A good death from the perspective of healthcare providers from the internal medicine department in Shanghai: A qualitative study
Chunyan Chen , Xiaobin Lai , Wenjuan Zhao , Menglei Chen
a Department of Nursing, Shanghai Cancer Center of Fudan University, Shanghai, China
b Department of Oncology, Shanghai Cancer Center of Fudan University, Shanghai, China
c School of Nursing, Fudan University, Shanghai, China
d Department of Integrated Therapy, Shanghai Cancer Center of Fudan University, Shanghai, China
Keywords:Attitude to death Hospice care Internal medicine Medical staff Qualitative research
ABSTRACT Objective: This study aimed to explore the understanding of healthcare providers working in the internal medicine department in Shanghai regarding a good death.Methods: The data of the study was collected using face-to-face semi-structured interviews.Through purposive sampling,16 physicians and 13 nurses who had experiences of caring for adult patients with life-threatening illnesses at the end-of-life stage in Shanghai were interviewed.The interviews were analyzed using qualitative content analysis.Results: Six characteristics of a good death emerged:no suffering,companionship and care,no worries or concerns, dying with dignity, involvement and acceptance, and less impact on the family.Eighteen categories were identified: dying without experiencing suffering; being relieved of symptoms and suffering; being relieved of psychological suffering; avoiding the use of futile treatment and resuscitation; being cared for and accompanied by family; receiving good health care; having a meaningful life without regrets; making good arrangements for family issues;having a chance to say goodbye;having a quality life before death; dying in a decent environment;the personal will to be respected; maintaining the integrity of the body;death of the patient being accepted by the family and healthcare providers;the death occurred despite the best efforts to care for the patient;limited financial and care burden;shortly affected quality of life of the patient; and improved family cohesion.Conclusion: Family members’ early involvement in caring for patients at the end-of-life stage helps achieve a good death.For patients with a terminal illness, avoiding unnecessary medical treatment and resuscitation could be the first step in achieving better patient death and promoting the development of advanced care planning in the mainland of China.
What is known?
· The meaning of a good death varies depending on different socio-cultural backgrounds from the perspective of different specialties.
· The attributes of a good death in Chinese society may include physical pain-free comfort and bodily integrity, psychological and spiritual peace, the wellbeing of family members, and the families’ companionship with the patients.
· The provision of health care is an essential criterion of a good death.
What is new?
· Both family members and healthcare providers should be considered when evaluating the quality of death of the patient with a Chinese cultural background.
· Family members’early involvement in caring for patients at the end-of-life stage helps achieve a good death.
1.Introduction
A good death is a multidimensional concept that is affected by multiple factors.Its meaning varies depending on sociocultural backgrounds.Compared with research on a good death in Western societies, a good death has been under investigation in the mainland of China.Zhang et al.interviewed Chinese patients with advanced cancer regarding their good death experience [1].Liu et al.explored the expectations of a good death in Chinese patients with advanced cancer using a qualitative approach[2].In addition,the death expectations of Chinese patients were assessed using foreign questionnaires [3,4].Several review articles on this topic have been published in the mainland of China during the past few years[5-8];however,most studies included in the review articles were conducted in overseas countries.Defining a good death in the mainland of China requires further exploration.
As dying increasingly becomes medicalized, a good death should be defined by the dying person, the family, and the healthcare providers[9].Healthcare providers,primarily those who provide care for chronically ill patients, have several years of experience caring for these patients and their families in their final days.Their experiences enrich their perceptions of a good death.To date,patients with terminal chronic illnesses do not die exclusively in hospice care settings.With the deterioration of the disease,they are frequently admitted to hospitals at the end-of-life stage[10-13].As a result, many patients die in acute-care hospitals[13-16].A recent study reported that only 9.4% of the deceased patients died in hospice care institutions in England[17].Although the United States is the global leader in hospice care,approximately 50% of the deceased did not receive hospice care [18].Others may die in acute-care wards, emergency rooms, ICUs, nursing homes,and other places where no hospice service was delivered[19,20].
