of tranexamic acid followed by Massive Transfusion Protocol with packed red blood cells, fresh frozen plasma and platelets, as well as an antifibrinolytic agent, to treat/prevent massive hemorrhage and trauma-induced coagulopathy[60-62]. Bleeding can be controlled by direct digital or dressing compression and proximal tourniquet application, for a limited time, which is preserved for special circumstances in hospital environment, where local hemorrhage cessation cannot be achieved with other manipulations[63]. Patients with diminished peripheral pulses and associated obvious gross limb deformity, such as displaced long bone fracture or joint dislocation, should undergo immediate manipulation to restore limb axis realignment and joint reduction respectively. The neurovascular status is consequently reassessed[64]. Reassessment is also required in cases of initial shock or hypothermia, after patient’s resuscitation and rewarming, because vascular status under these circumstances can be misleading[65].
Limb salvage versus amputation
Fasciotomies performed concomitantly with limb revascularization are associated with a four-times decrease in eventual amputation. There are also trauma surgeons who routinely perform prophylactic fasciotomies in the presence of high-risk scenarios[112]. This established intraoperative choice is possibly the reason for the low incidence of compartment syndrome after peripheral vascular injury[111]. Moreover, this approach may lead to possible conversion of a closed to open fracture, wound management related complications, altered sensation and chronic limb pain[113]. Still, these potential risks are easily overcome when there is a high chance of developing compartment syndrome and early fasciotomies should be considered in cases of revascularization following vascular trauma, multiple fractures or dislocation and /or multiple arterial injuries[21,112].
The Lower Extremity Assessment Project, a prospective multicenter study of patients with severe lower extremity injuries, stated that these limb-threatening injuries are likely associated with poor functional outcomes regardless of the choice between limb salvage and amputation[67]. Analogous results were presented by MacKenzie[68], in a series of 397 patients with severe lower limb trauma.The functional results were equally poor after amputation and limb reconstruction, and the outcome scores indicated substantial disability in 50% of patients.
Predictive factors for complications and poor outcomes in patients with combined musculoskeletal and vascular injuries are evaluated by variable injury scoring systems (MESS, NISSSA, LSI, PSI and HFS) including extensive soft-tissue injury, presence of open fracture, ischemic period exceeding 6 h,neurological deficit and other associated major injuries[69,70]. MESS (Mangled Extremity Severity Score) is predictive of amputation but its clinical validity is still in debate. MESS has been devised as a treatment decision aid; a score of ≥ 7 points usually indicates the need for primary amputation[71]. In 1994, Shanmuganathan[72] proposed the NISSSA score (Nerve Injury, Ischemia, Soft tissue injury,Skeletal injury, Shock and Age of the patient), which had the additional component of nerve injury -especially the loss of plantar sensation - apart of the bone and soft tissue injury components. Both scores were highly predictive of amputation, but the NISSSA had better sensitivity (81.8%63.6%) and specificity (92.3%69.2%) compared to MESS[72]. The Predictive Salvage Index (PSI) was proposed by Bosse[67] in 1987, with a reported sensitivity and specificity of 78% and 100%, respectively. The limb salvage index (LSI) was proposed by Russell in 1991 and although not utilized widely, the score was found more predictable than the MESS, PSI, NISSSA, and HFS-97 when assessing type III tibial fractures. Primary amputation is recommended after significant distal trauma, extensive crush, severe nerve dysfunction, an ischemic limb with duration exceeding 4 h of warm ischemia, segmental bone loss over one third of the length of the tibia, muscle loss in more than two compartments, and severe open foot injuries[73]. Besides injury characteristics, factors like non-Caucasian race, older age, female sex,lower educational level, lower economic status, smoking, and poor reported pre-injury general health condition, seem to play an important role in patients with less-than-optimal results[68].
Amputation
Limb amputation is a realistic solution in an emergency and could be life-saving in the setting of sepsis or ongoing bleeding in a hemodynamically unstable trauma patient, with the advantages of shorter hospitalization, fewer secondary procedures, and faster rehabilitation period. A published case series of nonsalvageable limb injuries reported that a delay of up to 5 d can be tolerated without negative impact on stump infection risk, giving the time for patient preparation and procedure planning on a semielective basis[74]. It must be underlined that long-term costs of prosthetics could likely make amputation an ultimately more expensive procedure[75].
