Applying the Passot technique in the surgical treatment of severe gynecomastia:A case report and literature review
Arnab Mohanty
Department of General,Minimal Access and Gastrointestinal Surgery,St.Stephen’s Hospital,Delhi 110054,India
Keywords:Reduction mammoplasty Gynecomastia Inferior pedicle Nipple transposition
ABSTRACT Gynecomastia is emerging as a major cosmetic and physiological concern among adolescents,especially in relation to obesity,acute weight loss following surgery,and other endocrine illnesses.Surgical treatment involves liposuction (mechanical,power-assisted,or ultrasound-assisted),nipple-conserving subcutaneous mastectomies,or nipple transpositions via various techniques.Unsightly scarring,with visible scar hypertrophy and nipple necrosis,continues to plague postoperative cosmetic outcomes;hence,different techniques of performing nipple transposition have been devised,ranging from free grafts to pedicled flaps.In this case report,we draw attention to an old technique,described by Passot in 1925,that was applied primarily for reduction mammoplasty in women at that time.This technique is still not as frequently used as the Wise pattern mastopexy technique in gynecomastia surgery,and we wish to convey that better cosmesis would be achieved in patients with Simon IIB/III and ptotic gynecomastia using this technique,avoiding a vertical scar.
1.Introduction
Gynecomastia is the physiological or pathological enlargement of the male breast tissue.It is divided into true and pseudo disease based on glandular and fibro-fatty tissue predominance,respectively.Several classification systems have been devised,the most popular of which have been the erstwhile and subjective Simon1and the more recent,and somewhat objective,Rohrich classifications2(Tables 1 and 2).
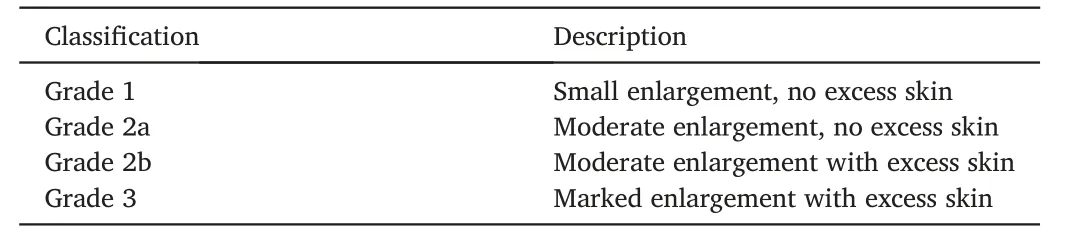
Table 1 Simon classification of gynecomastia.

Table 2 Rohrich classification of gynecomastia.
Treatment includes observation,medical therapy of the underlying endocrine etiologies,and surgery.There are also many surgical options,ranging from liposuction to more dramatic excisions and mastectomies.Patients with minimal glandular hypertrophy typically have little excess skin and are readily treated with liposuction,usually as the definitive modality.Power-assisted liposuction (PAL) and ultrasound-assisted liposuction (UAL) technologies have increased the tissue removal capability of conventional liposuction alone.3Excisional procedures include the classical Webster procedure4and the larger excisions in the Wise pattern,Letterman,and Dufourmentel-Mouly procedure,to name a few.However,many of these have been described for reduction mastopexy in women and thus present several limitations in male patients.They often leave excess glandular tissue behind,and the Wise pattern frequently causes coning of the breast and unacceptable scarring.5The stigmatization associated with inverted“T”scars has also been an issue.6Passot7described a technique of nipple transposition through a cephalad buttonhole on the breast mound,with good functional and cosmetic outcomes.This technique should probably be utilized much more than it currently is,especially in cases of severe gynecomastia.
We present a case of a boy with Simon 3,Rohrich IIB,and pseudoptosis who underwent subcutaneous mastectomy using the Passot technique and had no immediate postoperative complications and a good cosmetic outcome at the subsequent follow-up visits.