In the mainland of China, more patients die in acute-care settings than in hospice care settings.Taking Shanghai as an example,there were a total of 124,500 deaths in 2018,and it was estimated that at least 69,100 patients needed hospice care in 2018.However,only 9,700 patients used this service [21].The location of death were wards of hospitals and emergency rooms (55.53%), homes(31.58%), nursing homes (7.44%), and other places (5.45%) [21].Another study reported that the most common location of death were tertiary and secondary hospitals(60.13%)in the Putuo District,Shanghai [22].Only 4.64% of the deceased died in community health service centers where hospice care was provided[22].Other studies also reported that hospital wards, emergency rooms, and ICUs were the most common location of death [23-25].To date,acute-care settings are the most common death locations of the urban areas in the mainland of China.
Chinese healthcare providers working in acute-care settings have observed how patients and their families cope with dying,thus reflecting the value of life and death and the attitude toward death in Chinese society.Therefore,their experiences could enrich the concept of a good death in the mainland of China.Hence, the research question proposed in the study was the characteristics of a good death from the perspective of healthcare providers who have experience caring for patients with life-threatening illnesses,aiming to provide theoretical evidence for future research on local hospice care.
2.Method
This was a qualitative study.Data were obtained from interviews and analyzed using qualitative content analysis.
2.1.Setting and participants
The inclusion criteria for the participants were as follows:i)had worked in the internal medicine department as a nurse or a physician for over one year; ii) had experience of caring for dying patients with life-threatening illness; and iii) would voluntarily join the study.Participants were recruited using purposive sampling.The acquaintances of the authors in the hospitals introduced potentially eligible healthcare providers to the team.The first author invited participants.Of the 30 healthcare providers approached, one refused to join without reason; thus, 29 participants(16 physicians and 13 nurses)from eight acute-care hospitals in Shanghai participated in this study.The demographic characteristics of the 29 participants are presented in Table 1.

Table 1Demographic characteristics of the participants.
2.2.Data collection
Data were collected through semi-structured interviews from October 2020 to January 2021.Each participant was interviewed once.The second author conducted the interviews.All the interviews were recorded, and field notes were made.The interviewer was a middle-aged female academic staff with a doctorate and seven years of experience conducting qualitative research interviews.An interview guide was developed.The following questions were asked in the interviews:i)What kind of death could be called a “good death”? ii) Is there any difference between the real death you have seen and the ideal death? What is the difference?iii) What would you do, as much as possible, to help patients to achieve a good death when you take care of dying patients? Each participant was interviewed in a quiet room at the hospital where they worked.During each interview, the interviewer first introduced the background and aim of the study and ensured the principles of confidentiality and voluntary participation were clear to the participant.Participants then signed consent forms and filled in a questionnaire on demographic information.The length of the interviews ranged from 8 to 53 min.Data collection was stopped when data saturation was achieved.
2.3.Ethical considerations
The ethics application was sent to the ethics committees of the hospitals involved.The ethics committees considered the study can be exempted from the ethics approval because patients were not involved in the study.All participants signed consent forms before the interviews.The objectives and the analysis methods were explained to the participants twice before the interviews were conducted.First, the first author contacted all eligible participants and introduced the study over the telephone.Healthcare providers were given several days to make decisions.They could ask questions about the studyduring the decision period.On the day of the interview,the interviewer explained the study again.The principles of voluntary participation and confidentiality were emphasized.
2.4.Data analysis
All records were transcribed verbatim.NVivo software version 11 was used to manage and analyze transcripts.Qualitative content analysis was adopted for the data analysis [26].The study was conducted according to the following steps: i) reading the transcripts thoroughly; ii) dividing the interviews into content areas according to the interview questions;iii)extracting and condensing meaning units;iv)abstracting and labeling with a code;v)sortingthe codes into sub-categories/categories; and vi) creating subthemes/themes [26].The data were coded by the first two authors and reviewed by the other two authors.All authors discussed the results.One researcher (X.Lai) was an academic staff member specializing in nursing.Two(C.Chen&W Zhao)were experienced nurses working in oncological settings; one (M.Chen) was a physician specializing in palliative medicine.One (X.Lai) has a doctoral degree, and two (W.Zhao& M.Chen.) have masters’ degrees.The other has a bachelor’s degree.All four authors were female.