Amputation level, determined by the nature of injury, is another crucial point of interest related with long-term functional outcome. It is well recognized that preservation of the knee joint provides a significant functional advantage. With a stump of sufficient length, the prosthesis has better support and less energy for movement is demanded[76]. Transtibial amputees perform better than transfemoral or through-knee ones, with decreased rehabilitation time[77,78]. However, the tissue condition after traumatic injuries requiring below-knee amputation is not always adequate to provide a lengthy and durable stump able to support a prosthesis, given the fact that at least 10 cm from medial tibial plateau is recommended[76,79]. In such cases, composite flaps harvested from the amputated limb and sparepart surgery concept may provide stump lengthening, thus avoiding a more proximal amputation or the use of flap[80,81].
Limb salvage
Patient’s clinical situation, other major trauma (trunk, visceral or craniocerebral)than extremity injury requiring surgical treatment or nonoperative surveillance and determination of the type of vascular injury, are factors considered when proceeding to the operating theater. A necessary condition for fast and safe surgical management includes grouping of injured tissues,planning of the procedure and defining the appropriate equipment for successful cooperation between different specialties. Furthermore, possible required equipment and devises should be confirmed,including magnifying loupes and vascular surgery - microsurgical instrumentation, external and internal fixation systems, and shunts.
Even after a successful initial, multidisciplinary-guided treatment of a combined musculoskeletal and vascular injury, long term follow-up is crucial to prevent and detect early possible complications. This follow-up evaluation is performed by both orthopedic and vascular surgeons, with additional consultation from reconstructive surgeons, if necessary[126]. Alternatively, orthopedic surgeons with microsurgical background and competence can follow these patients, as they can solely perform allaround surgery for these combined injuries. Postoperative evaluations can be delayed in cases of segmental fractures, associated bone loss, or infection. In case of team management, the vascular surgeon will evaluate the arterial perfusion and venous flow and determine the shift from prophylactic thromboprophylaxis to antiplatelet agents 3-6 mo postoperatively. The vascular repair should be followed with ABI testing as well as graft duplex scan.
In the presence of acute life-threatening injuries, like intracranial hematoma, thoracic, abdominal or pelvic bleeding, team management with two operating teams should be considered to manage the lifethreatening injury, and control bleeding and re-establish perfusion at the injured extremity. In such cases, temporary measures, such as external fixation systems and intraluminal shunts, are the chosen treatment options following the Damage Control Surgery principles[82-84].
Vascular injuries include a variety of lesions from arterial spasm to complete transection. Pre- or intraoperative accurate diagnosis of injury type is crucial as it guides the treatment modality. Overall, vascular injuries include complete wall defects with hemorrhage or pseudoaneurysm, intimal tears like disruption, flap or subintimal hematomas, complete transections with hemorrhage/ occlusion, arteriovenous fistulas and vascular spasm[21,64].
Regarding the injury mechanism, penetrating trauma is most associated with complete transections,wall defects or secondary development of arteriovenous fistulas. Blunt trauma, however, is usually associated with intimal defects or subintimal hematomas. Arterial spasm can be a result of either blunt or penetrating injury, more commonly in young patients[65].
Little did she know that, over the years, the husband have been trying all ways to please her, little did she know that drumsticks was the husband s favorite.
Vascular injuries that are nonocclusive, like arterial spasm, intramural hematomas, or intimal flaps have a satisfactory healing potential with nonoperative treatment, with reported rates of 87%-95%[85,86]. Single vessel occlusion located peripherally - distal to knee/elbow - does not constitute risk for the viability of the limb. In these cases, in the absence of mangled extremity or severe soft tissue damage,observation with close clinical and imaging surveillance is a viable option. Other treatment options,besides open vascular repair, have a role in selected, isolated traumatic aneurysms where embolization can be performed[64]. Moreover, small pseudoaneurysms and intimal flaps or tears can be amenable to endovascular treatments, placing endovascular stents or stent grafts[87,88].