2.Case presentation
A 17-year-old boy presented to our outpatient department with enlargement of both breasts and occasional mastalgia for five years,with gradually increased in size and remained stable for one year.He had been evaluated thoroughly,and endocrine and other underlying disorders had been ruled out.On examination,he was diagnosed with bilateral Simon III gynecomastia with pseudoptosis.
He was evaluated thoroughly,including a preoperative work-up for general anesthesia.Measurements and markings were done(Fig.1),and he was planned for a subcutaneous mastectomy with an inferior-pedicled,de-epithelialized nipple flap transposition.Bilateral inframammary groove-based elliptical incisions were used for nipple-areola-skin-sparing mastectomies.The new nipple sites were marked intraoperatively (as opposed to the usual preoperative site markings)after the mastectomies were performed bilaterally,to obtain better symmetry(Fig.2).

Fig.1.Preoperative images depicting the diagnosis and operative site markings.The inframammary groove depicts the pseudoptosis.
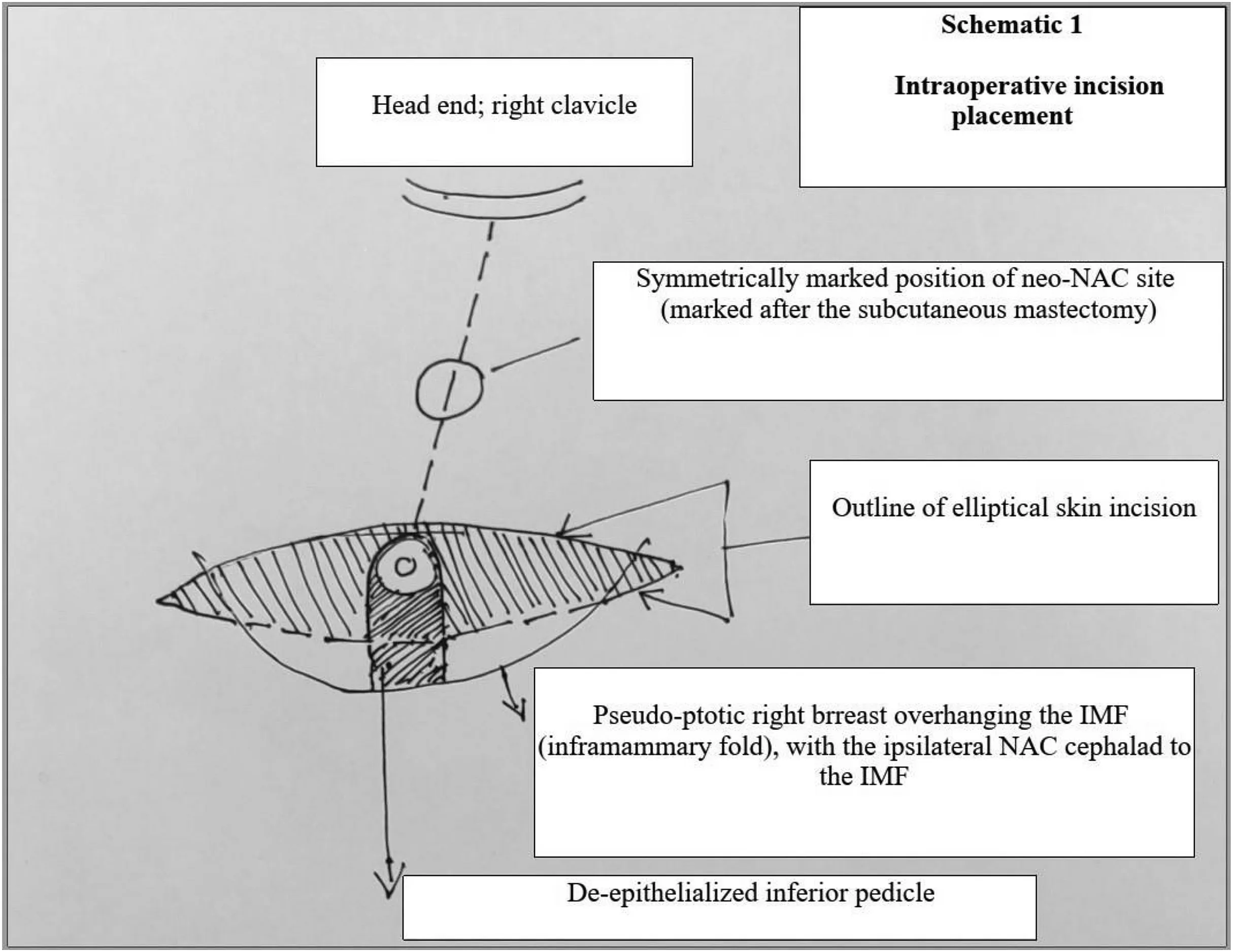
Fig.2.Intraoperative incision placement schematic.
