孤独症谱系障碍儿童动作协调能力与运动区皮质静息功能连接的特征分析
张亚茹 文世林 张雪冬 李文意 陈功 李雅 王子鑫 李倩倩 魏兵


摘 要:目的:明確孤独症谱系障碍(ASD)儿童动作协调能力与运动区皮质静息功能连接的关系。方法:共招募11名ASD儿童和20名典型发展儿童(TD)。应用儿童协调能力测量量表(M-ABC2)测试动作协调能力,用近红外光谱技术(fNIRS)监测运动区皮质静息态的血氧信号变化,并用“FC-NIRS”软件计算运动区皮质的静息功能连接(RSFC)强度。结果:ASD组的M-ABC2总分显著低于同龄的TD组[t (n=29)=-11.550,p=0.000],且精细动作能力(U=0,Z=-4.561,p=0.000)、手眼协调能力[t (n=29)=
-10.204,p=0.000]及静态和动态平衡能力[t (n=29)=-5.752,p=0.000]存在显著差异。ASD组的RSFC强度均值显著低于TD组[在HbO信号水平上,t (n=29)=-3.740,p=0.001],且脑右侧运动区存在差异的功能连接“边”的数量多于左侧。M-ABC总分与运动区RSFC均值之间存在显著相关[在HbO信号水平上,r=0.497,p=0.004],但在M-ABC2各二级指标上均与RSFC无相关性。结论:孤独症谱系障碍儿童的动作协调能力和运动区静息功能连接强度的发展均滞后于同龄的典型发展儿童,但是动作协调能力的损伤不一定与运动区功能连接强度的减弱有关。
关键词:孤独症谱系障碍; 动作协调能力; 运动区皮质; 静息功能连接; 近红外光谱技术
中图分类号:G 804.55 学科代码:040303 文献标识码:A
Abstract:Objective: To clarify the relationship between motor coordination ability and resting function of motor cortex in children with autism spectrum disorder (ASD).Methods: A total of 11 children with ASD and 20 typically developing(TD)children were recruited. First, the Movement Assessment Battery for Children - second edition (M-ABC2) Checklist was administered to assess the motor coordination ability. Second, changes in the motor area's blood oxygen signals in resting states were collected by functional near infrared spectroscopy (fNIRS). Finally, FC-NIRS software was used to calculate the Resting State Functional Connectivity (RSFC) of the cortical motor area. Results: the total scores of the M-ABC2 of the ASD children were significant lower than the age-matched TD children (t(n=29) =-11.550, p=0.000), and the differences were also significant in fine hands motor ability (U=0,Z=-4.561,p=0.000), hand-eye coordination ability (t(n=29)= -10.204, p=0.000), and static and dynamic balance ability (t(n=29) =-5.752, p=0.000). The mean value of the RSFC strength of ASD children was significant lower than the control group (at the HbO signals level, t(n=29) =-3.740, p=0.001) as well as numbers of the“edges”of the RSFC in the right motor area of the brain were greater than the left. Though there was a significant correlation between the total score of the M-ABC2 and the mean value of the RSFC strength (at the HbO signals level, r=0.497, p=0.004) within all subjects, no significant correlation was