Care should be taken from the operative team to establish the best conditions required for major surgical intervention. An operative tourniquet can replace the bleeding-control apparatus used at the emergency department. Skin aseptic preparation and draping should encompass potential areas of distal and proximal vascular control, fasciotomy sites and ipsilateral limb from groin to toenails for possible greater or lesser saphenous vein retrieval[52,64]. Adequate surgical approach is essential, with proximal and distal extension of the injury zone, to control hemorrhage and determine type and extend of arterial injury.
Sequence of intervention when orthopedic and vascular surgeons are implicated, remains an area of relative debate, despite being reported that this surgical sequence probably does not affect lower limb amputations rates[89]. Fracture reduction and fixation offers a stable skeletal “scaffold” for subsequent vascular repair (Figure 3). Vascular repair decreases warm ischemia time of the affected extremity[26,90]. Ischemia is crucial and determines the sequence of surgical intervention, with 6 h generally being the cutoff time interval for higher limb salvage rates[89,91]. It must be underlined that ischemia time is never accurate and in most cases is underestimated by patient, relatives, ambulance crew or other healthcare professional. As a general rule, in cases with cold ischemia (pulseless limb with no capillary refill) and in patients with prolonged period of warm ischemia (present capillary refill), vascular intervention should be performed first so as to restore perfusion as soon as possibletemporary intraluminal vascular shunt insertion[64,92,93]. Fracture fixation can be performed first when there is no evidence of cold or prolonged warm ischemia, especially in concomitant presence of unstable,comminuted fracture pattern.
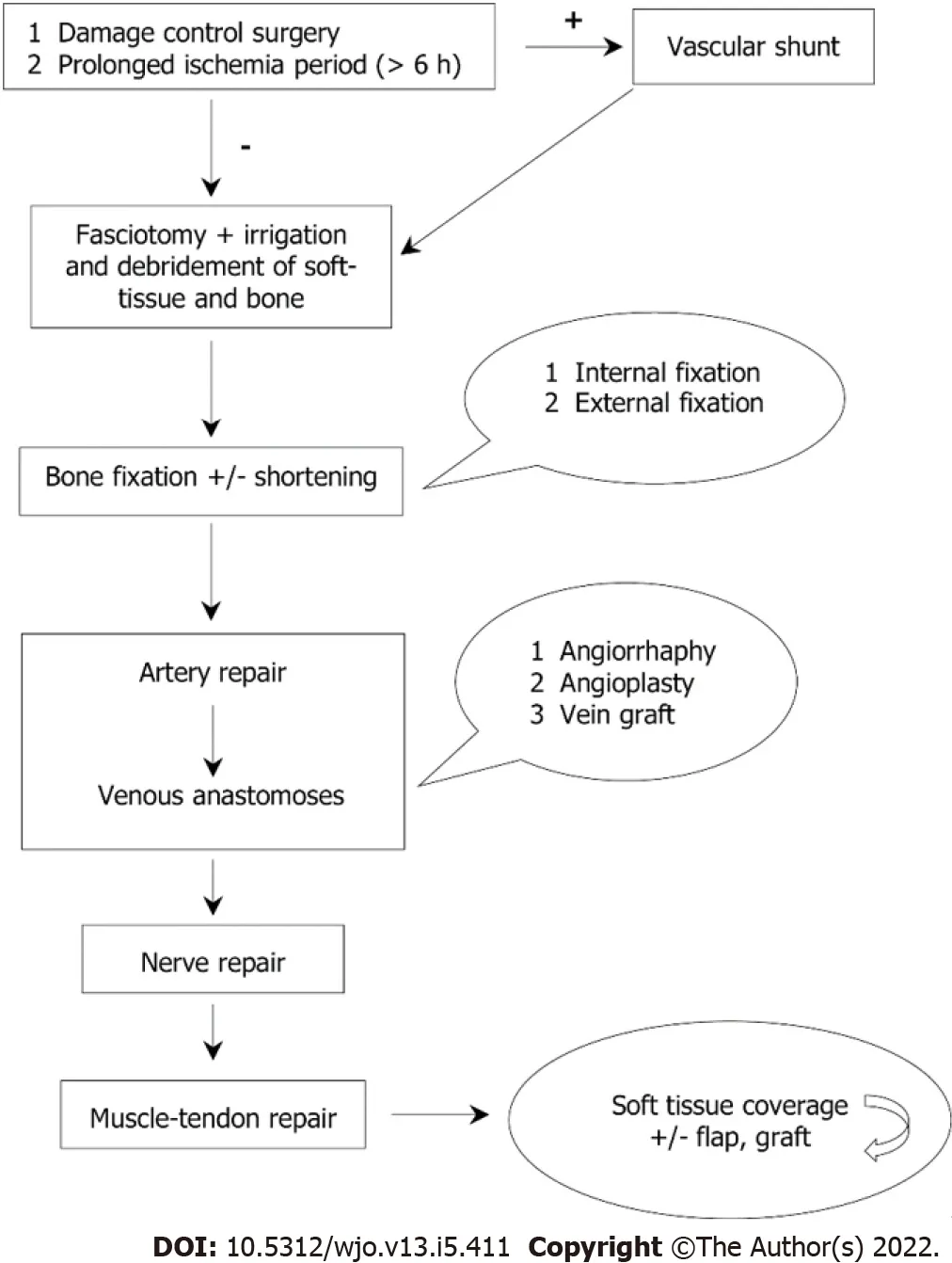
Concerning operative treatment of coexisting fracture, the dilemma between temporarydefinitive fracture fixation turns towards temporary external fixation by most authors, in order to offer prospective for bone defect management and avoid infection, “second hit” phenomenon related to coagulopathy, systematic inflammatory immune system response and fat/pulmonary embolism[94-96].Bone transport as well as induced membrane or Masquelet technique are options for large, segmental bone defects[97-99].
Regarding operative options for vascular injury manipulation, they include direct repair -anastomosis, vein patch angioplasty, bypass anastomosis with interposition graft placement,endovascular stents, and temporary intraluminal vascular shunts.
In cases of small lacerations, lateral angiorrhaphy with or without vein patch angioplasty is adequate as repair option. Injuries involving complete artery transection are addressed with central and peripheral debridement till healthy intima followed by end-to-end anastomosis[100,101]. If the anastomosis is not free of tension, a substitute conduit must be interposed. Conduit of choice for the most cases of peripheral vascular injuries is the autogenous reversed saphenous vein graft from the contralateral, uninjured lower limb with the alternatives of cephalic or basilic upper limb veins and synthetic grafts[100,102].