2.5.Rigor
Several methods were used to enhance the rigor of the study.The research team invited physicians and nurses from different hospitals located in several city districts to strengthen the study’s credibility.Physicians and nurses were interviewed to obtain opinions from two distinct perspectives.To foster the reflexivity of the study, the research team involved researchers with academic and clinical backgrounds.The study was designed after several discussions within the group.To manage the researcher bias generated by relying on a single interviewer,all the team members reviewed the data,discussed the findings,and reached a consensus on the results.One researcher (X.Lai) recorded her thoughts in a personal journal during the research process while conducting the interviews and after the interviews [27].
3.Results
According to the interviews,the characteristics of a good death included no suffering, companionship and care, no worries or concerns,dying with dignity,involvement and acceptance,and less impact on family (Table 2).
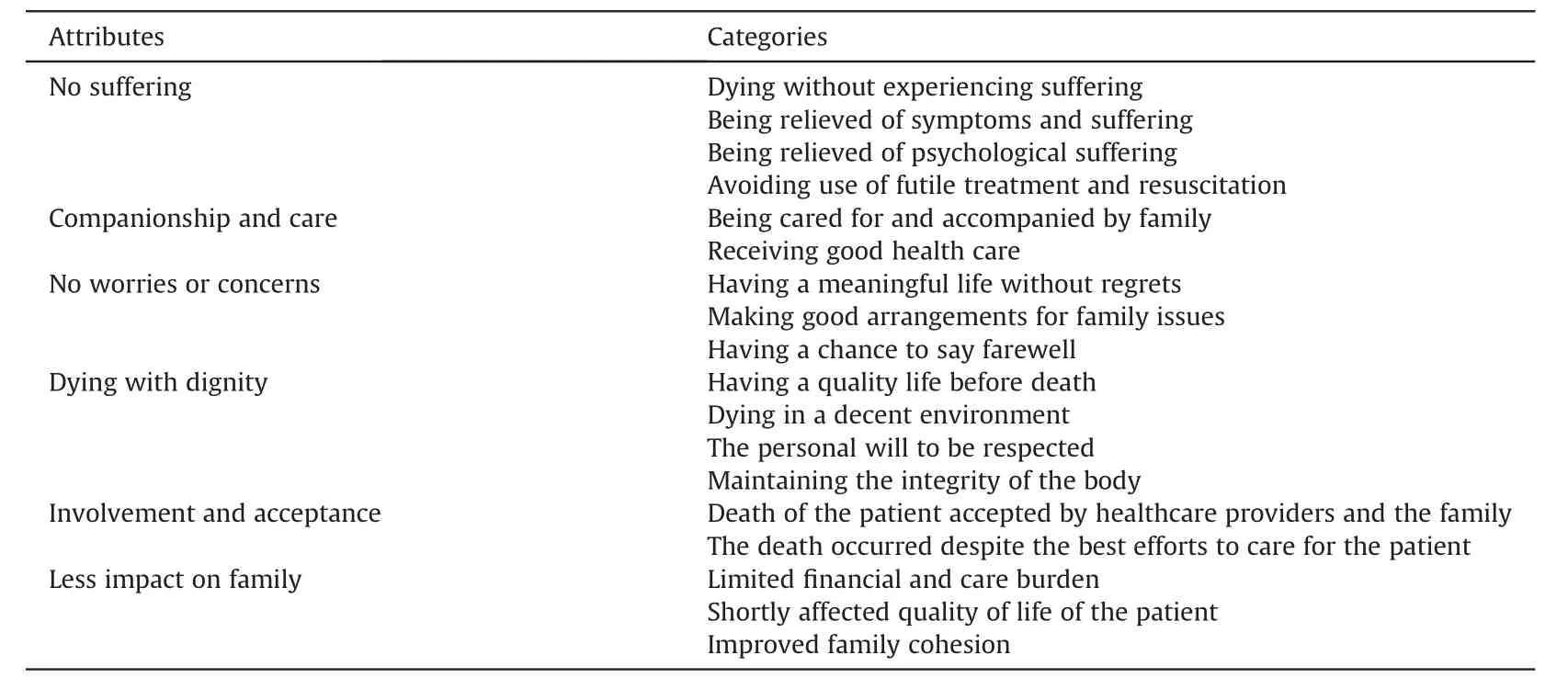
Table 2Attributes of a good death.