found at each group. Conclusions: Both the development of the motor coordination ability and the RSFC of the motor area of the ASD children lagged far behind the age-matched TD children, and the impairment in the motor coordination ability had no relationships to the decrease of the RSFC of the motor area.4435031E-261A-4E37-9ED9-2ECDDCBC066B
Keywords:autism spectrum disorder; coordination ability; motor area cortex; Resting State Functional Connectivity;fNIRS
孤独症谱系障碍(Autism Spectrum Disorder,ASD)是一种极其复杂的神经发育障碍,主要特征为社会交往、语言交流障碍和重复刻板行为[1]。据世界卫生组织(WHO)统计,全球约有6 700万ASD患者,且ASD患病后是发展最快的发育障碍之一[2]。ASD患者一生都会存在语言交流、社会交往方面的缺陷[3-4],这些缺陷不仅影响其参与标准化教育和就业,还严重地影响其日常生活质量[5],同时也会对其监护人或家庭造成巨大负担。
目前,ASD的病因不明,关于其病因的研究主要集中在遗传学[6-7]及大脑的结构和功能[8-11]等方面。其中,在大脑功能的研究中,脑区功能连接是重要的研究方向之一,该方面的研究主要探索大脑远程脑区神经信号的相互依赖或同步[12]及连接强弱[13]。近年来,研究者发现在静息状态下,这些以低频(<0.1 Hz)为特征的振荡可以在没有任务的情况下发生,且相关功能脑区之间存在關联[14-15],这种关联被称为静息功能连接(resting-state functional connectivity,RSFC)。RSFC旨在反映静息状态下自发性神经元活动的脑血流动力学波动,已被研究证实的静息态网络包括:运动、听觉、视觉、注意和默认网络[16],且这些网络在受试者之间甚至跨物种之间是一致的[17-18]。有研究表明,患有阿尔兹海默病[17]、精神分裂症[19]、孤独症[20]、癫痫[21]、多发性硬化症[22]等疾病的患者的大脑RSFC通常会发生改变。因此,对患者脑区RSFC进行研究将会为相应疾病的预测、诊断和愈后康复提供参考。
ASD儿童存在广泛的运动障碍,例如:步态、姿势的协调和模仿等问题,但是这些运动障碍与大脑连接异常的原因不明确[23]。ASD患者在婴儿期就可能出现动作能力的异常[24],例如整体动作能力和精细动作能力的损伤[25-26]。在整体动作能力方面,ASD儿童表现出较弱的姿势控制力[27]、不稳定的步态[28]及双侧协调动作能力受损[25, 29]。同样,与同龄的TD儿童相比,ASD儿童在瞄准控制和手部灵巧[30]、视觉运动整合[31]和用手书写[32]等精细动作方面发展滞后。也有研究表明,学龄前ASD儿童的粗大动作和精细动作能力接近同龄的典型发展儿童(typical development,TD)[33]。但是多数研究显示,ASD儿童在动作能力发展上出现了滞后或受损,且这些问题已对其参加各类集体活动造成了负面影响,并相应减少了其获得人际语言交流、社会交往和建立友谊的机会[34-35]。此外,动作能力的发展会随ASD儿童年龄的增长而出现退化的现象[36],从而进一步影响其学业成绩[37]和日常生活[38]。
虽然有研究表明,ASD儿童的动作能力滞后于同龄的一般儿童[39],但是动作能力行为指标和运动区RSFC之间的关系仍不明确。在最新的研究中,Cai等[40]对ASD基因特征、神经回路和行为学之间的因果链进行了研究,在动物模型(猴)的研究中发现MECP2的共表达基因显著富集于GABA相关的信号通路,且额-顶-枕网络内β带同步降低与异常行为表现相关。该研究还进一步对ASD患者的功能连接模式进行了验证,发现ASD患者的不良功能连接情形与猴子实验的结果一致。上述研究通过建立遗传学、神经通路和行为学的证据链,为解构临床异质性和推进精神障碍的准确诊断提供了新依据,同时也为进一步探索动作能力与运动区RSFC的关系提供了思路。
基于此,本研究提出如下假设:ASD儿童和TD儿童的动作协调能力和运动区RSFC均存在差异,且动作协调能力测试得分与RSFC具有相关性。研究拟应用fNIRS设备探索ASD儿童运动区RSFC的特征,并进一步探索其与动作协调能力的关系。
1 研究方法
1.1 实验对象
招募北京市海淀区某特殊学校的ASD儿童11人,某小学的TD儿童20人。受试者入组标准为:1)ASD组需持有诊断证明或残疾证;TD组需智力与精神正常,就读于普通小学。2)年龄在8~12岁之间。3)具备遵循指令并执行所需完成动作任务的能力。4)剔除患有脑外伤、心肺疾病、鼻炎等疾病的受试者。5)右利手。该实验获得首都体育学院伦理道德委员会的审批。实验前分别获得了受试者及其父母的知情同意,由受试者父母代其签署知情同意书,并填写孤独症儿童行为量表(autism behavior checklist,ABC量表),ABC量表得分情况见图1。