A keynote step in the operative treatment pathway of vascular injuries is the early recognition of patients indicated for temporary intraluminal shunt insertion, rather than definitive vascular repair and prior to bone stabilization. These indications include critically injured patients as part of damage control surgery, Gustilo IIIC open fractures, prolonged ischemia period, need for distal perfusion while another complex revascularization procedure like extra-anatomical bypass is performed and prior to replantation perfusion of an amputated upper extremity part[103,104].
Vein injuries and possible repair are usually addressed with less caution, in the presence of arterial injuries that are limb threatening. Peripheral vein ligation rarely consists a threat for limb salvage, but increases postoperative swelling and venous soft-tissue hemorrhage, having transient adverse effects on arterial inflow and leading to increased morbidity and infection risk. Operative options for peripheral venous repair include venous patch angioplasty, thoracostomy tubes as intraluminal venous shunts, or interposition graft placement from contralateral greater saphenous vein, common femoral vein, or axillary vein[105].
Injured structures are identified from superficial to deep layer, based on the knowledge of the crosssectional anatomy, and reconstruction starts from the deeper layer. Nerves are repaired after bone and vascular structures followed by muscle and tendons, which are the last to be reapproximated. Careful documentation by photos and/or video is mandatory, not only to accurately define the postoperative rehabilitation protocol, but for medicolegal purposes too. Tension-free nerve restoration is advocated, as neuroma formation is a common complication when nerve repair is performed incorrectly or under tension. Soft tissue coverage is the last stage that will ensure the rapid healing of the tissues. Decision for coverage should be taken in conjunction with reconstruction surgeon, including muscle flap transportation or extra-anatomical bypass graft fashioning[101,105,106].
Duplex ultrasound scanning (DUS) represents a combination of B-mode real-time ultrasound and pulsed Doppler flow. DUS is accurate in assessing vascular injury with reported sensitivity from 50% to 100% and specificity exceeding 95%[50,51]. It is also noninvasive and cost-effective but can be timeconsuming and significantly operator-dependent. Therefore, many surgeons consider it unreliable for the detection of vascular injuries in extremity trauma. In contrast, it may have a role in the surveillance of known vascular injuries in which nonoperative treatment has been selected[52].