The mastectomy specimens were weighed separately (Fig.3).An inferior-pedicled nipple flap was fashioned bilaterally (Fig.4),taking care to keep the flaps broad-based,on the inframammary fold,while tapering toward the apex,to ensure good vascularity of the nipple-areola complexes(NAC);the neo-nipple areola site was marked on either side.

Fig.3.Subcutaneous mastectomy specimens.Right,322 g;left,345 g.
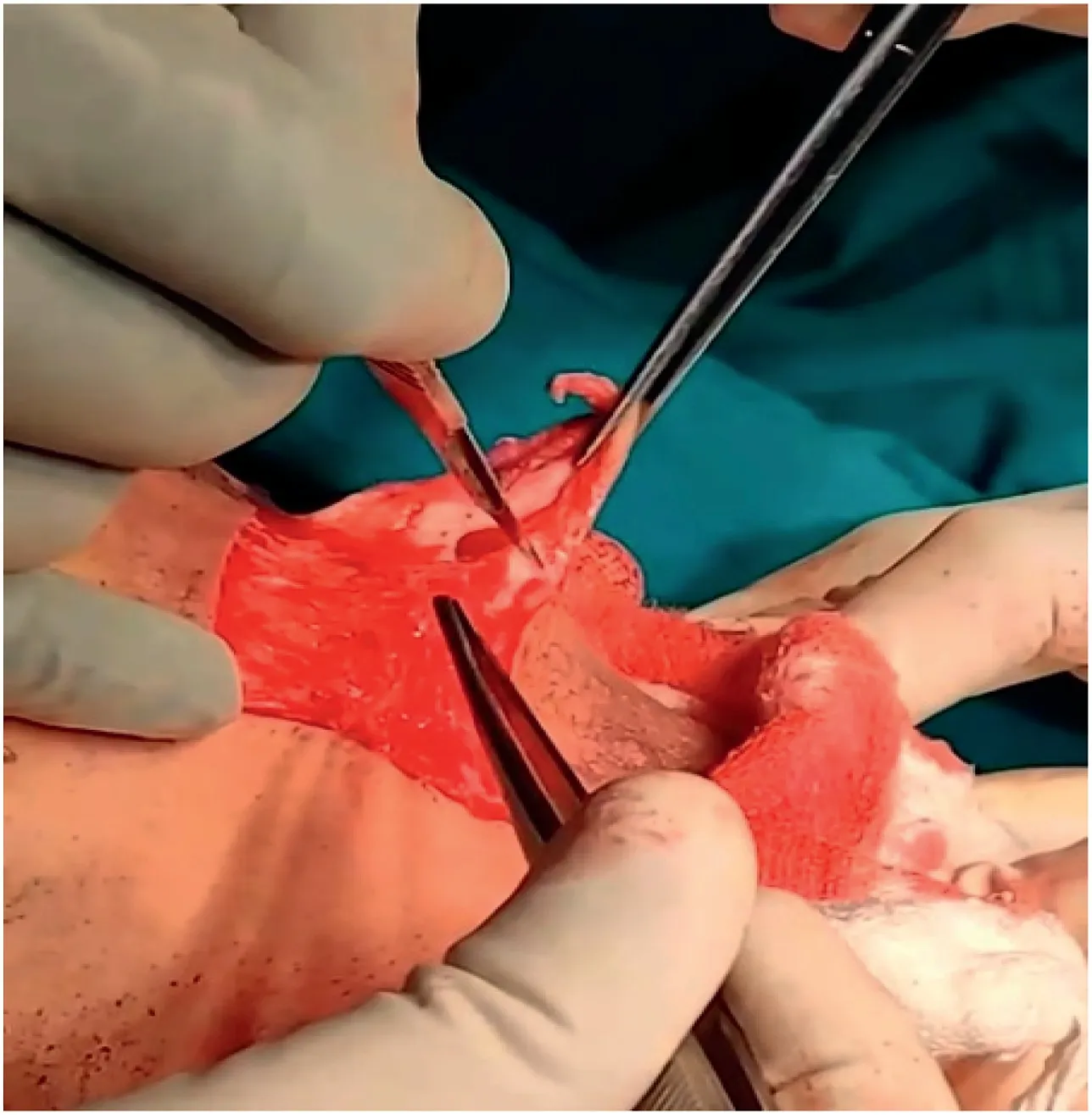
Fig.4.Fashioning the de-epithelialized inferior pedicle flap.
A circular skin segment was excised 5 mm smaller in diameter than the NAC ipsilaterally,and the pedicled flap was tunneled subcutaneously to the excised skin site.Care was taken to trim the pedicle sufficiently to prevent bulging and,at the same time,to prevent saucerization defects at the new site.The neo-nipple areola was fashioned using subcuticular 4-0 monocryl sutures.Jackson Pratt drains(12 Fr)were placed posterior to the flaps,and the superior mastectomy flaps were sutured to the inframammary groove incision site with 4-0 subcuticular monocryl sutures (Figs.5 and 6).

Fig.5.The completed procedure,with the inferior subdermal pedicles outlined in broken blue lines.
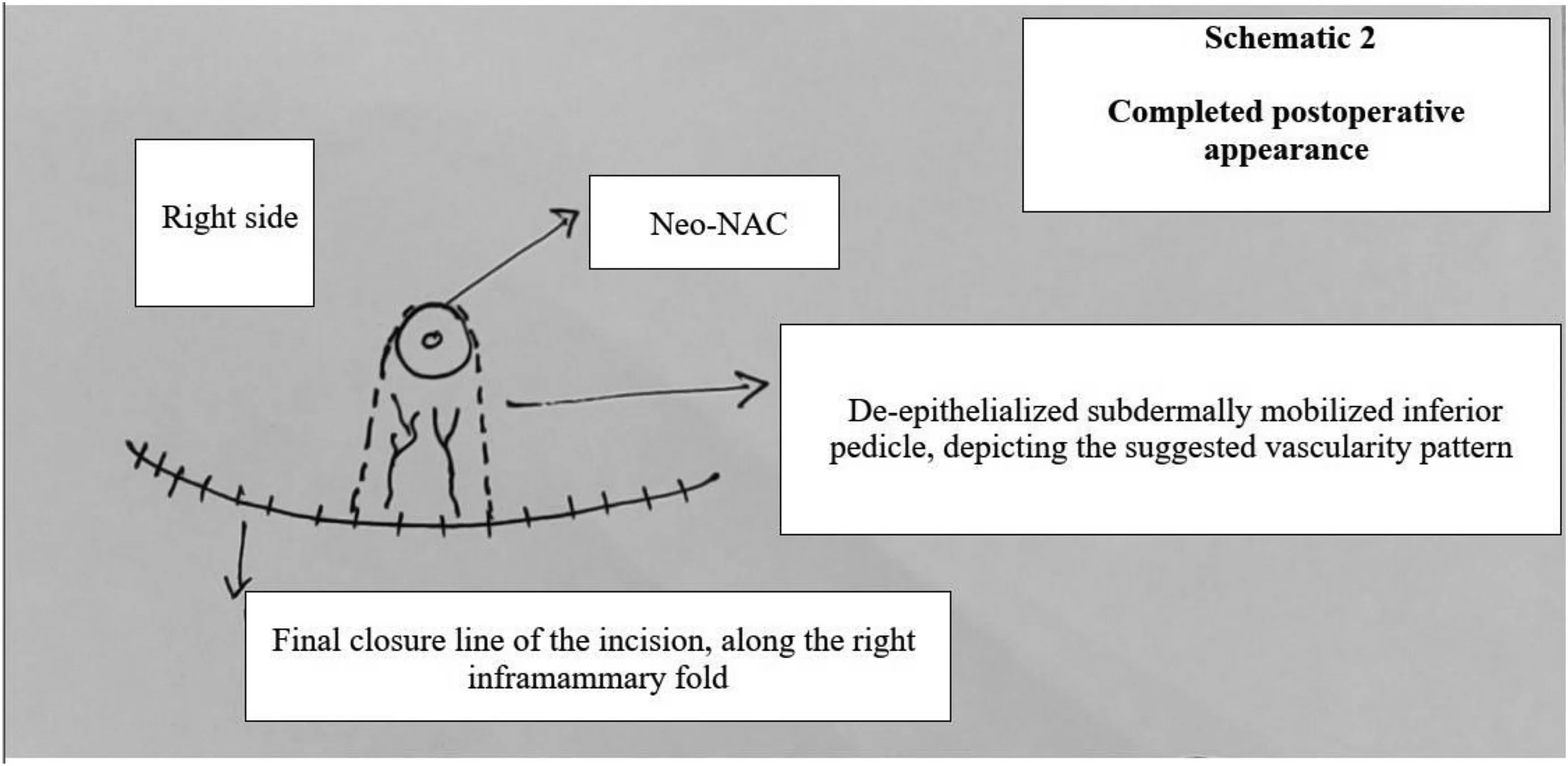