ASD组的ABC量表得分为(53.36±28.16),相应的自闭程度等级处于水平二和水平三之间。其中6名受试者的得分高于62分(存在孤独症症状),另外5名受试者在31分左右(疑似孤独症症状)。
1.2 动作协调能力测试(M-ABC2)
M-ABC2是一种获得了国际认可且被广泛应用的运动评估工具[41],可用于筛查ASD儿童的动作协调能力[42-44]。本研究主要应用M-ABC2测试手部灵活性、瞄准与捕捉、静态平衡能力与动态平衡能力3个方面,评估受试者的手部精细动作、手眼协调动作以及静态平衡能力和动态平衡能力。主试严格按照M-ABC2的测试标准执行,并根据受试者的测试表现如实填写相关测评记录表。M-ABC2由8个子测试组成,这些子测试构成了总运动分数,且M-ABC2结构的有效性已通过有关研究的验证[45]。手动灵活性项目包括3个子测试:单手钉板测试、定时双手组装测试和不定时绘图测试;瞄准与捕捉项目包括2个子测试:向目标投掷物体和通过单手或双手捕捉物体的测试;平衡性项目包括1个静态平衡测试和2个动态平衡测试,其中动态平衡测试包括接脚前进和单脚跳格。整个测试过程大约持续25 min。4435031E-261A-4E37-9ED9-2ECDDCBC066B
1.3 fNIRS测试
本研究应用便携式“fNIRS”系统(LIGHTNIRS,日本岛津公司),该系统采用3个波长(780 nm、805 nm、830 nm)近红外光检测人体脑组织血氧信号的变化。按照4×2(R)和4×2(L)安装了8个发射光极和8个接收光极。其中,单数光极配置在左侧光极帽,双数光极配置在右侧,共构成20个测量通道(CH1~CH20),如图3-(a)、图3-(b)所示。佩戴fNIRS光极帽方法:首先,确定头顶正中点(Cz),即鼻根至枕骨隆突的连线与双侧外耳孔连线的交汇点。在Cz点前1~2 cm处放置7号光发射器和2号光探测器,光极帽测量面板基本覆盖受试者的运动区,见图3-(c)。戴帽完毕后,对探头组进行检查和调整,以确保所有受试者佩戴光极帽的位置一致。采样频率设为10 Hz,在静息状态下连续扫描脑部5 min。
1.4 RSFC计算
将采集的原始数据导入 “LightNIRS”分析系统,将HbO、HbR、HbT 3个血氧信号及光强信号转化为文本格式(TXT格式)保存到存储器。在“MATLAB”数据平台上运行“FC-NIRS”[46]软件包,fNIRS测试数据计算的流程如下:1)质量控制。通过质量控制模块检测运动伪影,计算信噪比(SNR),以及標定坏导并剔除不合格数据。2)预处理。在预处理阶段,应用修正的比尔-朗伯定律将每个通道的光强信号转换为HbO、HbR和HbT浓度信号。采用0.01~0.1 Hz之间的带通,消除低频噪声。应用“样条插值法”和“相关信号改进法”减少运动伪影对数据的污染。此外,采用直线最小二乘拟合对线性趋势进行矫正。3)功能连接计算。取两两连接通道的平均相关系数(r值)为通道之间的功能连接值,进一步计算群组的RSFC值。
1.5 数理统计法
应用“MATLAB”数据处理平台对由190条“边”组成的Z值矩阵进行独立样本t检验,计算功能连接强度的整体均值和每条边的组间差异。应用“SPSS Statistics 22.0”软件对RSFC和动作协调能力的数据进行双变量相关分析。
2 研究结果
2.1 受试者基本情况
年龄(ASD组的Shapiro-Wilk检验值为0.97,n=11,p=0.85;TD组检验值为0.87,n=20,p=0.01)不呈正态分布。采用U检验进行组间比较,结果显示差异不显著(U=80.50,Z=-1.22,p=0.22)。身高(ASD=146.82±14.10,TD=141.40±8.14,t=1.36,p=0.18)和体质量(ASD=
38.55±11.24,TD=34.75±3.95,t=0.65,p=0.30)的组间差异也不显著(见表1)。
2.2 ASD组M-ABC2得分情况
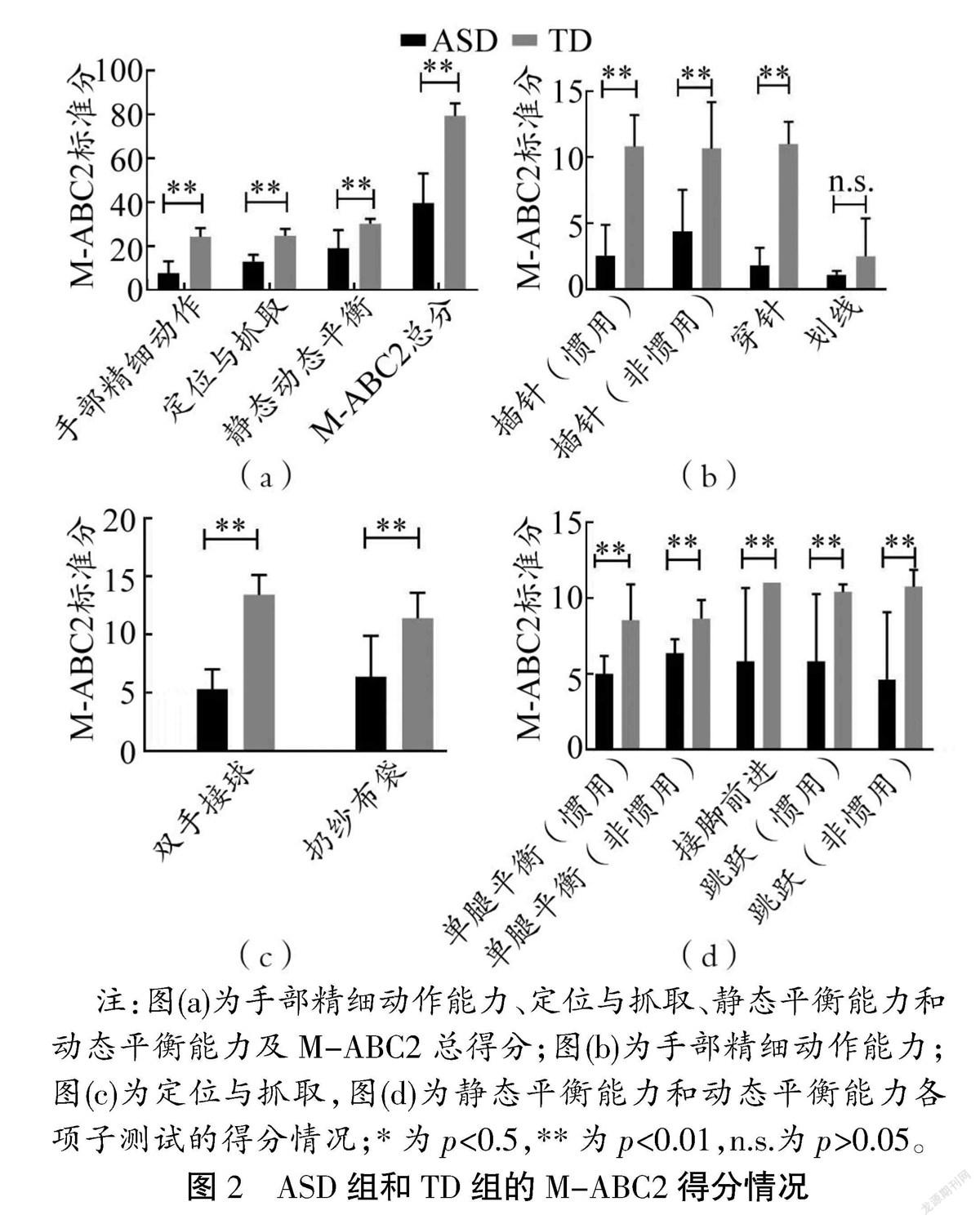
在M-ABC2测试结束后,将测试成绩录入“M-ABC2”测试系统进行统一评价,得到总分和各项子测试的标准分。对M-ABC2总分、手部精细动作、定位与抓取能力、静态平衡能力与动态平衡能力4个主要指标的得分进行了正态性检验(用Shapiro-Wilk方法检验)。检验结果显示,除ASD组的手部精细动作得分(Shapiro-Wilk检验值为0.850,n=11,p=0.043)未通过检验,其他数值均符合正态分布。根据统计要求,对符合正态性的指标进行t检验,而不符合正态分布的指标则使用U检验。ASD组和TD组的M-ABC2标准分对比结果如图2所示。
ASD组的M-ABC2总得分均值(39.64±13.52)显著低于TD组[(79.40±5.67),t(n=29)=-11.55,p=0.000]。在精细动作能力方面,ASD组(平均秩次为6.00)与TD组(平均秩次为21.50)具有显著差异(U=0,Z=-4.561,p=0.000);在手眼协调能力方面,ASD组(11.73±3.44)与TD组(24.80±3.04)具有显著性差异[t (n=29)=-10.95,p=0.000];在静态平衡能力和动态平衡能力方面,ASD组(19.00±8.40)与TD组(30.30±2.16)具有显著性差异[t(n=29)=-5.75,p=0.000)],见图2-(a)。