The use of negative pressure wound therapy as an alternative treatment of soft tissue defects, seems to improve angiogenesis, regulate perfusion, and promote local microvascular maturation. However, its use is limited and its efficacy and superiority over conventional dressing is questionable according to current multicenter randomized control trials and to Wound management of open lower limb fractures(WOLLF) study[107-109].
In the English country of Berwickshire, they say that brownies leave when given any gift because God appointed them as the servants of mankind, bound to work without payment
Cases with combined musculoskeletal and vascular injuries almost never have a unique surgical intervention. Second look for surgical site infection, soft-tissue viability and confirmation of vascular perfusion is routinely performed 24-48 h after initial surgery. The fasciotomy incision closure is performed after 7-10 d in case of optimal postoperative findings. At the same time,definite skeletal stabilization should be performed (external to internal fixation modification or unilateral external fixation system conversion to circular frame/hybrid fixation system) to minimize the risk of surgical site infection after the definite treatment, in case of preceding pin track infection.
COMPLlCATlONS
Compartment syndrome – fasciotomies
Compartment syndrome is defined as the increased pressure within a closed fascial space, leading to reduction of capillary perfusion to less than required level for tissue viability, well recognized as cause for poor limb functional outcome[110,111]. It is the result of external compression or fascia closure and after increased compartment pressure in cases of ischemia-reperfusion, fractures, soft-tissue contusion,and venous outflow obstruction. In this concept, situations like crush injury, significant limb swelling,combined arterial and venous injuries requiring simultaneous clamping, need for arterial/venous ligation, early thrombosis of vascular repair, ongoing hypotension/continuing resuscitation and delayed treatment with no arterial perfusion for 4-6 h, determine high-risk patients for compartment syndrome development after combined trauma. Early clinical findings related to compartment syndrome are pain on passive movement of the involved compartments’ muscles and patients’ pain considered out of proportion to the injury, while classical 6 Ps (pulselessness, pallor, paresthesia, pain,paralysis, poikilothermia) are frequently not present in trauma patients with possible altered mental status and associated injuries and represent late signs of established compartment syndrome on the injured extremity[110].
A crucial question to be answered early after patient presentation and initial resuscitation, is the one of limb salvageprimary amputation, and in case of amputation, the timing and level of amputation.This decision is usually hard for patients, families and trauma surgeons. Patients in most cases are young and active with long remaining working lifespan, not willing to integrate a major, permanent physical modification. Surgical teams, however, usually experience amputation as a therapeutic failure and sometimes multiple, complex salvage procedures are guided, with uncertain outcome but with preservation of the patient’s body image, at least initially. Progress and ongoing experience in microsurgical and reconstructive techniques provides wide range of surgical options, but limb salvage choice with extended indications, has often remarkable functional and emotional cost for the patients[66].
Infection
In addition to the basic complication of the already-mentioned compartment syndrome, bone and softtissue infection following combined musculoskeletal and vascular injuries, represents the major cause for late extremity amputation[114-117]. Gustilo[118], classifying open fractures reported an infection rate as high as 42% associated with vascular damage requiring repair (Gustilo IIIC fractures).Moreover, infection seems also being related with vascular thrombosis[119].
Nonunion
Vascular compromise, which often indicates the release of high energy in the fracture area, is a wellestablished predictive indicator for a nonunion in Gustilo-Anderson grade IIIC injuries[120]. Moreover,the coexistence of even a subclinical compartment syndrome appears to delay or prevent the process of long bones union[121].
Secondary amputation
Secondary amputations can be expected in 5.5%-28% of Gustilo type IIIC open tibial fractures[122,123].The main reasons for secondary amputation include delayed revascularization, lack of adequate collateral blood flow, extensive soft tissue necrosis, infection, distal thrombosis, or postoperative arterial disruption[124].