3.1.No suffering
No suffering was the principal characteristic of a good death for the participants.Most people die from illness;relieving symptoms and suffering is a critical component of a good death.
“It would be best that one could die in sleep.If the disease is inevitable, helping the patient have no suffering and alleviating their symptoms is an important component of a good death.”(D4)“I think no pain is essential for patients.” (N1)
Furthermore,the participants thought dying patients needed to avoid futile medical treatment and resuscitation in the end.
“For patients with late-stage cancer or heart failure, it is meaningless to use what is called ‘active rescue,’ that is, intubation,cardiopulmonary resuscitation (CPR), respiratory machines, etc.They only cause pain to patients.” (D3)
In addition, relieving the psychological suffering of dying patients was also an essential part of no suffering.
3.2.Companionship and care
The participants thought that being cared for and accompanied by the family was another essential characteristic of a good death.There were several things that the relatives could do for the dying patients,such as spending time with the patient,being involved in the patient’s daily care,chatting with the patient,and fulfilling the patient’s wishes.
“I think it would be best to have family members around.Dying alone is miserable.”(D4)
“I would take good care of him/her,at least I will help him/her keep clean and comfortable.” (N6)
“Money, or other materials, are useless.Comforting the feelings of patients and spending time with patients are the most important.”(N9)
Yet,the participants disagreed about sharing“bad news”with the patients and involving them in decision-making.Some thought that patients should be involved,whereas others argued that it was better to hide it.Besides,high-quality healthcare provided by professionals during the dying phase is an essential componentof“being cared for.”
“To achieve a good death, the first thing is that an individual can receive good medical and nursing care when dying.” (D12)
3.3.No worries or concerns
No worries or concerns were identified as an additional characteristic of a good death.Having a meaningful life without regrets is a characteristic of no worries or concerns.However, the definition of meaningfulness varies.It is presumed that a valuable life is one where an individual can bring happiness to the family.
“I think it is a good death after having a meaningful life and fulfilling personal value.” (D6)
Patients could die without worries when they make a good arrangement of family issues before they die.
“It is better if an individual can communicate well with the family and make a good arrangement of family issues before dying.”(D2)
Having a chance to say goodbye is also essential for a good death.
“I met some patients who had their religion.When their friends who shared the same religion come here,they recited the lection.I think it is a good way to face death since the patient could get comfort and support from the faith.” (D10)
3.4.Dying with dignity
Dying with dignity is another essential characteristic of a good death.The participants defined dignity considering four aspects.The first aspect is having a quality life before death.An individual could at least perform self-care and share feelings and ideas with others.The second aspect is dying in a familiar and decent environment surrounded by family members.
“The environment also means a lot.I could not accept dying in the emergency room.I need a room with at least a curtain between beds to provide privacy.I do not want many inessential people or irrelevant people surrounding me.” (D7)
Third, the personal will should be respected, especially in the medical decision of the patient.
“The dignity also includes that the personal will is respected.We have very often seen that family members made decisions that violated the patient’s will.The patient may experience suffering,and we felt regret.I think it would be better to follow the patient’s decision.” (N9)
Fourth, the integrity of the body is maintained during death.This means avoiding body damage due to treatments as much as possible and avoiding exposure of the naked body.
“Sometimes,when the patient was dying,family members insisted on performing resuscitation.The patient’s ribs were broken because of the CPR.I think it was an insult to the patient and no dignity at all.” (D9)
3.5.Involvement and acceptance
The participants thought that a good death was not only judged by the patient but more often by others, including the family members and the healthcare providers who had cared for the patient.Hence, it is also a characteristic of a good death that healthcare providers and family members accept the patient’s death.It could be considered a good death only when the death occurred after the healthcare providers and family members got the prognosis of the illness and tried their best to take care of the patient.