用同样方法对M-ABC2各子项目的得分进行对比分析。本研究显示,除“划线”得分ASD组(平均秩次为14.18)与TD组(平均秩次为17.00)不具有显著差异(U=90.0,p=0.427),其他项目均具有显著差异,如图2-(b)、图2-(c)、图2-(d)所示。上述研究表明,ASD儿童的动作协调能力显著滞后于TD儿童。
2.3 ASD组运动区RSFC的特征
通过脑网络软件(FC-NIRS)的计算,得到了3种血氧信号水平(HbO、HbR和HbT)的RSFC值。正态性检验结果显示:在HbO信号水平上,ASD组的RSFC值(Shapiro-Wilk检验值为0.654,n=11,p=0.000)未通过正态性检验,但是其他各血氧信号水平的各组数值均符合正态分布。t检验和U检验结果显示,在HbO信号水平上,ASD组(平均秩次为8.45)与TD组(平均秩次为20.15)具有显著性差异(U=27,Z=-3.427,p=0.000)。在HbR(t (n=29)=-3.87,p=0.000)和HbT(t (n=29)=-2.78,p=0.000)信号水平上,RSFC均值同样具有显著性差异。本研究进一步比较了ASD组和TD组运动区的190条“边”的组间差异(数据呈正态分布,Shapiro-Wilk检验,独立样本t检验)。结果显示,在ASD组和TD组运动区的190条“边”的比较中(经FDR校正后),HbO有19 条“边”(见图3-f),HbR有23条“边”,HbT为0,存在显著差异。本研究进一步将这些存在差异的“边”所对应分布的左右运动区进行提取(见表2),结果显示,右侧运动区功能连接存在差异的“边”最多(n=20),其次是左-右运动区的“边”(n=15),左侧运动区功能连接存在差异的“边”最少(n=7),且在HbO和HbR信号水平上,所有的t值均为负值。上述结果表明,相比TD组,ASD组运动区RSFC强度在右侧脑区的差异最大。4435031E-261A-4E37-9ED9-2ECDDCBC066B
2.4 运动区RSFC与动作协调能力得分的关系
取HbO和HbR两种信号(HbT信号的信效度相对较低)的RSFC均值,按总体和各群组对RSFC均值与M-ABC2总分及二级动作协调能力指标进行相关性检验,结果如图4和图5所示。
在总体上,RSFC均值与M-ABC2总分存在显著相关性(HbO信号水平,r=0.50,p=0.004;HbR信号水平,r=0.69,p=0.000),见图4。本研究进一步对RSFC均值和M-ABC2二级指标进行了相关性检验。结果显示,在HbO信号水平时,手部灵活性(r=0.572,p=0.001)、瞄准与捕捉(r=0.496,p=0.005)及静态平衡能力与动态平衡能力(r=0.509,p=0.003)均具有显著相关性。在HbR信号水平时,手部灵活性(r=0.708,p=0.000)、瞄准与捕捉(r=0.603,p=0.000)、静态平衡能力与动态平衡能力(r=0.577,p=0.001)也具有显著相关性。以上结果说明儿童动作协调能力可能与运动区RSFC有关。
但是在各群组中,ASD组的RSFC均值与M-ABC2总分及二级指标之间均无相关性,且TD组也无显著相关性。结果表明,ASD儿童在手部精细动作、定位与抓取能力、静态平衡能力与动态平衡能力方面存在的发展障碍与运动区的RSFC减弱不一定具有直接相关性。
3 讨论
3.1 ASD组M-ABC2测试过程表现出的非典型特征
M-ABC2测试结果显示,ASD组的得分普遍低于TD组。同时,在测试过程中,相比同龄TD组,ASD组的行为也表现出了非典型特征。例如,在手动灵活性的测试中,在最后一次测试时表现出了烦躁或试图终止测试的问题行为;在穿线测试时,手指动作较为笨拙,容易出现前后绕着穿的问题;描画轨迹时,手部肌肉僵硬、按笔较重或不看描画轨迹就行笔,且错误次数明显多于TD组;在双手接球的测试中,接球动作僵硬,缺少主动接球的意识;在投掷豆袋测试中,不看垫子就将豆袋扔出,且投掷力度调整不精确;在单足站立测试中,难以找到平衡点,容易出现任务失败;在跳格的测试中,不看格子,身体动作僵硬。
虽然大多数受试者家长反映其在康复机构接受过动作能力的康复训练,受试者已具备一定的动作能力基础,但是此次测试的结果却不令人满意。此外,对个别难于理解的项目,主试在测试前给被试反复示范并组织练习直至其掌握测试要领,未出现不理解动作目的而进行测试的情况。因此,上述情况出现的原因可能是:ASD儿童动作技能泛化和迁移能力弱,或存在已习得的运动技能出现遗忘或退化的现象。
3.2 ASD儿童动作协调能力发展滞后的可能性原因
ASD儿童普遍存在手势功能障碍[33],且在临床上约有67%的高功能ASD儿童有严重的精细动作障碍[47]。ASD儿童精细动作能力发展滞后的可能性原因是:模仿能力受损和运动计划不良[48]、难以理解运动目标[49]。本研究显示,ASD组精细运动技能滞后于TD组,与已有的相关研究结果一致。精细动作能力发展的滞后可能会对其早期学习和生活自理能力产生较大影响[50],因此,应该重视对ASD儿童进行精细动作技能的干预训练。