Venous insufficiency
There is increasing evidence that primary or secondary venous insufficiency, particularly in the setting of combined peripheral arterial and venous injuries, may impair the chance of limb salvage. A proposed benefit to venous patency is that maintaining adequate venous drainage of an injured extremity can minimize extremity swelling, hemorrhage, and compartment syndrome. Feliciano argued that these acute benefits are an indication for immediate venous reconstruction, even if the fate of the repair will likely be to thrombose later[102]. Other local vascular complications such as arterial disruption,pseudoaneurysm and emboli may result in a vicious circle of both regional and systemic adverse effects,like myocardial infarction, respiratory distress due to pulmonary embolism, acute renal failure,[125].
When the kids came in, he took them for walks along the pier21 near their office. Often she went along and watched Eric, who was becoming a master of sign language, talk and laugh with her boys as no one else had before.
LONG TERM FOLLOW-UP
For some months the king’s grief was great; then gradually he began to forget a little, and, besides, his counsellors were always urging him to seek another wife. At first he refused to listen to them, but by-and-by he allowed himself to be persuaded to think of it, only stipulating7 that the bride should be more beautiful and attractive than the late queen, according to the promise he had made her.
15. White pebbles: Pebbles symbolize46 justice. In ancient Greece, a vote with a white pebble4 indicated that the voter thought the suspect was not guilty. White pebbles have also been used as gravesite gifts to ensure rebirth of the spirit (Olderr 1986).
In addition, the continuous cooperation with the radiologists, physiatrists and physiotherapists at the follow-up period ensures rapid recovery without serious complications, or their detection and management in a timely manner. Finally, due to the functional impairment frequently left after these complex injuries, long-term psychological support is often necessary.
DlSCUSSlON
CTA is established as the gold standard imaging method when dealing with vascular injuries in the extremity trauma[53-55]. CTA provides a rapid confirmation of the presence and location of vascular injury with simultaneous detection of bone and soft-tissue injuries/defects, without being an interventional examination and with high cost-effectiveness index[56]. It can highlight radiological findings like hematoma, active bleeding (contrast medium extravasation), arterial dissection, transection or occlusion,pseudoaneurysm, arteriovenous fistulas, focal narrowing or spasm, as well as anatomical variants of vascular origin like bifurcation with an hypoplastic posterior tibial artery or popliteal artery trifurcation in the popliteal fossa[53]. The study has limitations in cases with CT artifacts in the presence of foreign body such as metallic fragments at the study field, suboptimal accuracy in poor timing of intravenous contrast agent administration and the potential risk for renal damage from contrast medium[57]. As mentioned above, presence of obvious hard signs dictates operative treatment on an emergency basis without further imaging. However, trauma teams can consider the execution of CTA in the case of hemodynamically stable patients despite hard signs for vascular injury, for preoperative planning so as to avoid extended exploration intraoperatively and to decrease surgical time[58].
The level of alertness is always determined by (1) The pattern of the injury (open or closed, fracture or dislocation, single or multiple injury, calibration of injury scores); (2) The anatomical area of the injury(open tibial fractures, knee dislocations and supracondylar elbow fractures in children of type III due to Gartland classification have rates of concomitant vascular injuries > 10%)[21,24,26,28,29]; and (3) The type of arterial lesion that the literature correlates with specific trauma patterns. Vascular injuries that are nonocclusive, like arterial spasm, intramural hematomas, or intimal flaps have a satisfactory healing potential with nonoperative treatment, with reported rates of 87%-95%. Therapeutic choices usually consist in monitoring the patient during follow-up, by means of physical examination and ultrasound scan. Single vessel occlusion located peripherally - distal to knee/elbow - does not constitute a risk to the viability of the limb. In these cases, in the absence of mangled extremity or severe soft tissue damage, observation with close clinical and imaging surveillance is a viable option[85,86].
A fundamental dimension of the successful outcome of combined orthopedic and vascular injuries is the speed and accuracy of patient management. Most of the time lost in the treatment approach of the injured patient, after the arrival to the trauma center, concerns the definite diagnosis of the vascular injury and the decision-making procedure. Orthopedic pathology is defined in the majority of cases with a simple X-ray (usually already done in primary or secondary survey). The presence of hard signs has 92%-95% sensitivity for incidence of vascular injuries requiring surgical intervention with a positive predictive value of 95%[33-35]. In these cases, immediate operative intervention - injury site exploration in the presence of any hard sign - is strongly suggested by the literature without further delay for additional advanced vascular imaging (CT or conventional angiography)[36,37]. Rapid decisions are ensured by the use of trauma classifications which assist the surgeons’ judgment in adjunct to clinical evaluation and facilitate in-depth guidance of patients and their families prior to definitive surgical treatment. Predictive factors for complications and poor outcomes in patients with combined musculoskeletal and vascular injuries are evaluated by variable injury scoring systems (MESS, NISSSA, LSI, PSI and HFS)[69,70].