Fig.6.Schematic of the completed procedure with the inferior subdermal pedicle outlined in broken lines.
The patient recovered uneventfully and was discharged on the 3rd postoperative day.No complications,such as hematoma,seroma,surgical site infection,or skin necrosis,were noted at any time.Both drains were removed on the 5th postoperative day at the outpatient visit.Follow-up visits were planned at 2 weeks,4 weeks(Fig.7),3 months,and 6 months.The new nipple-areola site healed without notable contraction,and scarring was minimal.No necrosis was observed at any of the surgical sites,and no contour anomalies were noted at any time during follow-up.The nipple-areola sensations remained intact during the postoperative period.

Fig.7.Four weeks postoperatively.
3.Discussion
The very fact that there are several surgical options are available for the treatment of severe gynecomastia(Simon 2b/3,Rohrich III/IV,with ptosis)suggests that no single option has been validated as being the best.The choices are largely dependent on surgeon preference,5and each procedure has its own merits and demerits.Most of the procedures were designed for reduction mastopexy of the female breast,and hence pose significant challenges when applied to male breasts with a much lower breast-skin ratio and variable vascularity of the flaps.
Overweight patients with pseudogynecomastia should preferentially be treated using techniques that allow for greater tissue removal and NAC repositioning.8Traditionally,such patients would be offered a NAC graft or techniques using an areolar pedicle flap.
Among the latter,choices vary between the superior,inferior,central,medial,superolateral,8or superomedial pedicles.NAC grafting is a simple technique,but it is fraught with lack of sensitivity of the NAC,the chance of graft non-integrity with the risk of pathological scarring and necrosis,and mainly,the need for dressing and special care of the graft for as long as 2 weeks postoperatively.Techniques based on pedicles usually preserve the tactile sensitivity of the NAC.9For most patients with moderate to severe gynecomastia,peri-areolar excisions and skin resections should suffice;however,for patients with severe gynecomastia associated with various grades of ptotic NAC,extra-areolar incisions and scars might be needed.Wise pattern reduction has become an essential tool for severe gynecomastia surgeons,with some esthetic and scar tissue concerns associated with the vertical component of the scar,leading to a search for more cosmetic incision placements.