ASD儿童对力的掌握和调节存在问题[51],且存在明显的动作协调能力缺陷[52]。在投掷和接物的操纵测试中,ASD儿童可能会表现出动作协调能力发展滞后,物体操纵能力不佳,动作模仿能力不足,以及动作发展障碍的问题[53]。在定位与捕捉运动测试时,ASD儿童在投掷或接球过程中很难控制投球或接球的力量和方向[54],與同龄的TD儿童相比,6~10岁的ASD儿童在运用特定运动技能(例如飞奔、跳跃)和物体控制技能(例如击打、运球、接球、横滚)时存在明显的障碍[39]。
ASD儿童存在站立平衡和姿势矫正的障碍[55],有研究表明其足底压力中心(COP)的标准化正中侧外摆值和质心分离值显著高于TD儿童[56]。如果要维持单腿平衡,需要人体精准地响应下肢本体感受器的传入反馈,通过对下肢肌肉进行增益调整来维持平衡[57]。上述过程除需感觉运动控制系统的主动参与,还需综合多个感觉系统(例如视觉、前庭觉和本体感觉系统)整合信息,并基于神经反馈迅速矫正动作[58],ASD儿童可能在感知觉信息的整合方面存在缺陷,致使其难以在非平衡条件下保持身体姿势的稳定。而在日常生活中,平衡能力很重要,例如完成穿衣、洗澡、骑自行车等各类活动[59],ASD儿童在平衡能力上的缺陷可能会严重影响其自理能力、社交能力和生活质量[60]。
3.3 运动区RSFC与ASD儿童动作协调能力的关系
ASD儿童大脑运动区功能连接异常可能是导致其难以熟练执行手势[40],以及难于使用工具和模仿手势[53]的原因。辅助运动区(SMA)和初级运动皮层的活动与步态启动有关[61],且与手和脚的有节奏运动和肢体协调高度相关[62]。运动皮层对维持正常步态具有重要作用[63-64],在动态平衡任务执行过程中,大脑辅助运动皮层可控制身体不发生左右摆动[65]。因此,运动区皮质功能连接的异常可能会严重影响动作的协调性和身体姿势的稳定性[66]。
有研究表明,运动区功能连接以及跨网络的神经通路可能与动作协调能力有关[67-68],躯体运动区位于大脑中央沟的前侧,主要通过空间感觉和运动规划来控制人体的运动[69]。在本研究中,左脑和右脑的运动区RSFC存在显著的组间差异,如表2所示,ASD组右脑运动区有多条功能连接“边”的强度显著低于对照组。本研究结果佐证了:1)ASD儿童的运动区RSFC未出现偏侧化异常;2)儿童动作协调能力可能与大脑运动区功能连接(RSFC)有关。
又有研究表明,运动系统存在利手之间的不对称性[70],例如右利手者的大脑左侧中央沟比左利手者深,反之,左利手者的大脑右侧中央沟比右利手者深。功能性磁共振成像(fMRI)研究表明,初级运动皮层(M1)具有明显的利手半球优势,且半球优势与动作表征能力相关[71]。在本研究中,ASD受试者均为右利手,测试结果显示其左脑运动区的RSFC强度优于右脑运动区,且与TD组相比,左脑运动区存在差异“边”的数量少于右脑(见表2)。这表明,ASD儿童的大脑运动区的发展与TD儿童一致,也存在利手的不对称性,未出现偏侧化异常的现象。4435031E-261A-4E37-9ED9-2ECDDCBC066B
還有研究发现,与TD儿童相比,在第3个月和第6个月时ASD儿童的兄弟姐妹表现出更多的动作发展问题。例如,早期运动发展延迟、运动率低、运动变异性大、人际同步性弱[72]等。学龄ASD儿童的动作能力也存在预期的发展滞后[73],与TD儿童相比,其在基础运动等多项测试中得分较低[74]。虽然ASD儿童动作能力发展明显滞后,但由于其临床表现的多样性和复杂性,很难对其潜在的神经生物学机制进行解释。近年来,有研究将ASD个体的脑网络连通异常与特定症状进行关联分析[75-77],例如:有研究者通过fMRI技术测试ASD患者脑网络同步或功能连接异常[78]时发现,相比对照组,ASD患者大脑皮层区域的功能连接数量不足。此外,有一项静息态fMRI研究显示,ASD患者虽然在胼胝体体积和灰质半球间连通性均出现了显著降低,但未见两者之间存在直接的关联,这表明结构和功能指标是用来衡量半球间连通性的两个不同方面[79]。虽然本研究支持运动区RSFC与动作协调能力有关的观点,但是不足以证明ASD儿童动作协调能力受损与运动区RSFC降低直接相关,这个问题仍有待进一步研究论证。
3.4 研究不足之处
1)虽然fNIRS设备有良好的生态效度,对脑动噪声的容忍度较高,但是ASD儿童的安坐能力较差,选择合适的受试者比较困难,本研究仅纳入了11名ASD受试者,样本量偏小且年龄均值稍大于对照组。2)研究采用ABC量表对ASD受试者的自闭程度进行了评估,但是未对其智力发展水平等进行控制。
4 结论
孤独症谱系障碍儿童的动作协调能力和大脑运动区的静息功能连接强度均滞后于同年龄段以上能力和脑功能有典型的发展特征的儿童,但是动作协调能力的受损不一定与大脑运动区功能连接强度的减弱有关。
参考文献:
[1] GESCHWIND D H, LEVITT P. Autism spectrum disorders: developmental disconnection syndromes[J]. Curr Opin Neurobiol, 2007, 17(1): 103.