“I think it can be called a good death when healthcare providers feel they have given the patient the best care they could provide, and the family members have tried their best.” (D9)
“I think that the patient would pass away peacefully if the patient,relatives, and healthcare providers all could accept the condition.”(N4)
3.6.Less impact on family
The participants thought it was also a good death when the financial and care burden of the family was limited to as little as possible during the dying stage of the patient.
“If I were the patient, I hope that the dying phase would not last long.If I need care for years,it would be a huge burden.It would be better if I could die quickly.” (D1)
Furthermore, it was also crucial for a good death that the patient’s quality of life was affected for a short time.
“I hope the disease journey would not be long,so my quality of life would be affected only in a short period, I would only suffer for a while.This may be a better way to die.”(N6)
In addition,the participants considered it a good death if family cohesion could be improved through the painful experience.
4.Discussion
4.1.Essential components of a good death in China:family members
The study found that support and care from family members is a critical component of a good death of an individual.This finding agrees with those of previous studies [2,8,28-36].Relatives’acceptance of the patient’s death is also a critical component of a good death.Previous studies have reported similar findings, that the peace and safety of family members are essential characteristics of a good death from people in Taiwan, China [28-33].In the mainland of China, Liu et al.found that family harmony was an essential characteristic of a good death[2].These findings indicate that death is a family issue in Chinese society.Whether the family could accept the death, remain psychologically peaceful, and have no regret is critical when the individual dies.Therefore,healthcare providers should consider the acceptance and feelings of family members when caring for dying patients.
4.2.Non-ignorable characteristic: the acceptance and endeavor of family
In this study, one of the identified characteristics of a good death is that the family members involved in caring for the patients could accept their death and feel they have tried their best during the dying phase.Family involvement during the dying and death processes has been emphasized in previous literature[37-39].Long-term involvement of family members in care could allow them better to understand the actual condition and ideas of the patients.It could prevent the negative impacts of “Daughter from California Syndrome.” It allows family members to approach the prognosis more rationally and accept the patient’s death more peacefully.
Furthermore,caring for sick family members is a way for family members to share their feelings.It is also a chance to treat the ill parent with filial piety in Chinese culture.Family caregivers could reduce the regret and guilt about the patient’s death and accept the death better after spending considerable time,energy,and feelings when caring for dying patients.This finding indicates that family members should be encouraged to participate in caring activities to enhance the quality of the patient’s death.Healthcare providers can help guide family members to provide high-quality involvement.
4.3.Top difficulty hindering good death: unnecessary invasive treatment
Healthcare providers argue that the patients’ will should be followed, and their medical decisions should be respected in the study.Health care providers consider that appropriate medical treatment, rather than exhausting every possible treatment to prolong life,is a crucial aspect of a good death[40].Miyashita et al.[41]included “receiving enough treatment” as a Good Death Inventory core domain in Japanese culture.The finding of the present study is different from study of Miyashita.The perspectives of the healthcare providers and the bereaved family members might be different.Another reason may be the change of people’s attitude towards the treatment at the end-of-life stage over time.With the development of hospice care,more people realize the harm of overtreatment on patients, families, and the healthcare system at the terminal stage.Nevertheless,it is worthy of exploring the opinions of patients and family members about good death in China.
Despite the attitude change, unnecessary treatment still represents the most significant differences between death in reality and the ideal good death.Advance care planning (ACP) is a good solution for narrowing this gap.ACP has been developed for half a century since Luis Kutner proposed “Living will” in 1969 [42].Modern ACP focuses on patients’ preferences for life-sustaining treatment, organ donation, renal dialysis, pain management, artificial nutrients and hydration, cardiopulmonary resuscitation, and ventilator use.Patients’preferences are often put into an advanced directive (AD), a legal document that goes into effect only if an individual is incapacitated and unable to speak for themselves[43].