The first report of vertical scarless mastopexy is attributed to Passot;he performed the procedure using an inferior-pedicled flap and published the report in 1925.Excess fatty tissue was removed as a wedge from only the inferior pole of the breast.10Lalonde11described a similar horizontally oriented wedge excision,not extending as far back as the Passot scar,with a similar button-holing siting of the new nipple position.The technique was aimed at lowering the risk of scar hypertrophy or keloid development over the vertical aspect of the Wise pattern scar in the inclined population.Kazzazi and Malata12described similar techniques.The resulting horizontal skin flaps allow resection of significant redundant and flaccid tissues as they can extend to the posterior axillary line or the back,in cases where it is associated with torsoplasty;furthermore,this restores the masculinity of the chest with final positioning of the scar in the submammary fold,in the transition between the chest and the abdomen,which makes it aesthetically acceptable in the long run.This is especially useful in patients with pseudogynecomastia and excessive redundant skin after metabolic surgery or weight loss due to other reasons.
The Passot technique is associated with several possible issues.The scar on the submammary fold may develop the same complications as the vertical scar that it does away with.Additionally,hematoma,seroma,and wound breakdown,along with NAC necrosis,although rare,may still be seen.The risk of flap weight-related postoperative ptosis,addressed by Thiénot,can be managed by maintaining a narrow base of the flap with gradual tapering toward the NAC and excising adequate fat from the superior flap so that the pedicle can be accommodated without unwanted bulging and additional weight,adding to a better esthetic value and a lower possibility of subsequent ptosis.13The posterolateral extension of the scar can be curtailed in most men and seldom stretches beyond the mid-axillary line,leading to better overall acceptability.Finally,the Passot technique has an individually tailored place,depending on multiple factors,in the surgical management of severe gynecomastia,while the more conventional techniques suffice for most patients with smaller grades of the disease.
4.Conclusion
The Passot technique,with no vertical scar and with NAC transposition,is an effective technique for the surgical treatment of severe gynecomastia as it allows for wide tissue resection,with low morbidity and good esthetic and functional outcomes.It should be more widely promoted,with reservations,in the surgical correction of the severe grades of gynecomastia,especially those associated with ptosis and postweight-loss skin and tissue redundancy.
Ethics approval and consent to participate
The need for ethical approval and consent to participate was waived due to the retrospective nature of this study.
Consent for publication
Due written consent was obtained from the patient and his guardians regarding the publication of data and images.
Competing interests
None.
Author's contributions
Mohanty A:Conceptualization;Data curation;Formal analysis;Investigation;Methodology;Project administration;Resources;Software;Supervision;Validation;Visualization;Writing-Original draft;Writing-Review and editing.
Acknowledgments
I acknowledge the trust and willingness of my patient and the residents and staff who were instrumental in his speedy recovery.
 Chinese Journal of Plastic and Reconstructive Surgery2022年1期
Chinese Journal of Plastic and Reconstructive Surgery2022年1期
- Chinese Journal of Plastic and Reconstructive Surgery的其它文章
- Clinical applications of paraumbilical perforator flaps in multiple angiosomes for the reconstruction of the upper limbs
- Foreword from Dr.Chin-Ho Wong
- Effect of local massage on prevention and treatment of intra-arterial polymethyl methacrylate embolism complications:An experimental animal study
- External application of a Nocardia rubra cell wall skeleton in the treatment of diabetic foot ulcers
- Polyacrylamide gel migration after injection for breast augmentation:A case report
- Misdiagnosis of malignant meningioma in subcutaneous soft tissue of the forehead:A case report