[2] JON BAIO E E A. Prevalence of autism spectrum disorder among children aged 8 years — autism and developmental disabilities monitoring network, 11 sites, united states, 2014[J]. Morbidity and Mortality Weekly Report, 2018,67(6):1.
[3] WOOLFENDEN S, SARKOZY V, RIDLEY G, et al. A systematic review of the diagnostic stability of autism spectrum disorder[J]. Research in Autism Spectrum Disorders, 2012, 6(1): 345.
[4] WORLEY J A, MATSON J L. Comparing symptoms of autism spectrum disorders using the current DSM-IV-TR diagnostic criteria and the proposed DSM-V diagnostic criteria[J]. Research in Autism Spectrum Disorders, 2012, 6(2): 965.
[5] FRITH U. Autism: a very short introduction[M]. New York: Oxford University, 2008:110.
[6] ABRAHAMS B S, GESCHWIND D H. Advances in autism genetics: on the threshold of a new neurobiology[J]. Nat Rev Genet, 2008,9(5): 341.
[7] DALLAGLIO L, MUKA T, CECIL C, et al. The role of epigenetic modifications in neurodevelopmental disorders: a systematic review[J]. Neurosci Biobehav Rev, 2018, 94: 17.
[8] ANAGNOSTOU E, TAYLOR M J. Review of neuroimaging in autism spectrum disorders: what have we learned and where we go from here[J]. Mol Autism, 2011, 2(1): 4.
[9] HERNANDEZ L M, RUDIE J D, GREEN S A, et al. Neural signatures of autism spectrum disorders: insights into brain network dynamics[J]. Neuropsychopharmacology, 2015,40(1): 171.
[10] PHILIP R C, DAUVERMANN M R, WHALLEY H C, et al. A systematic review and meta-analysis of the fMRI investigation of autism spectrum disorders[J]. Neurosci Biobehav Rev, 2012, 36(2): 901.4435031E-261A-4E37-9ED9-2ECDDCBC066B
[11] RAKIC M, CABEZAS M, KUSHIBAR K, et al. Improving the detection of autism spectrum disorder by combining structural and functional MRI information[J]. Neuroimage Clin, 2020, 25: 102181.
[12] WANG K, MENG L, LIANG W, et al. Altered functional connectivity in early alzheimers disease: a resting-state fMRI study[J]. Human Brain Mapping, 2010, 28(10):967.
[13] CORDES D, HAUGHTON V M, ARFANAKIS K, et al. Mapping functionally related regions of brain with functional connectivity MR imaging[J]. AJNR Am J Neuroradiol, 2000, 21(9): 1636.
[14] LOWE M J, MOCK B J, SORENSON J A. Functional connectivity in single and multislice echoplanar imaging using resting-state fluctuations[J]. NeuroImage, 1998, 7(2):119.
[15] BISWAL B, YETKIN F Z, HAUGHTON V M, et al. Functional connectivity in the motor cortex of resting human brain using echo-planar MRI[J]. Magn Reson Med, 1995, 34(4): 537.
[16] DE LUCA M ,BECKMANN C F ,DE STEFANO N , et al. fMRI resting state networks define distinct modes of long-distance interactions in the human brain[J]. NEUROIMAGE, 2006, 29(4): 1359.
[17] GREICIUS M D, SRIVASTAVA G, REISS A L, et al. Default-mode network activity distinguishes alzheimers disease from healthy aging: evidence from functional MRI[J]. Proc Natl Acad Sci U S A, 2004, 101(13): 4637.
[18] VINCENT J L, PATEL G H, FOX M D, et al. Intrinsic functional architecture in the anaesthetized monkey brain[J]. Nature, 2007, 447(7140): 83.
[19] LITTOW H, HUOSSA V, KARIJALAINEN S, et al. Aberrant functional connectivity in the default mode and central executive networks in subjects with schizophrenia - a whole-brain resting-state ICA study[J]. Front Psychiatry, 2015, 6:26.
[20] JUST M A, CHERKASSKY V L, KELLER T A, et al. Functional and anatomical cortical underconnectivity in autism: evidence from an fMRI study of an executive function task and corpus callosum morphometry[J]. Cereb Cortex, 2007, 17(4):951.[21] LUI S, OUYANG L, CHEN Q, et al. Differential interictal activity of the precuneus/posterior cingulate cortex revealed by resting state functional MRI at 3T in generalized vs. partial seizure[J]. Journal of Magnetic Resonance Imaging, 2008, 27(6):1214.
[22] LOWE M J, PHILLIPS M D, LURITO J T, et al. Multiple sclerosis: low-frequency temporal blood oxygen level-dependent fluctuations indicate reduced functional connectivity initial results[J]. Radiology, 2002, 224(1): 184.4435031E-261A-4E37-9ED9-2ECDDCBC066B
[23] JUST M A, KELLER T A, MALAVE V L, et al. Autism as a neural systems disorder: a theory of frontal-posterior underconnectivity[J]. Neuroscience & Biobehavioral Reviews, 2012, 36(4): 1292.
[24] ANJANA N, BHAT R J. Current perspectives on motor functioning in infants, children, and adults with autism spectrum disorders[J]. American Physical Therapy, 2011, 91(7):1116.
[25] FOURNIER K A, HASS C J, NAIK S K, et al. Motor coordination in autism spectrum disorders: a synthesis and meta-analysis[J]. Journal of Autism and Developmental Disorders, 2010, 40(10):1227.
[26] MARSH K L, ISENHOWER R W, RICHARDSON M J, et al. Autism and social disconnection in interpersonal rocking[J]. Front Integr Neurosci, 2013, 7: 4.