It is also necessary in the future to establish common action protocols between orthopedic, vascular and general surgeons, and for each tertiary trauma center to have a clearly defined action protocol that will be applied in the same way each time and will be included in the training program of young doctors.
As a general rule, in cases with cold ischemia (pulseless limb with no capillary refill) and in patients with prolonged period of warm ischemia (present capillary refill), vascular intervention should be performed first so as to restore perfusion as soon as possibletemporary intraluminal vascular shunt insertion. Fracture fixation can be performed first when there is no evidence of cold or prolonged warm ischemia, especially in concomitant presence of unstable, comminuted fracture pattern. Failure to perform fasciotomies after revascu larization of an acutely ischemic limb is the most common cause of preventable limb loss. Finally, a bed in the intensive care unit ideally should be reserved for early postoperative monitoring. Although open surgical repair has always been the gold standard for treating vascular trauma, the application of endovascular techniques should be a more beneficial future perspective according to specific indications.
CONCLUSlON
Although vascular injuries are rare, they may occur in the context of major combined musculoskeletal trauma. The high index of suspicion, the imaging evaluation, and the timely referral of these patients to organized trauma centers ensure firstly the survival of the patient and the extremity and secondarily the best functional outcome in such challenging cases. Vascular injuries as part of musculoskeletal trauma are usually the result of the release of a high-energy load at the wound site so that the prognosis is strongly determined by the degree of soft-tissue damage, the duration of limb ischemia, the patients’general medical status and the presence of associated injuries. We therefore consider that distinct guidelines and multidisciplinary team management arepreconditions in dealing with combined musculoskeletal and vascular injuries of the extremities.
FOOTNOTES
Stefanou N, Papageorgiou F and Dailiana ZH wrote the paper; Stefanou N, Arnaoutoglou C and Dailiana ZH participated in the conception and design of the study; Stefanou N, Arnaoutoglou C, Papageorgiou F and Dailiana ZH participated in the analysis and drafting of the literature data; Matsagkas M, Varitimidis S and Dailiana ZH participated in critical revision of the article; Varitimidis S, Dailiana ZH participated in the analysis and interpretation of the literature data; All authors read and approved the final manuscript.
They were very poor, and their seven children4 incommoded them greatly, because not one of them was able to earn his bread. That which gave them yet more uneasiness was that the youngest was of a very puny2 constitution, and scarce ever spoke3 a word, which made them take that for stupidity which was a sign of good sense. He was very little, and when born no bigger than one s thumb, which made him be called Little Thumb.1
Authors declare no conflict of interests for this article.
This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Greece
We should take this to heart, so that it may not happen to us, for we cannot indeed tell if we may not some day come to the rag-bag, and be made into white paper, on which will be printed our whole history, even the most secret parts, so that we too go about the world relating it, like the shirt-collar
Nikolaos Stefanou 0000-0002-6784-6022; Christina Arnaoutoglou 0000-0002-2280-8866; Fotios Papageorgiou 0000-0001-6646-9379; Miltiadis Matsagkas 0000-0001-8164-6601; Sokratis Varitimidis 0000-0003-3193-9566; Zoe H Dailiana 0000-0003-3890-0832.
Liu JH
Kerr C
Liu JH
 World Journal of Orthopedics2022年5期
World Journal of Orthopedics2022年5期
- World Journal of Orthopedics的其它文章
- Coronal plane deformity around the knee in the skeletally immature population: A review of principles of evaluation and treatment
- lnsufficient lateral stem contact is an influencing factor for significant subsidence in cementless short stem total hip arthroplasty
- Distal femur complex fractures in elderly patients treated with megaprosthesis: Results in a case series of 11 patients
- Prevalence and factors of work-related musculoskeletal disorders among hand surgeons
- What factors are important to new patients when selecting an orthopedic oncologist?
- Anterior vertebral body tethering for idiopathic scoliosis in growing children: A systematic review