Despite heated discussions about ACP in the literature, the engagement of ACP is not satisfactory.There is a gap between the literature and policy documents relating to ACP and the realities of clinical care.Grant et al.reported that only 10%-41% of the public had named a proxy or completed a written document [44].The barriers to implementing ACP come from both healthcare providers and patients.A recent systematic review reported that a lack of communication skills, different interpretations of the concept of ACP,cultural factors,being lost in transition,and medicolegal issues were barriers hindering the implementation of ACP in clinical settings [45].The attitude of family members toward ACP also affects their engagement in ACP.Some families may think that ACP means giving up and losing hope [46].
A recent review found that implementing ACP in clinical settings in Asia is challenging [47].Although physicians in Asia acknowledge the importance of ACP, they rarely engage in it because of several considerations [47].Taiwan, China was the first in Asia to legalize the process of ACP in 2016.However,only 0.086%of the adult population completed the ADs in 2020 in Taiwan,China[48].The focus on ACP has increased in the mainland of China’s academic community during the past few years.The perception and acceptance of ACP in public in the mainland of China are relatively low [49].In addition, the avoidance attitude of Chinese people toward death would be a significant barrier to ACP[46,50].Owing to multiple factors, such as cultural factors, public awareness,policy and regulations,and religious factors,it is currently not the best time to promote ACP in the entire society in the mainland of China [51].Despite the long time required to implement ACP in the mainland of China, avoiding unnecessary medical treatment and resuscitation for patients with a terminal illness can be the first step toward promoting its development and enhancing the quality of dying and death of a patient.It could be a key research topic to promote good death in the current Chinese medical and social environment.
4.4.Study limitation
The study only recruited healthcare providers working in Shanghai in the acute-care hospitals (i.e., tertiary hospitals).In Shanghai, patients with terminal illness may also spend their last days in sub-acute care hospitals (i.e., secondary hospitals).A few patients die in the hospice wards of community health service centers.Hence, healthcare providers working in sub-acute care hospitals and hospice care settings should also be studied to understand the concept comprehensively.Additionally,the concept of a good death is worthy of exploration in other areas in the mainland of China.This would develop a more generalizable concept of what it means to have a good death in the mainland of China.
5.Conclusion
This qualitative study explored the perceptions of a good death of healthcare providers with a Chinese sociocultural background.Six characteristics of a good death were identified: i) no suffering;ii) companionship and care; iii) no worries or concerns; iv) dying with dignity;v)involvement and acceptance;and vi)less impact on the family.One prominent characteristic of a good death in Chinese society is the feeling of healthcare providers and family members trying their best and their acceptance of the patient’s death.Furthermore, reducing the use of invasive treatment during the end-of-life stage is a significant factor for enhancing the quality of death in China.
Declaration of competing interest
The authors have declared no conflict of interest.
Funding
This work was funded by the 2020 Original Research Project of Fudan University, China.
Data availability statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
CRediT authorship contribution statement
Chunyan Chen:Conceptualization, Methodology, Resources,Writing - original draft.Xiaobin Lai:Conceptualization, Methodology, Software, Formal analysis, Investigation, Writing - original draft, Supervision.Wenjuan Zhao:Methodology, Formal analysis,Resources, Writing - review & editing.Menglei Chen:Methodology, Investigation, Resources, Writing - review &editing.
Acknowledgements
The authors would like to thank all of the colleagues and friends who helped to approach eligible health care providers.We would also like to thank Editage (www.editage.cn) for English language editing.
Appendix A.Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijnss.2021.11.002.
 International Journal of Nursing Sciences2022年2期
International Journal of Nursing Sciences2022年2期
- International Journal of Nursing Sciences的其它文章
- Effects of mindfulness meditation on trait mindfulness, perceived stress,emotion regulation,and quality of life in hemodialysis patients:A randomized controlled trial
- Application of rational emotive behavior therapy in patients with colorectal cancer undergoing adjuvant chemotherapy
- The effect of slow deep breathing relaxation exercise on pain levels during and post chest tube removal after coronary artery bypass graft surgery
- The association between frailty of older stroke patients during hospitalization and one-year all-cause mortality:A multicenter survey in China
- Translation and piloting of the Chinese Mandarin version of an intensive care-specific pressure injury risk assessment tool (the COMHON Index)
- Adaptation and validation of pediatric peripheral intravenous catheter insertion and care practices audit tools