[27] SACREY L A, GERMANI T, BRYSON S E, et al. Reaching and grasping in autism spectrum disorder: a review of recent literature[J]. Front Neurol, 2014, 5: 6.
[28] HILTON C L, ZHANG Y, WHILTE M R, et al. Motor impairment in sibling pairs concordant and discordant for autism spectrum disorders[J]. Autism, 2012, 16(4): 430.
[29] DZIUK M A, GIDLEY L J, APOSTU A, et al. Dyspraxia in autism: association with motor, social, and communicative deficits[J]. Dev Med Child Neurol, 2007, 49(10): 734.
[30] ISENHOWER R W, MARSH K L, RICHARDSON M J, et al. Rhythmic bimanual coordination is impaired in young children with autism spectrum disorder[J]. Research in Autism Spectrum Disorders, 2012, 6(1): 25.
[31] KOPP S, BECKUNG E, GILLBERG C. Developmental coordination disorder and other motor control problems in girls with autism spectrum disorder and/or attention-deficit/hyperactivity disorder[J]. Research in Developmental Disabilities, 2010, 31(2): 350.
[32] KUNSHKI A, CHAU T, ANAGONSTOU E. Handwriting difficulties in children with autism spectrum disorders: a scoping review[J]. Journal of Autism and Developmental Disorders, 2011, 41(12):1706.
[33] PROVOST B H S L. Levels of gross and fine motor development in young children with autism spectrum disorder[J]. Physical and Occupational Therapy in Pediatrics, 2007, 3(27): 21.
[34] FREITAG C M, KLESER C, SCHNEIDER M, et al. Quantitative assessment of neuromotor function in adolescents with high functioning autism and asperger syndrome[J]. Journal of Autism and Developmental Disorders, 2007, 37(5):948.
[35] BHAT A N, LANDA R J, JAMES C C. Current perspectives on motor functioning in infants, children, and adults with autism spectrum disorders[J]. Physical Therapy, 2011, 91(7): 1116.4435031E-261A-4E37-9ED9-2ECDDCBC066B
[36] BROWN T, LALOR A. The movement assessment battery for children-second edition (MABC-2): A review and critique[J]. Physical & Occupational Therapy in Pediatrics, 2009, 29(1):86.
[37] KITA Y, SUZUKI K, HIRATA S, et al. Applicability of the movement assessment battery for children-second edition to Japanese children: a study of the age band 2[J]. Brain and Development, 2016, 38(8):706.
[38] AMENT K, MEJJA A, BUHLMAN R, et al. Evidence for specificity of motor impairments in catching and balance in children with autism[J]. Journal of Autism and Developmental Disorders, 2015, 45(3):742.
[39] PAN C Y T C. Fundamental movement skills in children diagnosed with autism spectrum disorders and attention deficit hyperactivity disorder[J]. Journal of Autism and Developmental Disorders, 2009(39): 1694.
[40] CAI D C, WANG Z, BO T, et al. MECP2 Duplication causes aberrant GABA pathways, circuits and behaviors in transgenic monkeys: neural mappings to patients with autism[J]. J Neurosci, 2020, 40(19):3799.
[41] MISSIUNA C R. Exploring assessment tools and the tar- get intervention for children with developmental coordination disorder[J]. Phys Occup Ther Pediatr, 2006, 26(1/2):71.
[42] CRAIG F, LORENZO A, LUCARELLI E, et al. Motor competency and social communication skills in preschool children with autism spectrum disorder[J]. Autism Res, 2018, 11(6): 893.
[43] LIU T, KELLY J, DAVIS L, et al. Nutrition, BMI and motor competence in children with autism spectrum disorder[J]. Medicina (Kaunas), 2019, 55(5):135.
[44] LIU T, BRESLIN C M. The effect of a picture activity schedule on performance of the MABC-2 for children with autism spectrum disorder[J]. Res Q Exerc Sport, 2013, 84(2): 206.
[45] SCHULZ J H. Structural validity of the movement ABC-2 test[J]. Res Develop Disabil, 2011(32): 1361.
[46] XU J, LIU X, ZHANG J, et al. FC-NIRS: A functional connectivity analysis tool for near-infrared spectroscopy data[J]. Biomed Res Int, 2015:1.
[47] MANJIVIONA J P. Comparison of asperger syndrome and high-functioning autistic children on a test of motor impairment[J]. Journal of Autism and Developmental Disorders, 1995(25):23.
[48] DEMYER M K, HINGTGEN J N, JACKSON R K. Infantile autism reviewed: a decade of research[J]. Schizophrenia Bulletin, 1981, 7(3): 388.
[49] FABBRI-DESTRO M C. Planning actions in autism[J]. Experimental Brain Research, 2009(192): 521.4435031E-261A-4E37-9ED9-2ECDDCBC066B
[50] JASMIN E, JASMIN E, COUTURE M, et al. Sensori-motor and daily living skills of preschool children with autism spectrum disorders[J]. Journal of Autism and Developmental Disorders, 2009, 39(2):231.
[51] MARI M M. Autism and movement disturbance[J]. Autism: Mind and brain, 2003: 225.
[52] GHAZIUDDIN M B. Clumsiness in autism and asperger syndrome: a further report[J]. Journal of Intellectual Disability Research, 1998, 1(42): 43.
[53] EGGLESTON M, WATKINS W, FRAMPTON C, et al. Coordination difficulties and self-esteem: the views of children, adolescents, and their parents[J]. Aust Occup Ther J, 2020, 67(5):437.
[54] REID G O C J. The autism spectrum disorders: physical activity instruction.[J]. Palaestra, 2003, 2(19): 20.
[55] PAPADOPOULOS N, MCGINLEY J, TONGE B, et al. Motor proficiency and emotional/behavioural disturbance in autism and aspergers disorder: another piece of the neurological puzzle?[J]. Autism, 2012, 16(6): 627.
[56] FOURNIER K A, KIMBERG C I, RADONOVICH K J, et al. Decreased static and dynamic postural control in children with autism spectrum disorders[J]. Gait Posture, 2010, 32(1): 6.
[57] GOWEN E, HAMILTON A. Motor abilities in autism: a review using a computational context[J]. J Autism Dev Disord, 2013, 43(2): 323.
[58] STEINDL R K. Effect of age and sex on maturation of sensory systems and balance control[J]. Developmental Medicine and Child Neurology, 2006(48): 477.
[59] JASMIN E C. Sensori-motor and daily living skills of preschool cwith autism spectrum disorders[J]. Journal of Autism and Developmental Disorders, 2009, 2(39):231.
[60] LEARY M R. Moving on autism and movement disturbance[J]. Mental Retardation, 1996, 1(34):39.
[61] YAZAWA S, SHIBASAKI H, IKEDA A, et al. Cortical mechanism underlying externally cued gait initiation studied by contingent negative variation[J]. Electroencephalography and Clinical Neurophysiology/Electromyography and Motor Control, 1997, 105(5): 390.
[62] DEBAERE F, SWINNEN S P, BEATSE E, et al. Brain areas involved in interlimb coordination: a distributed network[J]. Neuroimage, 2001, 14(5): 947.
[63] SUZUKI M, MIYAI I, ONO T, et al. Activities in the frontal cortex and gait performance are modulated by preparation: an fNIRS study[J]. NeuroImage, 2008, 39(2): 600.
[64] SUZUKI M, MIYAI I, ONO T, et al. Prefrontal and premotor cortices are involved in adapting walking and running speed on the treadmill: an optical imaging study[J]. Neuroimage, 2004, 23(3): 1020.4435031E-261A-4E37-9ED9-2ECDDCBC066B
[65] KARIM H, SCHMIDT B, DART D, et al. Functional near-infrared spectroscopy (fNIRS) of brain function during active balancing using a video game system[J]. Gait & Posture, 2012, 35(3): 367.
[66] DUYSENS J, SEVERENS M, NIENHUIS B. How can active cycling produce less brain activity than passive cycling?[J]. Clinical Neurophysiology, 2013, 124(2): 217.
[67] BARBER A D, SRINIVASAN P, JOEL S E, et al. Motor“dexterity”: evidence that left hemisphere lateralization of motor circuit connectivity Is associated with better motor performance in children[J]. Cerebral Cortex, 2012, 22(1):51.
[68] SEIDLER R, ERDENIZ B, KOPPELMANS V, et al. Associations between age, motor function, and resting state sensorimotor network connectivity in healthy older adults[J]. NeuroImage, 2015, 108: 47.
[69] FRANCESCHINI M A, FANTINI S, THOMPSON J H, et al. Hemodynamic evoked response of the sensorimotor cortex measured noninvasively with near-infrared optical imaging[J]. Psychophysiology, 2003, 40(4): 548.
[70] AMUNTS K, J?魧NCKE L, MOHLBERG H, et al. Interhemispheric asymmetry of the human motor cortex related to handedness and gender[J]. Neuropsychologia, 2000, 38(3): 304.
[71] HAMMOND G. Correlates of human handedness in primary motor cortex: a review and hypothesis[J]. Neurosci Biobehav Rev, 2002, 26(3): 285.
[72] STAPLES K L, REID G. Fundamental movement skills and autism spectrum disorders[J]. Journal of Autism and Developmental Disorders, 2010, 40(2): 209.
[73] BERKELEY S L. Locomotor and object control skills of children diagnosed with autism[J]. Adapted Physical Activity Quarterly, 2001(18): 405.
[74] LANDA R, GARRETT-MAYER E. Development in infants with autism spectrum disorders:a prospective study[J]. Journal of Child Psychology and Psychiatry, 2006, 47(6): 629.
[75] DINSTEIN I, PIERCE K, EYLER L, et al. Disrupted neural synchronization in toddlers with autism[J]. Neuron, 2011, 70(6): 1218.
[76] WENG S, WIGGINS J L, PELTIER S J, et al. Alterations of resting state functional connectivity in the default network in adolescents with autism spectrum disorders[J]. Brain Research, 2010, 1313(1): 202.
[77] UDDIN L Q, SUPEKAR K, LYNCH C J, et al. Salience network-based classification and prediction of symptom severity in children with autism[J]. JAMA Psychiatry, 2013, 70(8): 869.
[78] JUST M A, CHERKASSKY V L, KELLER T A, et al. Cortical activation and synchronization during sentence comprehension in high-functioning autism: evidence of underconnectivity[J]. Brain, 2004, 127( 8): 1811.
[79] ANDERSON J S, DRUZGAL T J, FROEHLICH A, et al. Decreased interhemispheric functional connectivity in autism[J]. Cereb Cortex, 2011, 21(5): 1134.
收稿日期:2021-04-28
基金名稱:北京市社会科学基金项目(19YTB011)。
第一作者简介:张亚茹(1995—),女,硕士,研究方向为田径理论与方法,E-mail:591471705@qq.com。
通信作者简介:文世林(1980—),男,博士,副教授,研究方向为身体活动促进脑健康,E-mail:313811819@qq.com。
作者单位:1.首都体育学院,北京 100191;2. 北京市健翔学校,北京 100086。
1.Capital University of Physical Education and Sports, Beijing 100191, China ; 2.Beijing Jianxiang School,Beijing 100086, China.4435031E-261A-4E37-9ED9-2ECDDCBC066B

