Predictive value of initial procalcitonin level in perioperative period of critically ill cancer patients
Yu-Lin Wu, Cui-Han Wang, Yan-Kun Zhang, Xiao-Wu Zhang, Rui Xia, Shan-Shan Lin, Bei-Tian Jia, Ya-Meng Cui*, Dong-Hao Wang*
1Tianjin Medical University Cancer Institute and Hospital, Tianjin 300060, China.2Tianjin Hospital of Integration of Traditional Chinese and Western Medicine &Nankai Hospital, Tianjin 300102, China.3Tianjin Fourth Central Hospital, Tianjin 300142, China.4Tianjin University of Traditional Chinese Medicine, Tianjin 301617, China.
Abstract
The predictive value of the initial procalcitonin (PCT) level was explored in the perioperative period of critically ill cancer patients.Background: It is quite important to predict infections in patients in the intensive care unit (ICU).Cancer surgery is characterized by large trauma, long duration, and wide operation scope; and there are many inflammatory factors in the tumor.Common manifestations of systemic inflammatory response syndrome(SIRS), such as fever, elevated white blood cells, and elevated inflammatory indicators,frequently occur in patients during the perioperative period as a result of the above factors.These factors are diverse and complex; additionally, advanced cancer and the trauma of major surgery are important factors that influence PCT blood levels.Because all of the aforementioned factors make it difficult to distinguish the postoperative inflammatory response from the true infection in clinical practice, conventional methods cannot predict disease severity or disease course.Methods: A total of 53 patients with endotracheal intubation admitted to the ICU of Tianjin Medical University Cancer Institute and Hospital from January 2020 to May 2020, were retrospectively selected.According to the patient source, 35 cases were assigned to ORIG (Operating Room to ICU Group), and 18 cases were assigned to General Ward to ICU group (GWIG).At the ICU admission, the patient’s age, sex,surgical site of tumor, reason for ICU and other data were recorded to form a database; PCT,B-type natriuretic peptide (BNP), high sensitivity troponin I (hsTni), serum creatinine (Cr),serum cystatin C (Cys-c) and other laboratory indicators were detected; scores of acute physiology and chronic health evaluation II (APACHE II) and sequential organ failure assessment (SOFA) were marked 24 h after ICU admission; Proportion of Antibiotics, Time Antibiotic Application, and Time Indicators (Ventilator support Time, Endotracheal Intubation Time, ICU Stay Time) were recorded during the period from ICU admission to ICU discharge.Results: APAHCE II score and SOFA score increased significantly in the GWIG, compared with the ORIG, and the differences were statistically significant (P <0.01); the GWIG had a significantly longer Time Antibiotic Application than the ORIG, and the difference was statistically significant (P < 0.01); in terms of blood indicators, the PCT,BNP, and hsTNi levels were elevated in the GWIG compared with the ORIG, and the differences were statistically significant (p < 0.01); no statistical differences were found in Cr and Cys-C levels (P > 0.05).In terms of time indicators, the Ventilator support Time,Endotracheal Intubation Time, and ICU Stay Time were prolonged in the GWIG compared with the ORIG, and the differences were statistically significant (P < 0.01).The PCT level was statistically significant (P < 0.01) when correlated with the Ventilator Supporting Time and Endotracheal Intubation Time; however, the PCT level was negatively correlated with the ICU Stay Time, with a small r (correlation coefficient) value and no statistical significance (P > 0.05) when correlated with the ICU Stay Time.Conclusion: The initial PCT level can predict the disease severity in critically ill cancer patients treated with mechanical ventilation during the perioperative period.
Keywords: critically ill cancer patients; perioperative period; mechanical ventilation;procalcitonin; disease severity
Background
The presence of infection and an increase in the sequential organ failure assessment (SOFA) score of 2 or more points is the latest definition of sepsis [1].Infections are mainly identified based on sensitive laboratory indicators.As we all know, predicting infection in ICU patients is critical so that doctors can make the best clinical decision possible.Delayed treatment or an incorrect diagnosis may lengthen the ICU stay or even increase the fatality rate [2].Procalcitonin (PCT) is a glycoprotein, with a low level in the normal population.However, if the body is infected with bacteria, the PCT level will be significantly elevated, so it can be used as one of the diagnostic indicators of bacterial infectious disease [3].The PCT level begins to rise at 4 h and reaches a peak 8-24 h after bacterial invasion.However, because the time at which the patient is admitted to the ICU may not be the time of initial infection, conventional methods cannot predict the disease course of patients.
Cancer has become a chronic disease, so people have a higher expectation for the prognosis of cancer.Currently, surgery is one of the primary methods for cancer patients to eliminate the threat of cancer.Furthermore, the treatment of critically ill cancer patients during the perioperative period has a direct impact on the quality and prognosis of their postoperative survival.Cancer surgery is characterized by large trauma, long duration, and wide operation scope; there are several inflammatory factors in the tumor.Affected by the above factors, common manifestations of SIRS often occur in patients during the perioperative period, such as fever, elevated white blood cells, and elevated inflammatory indicators.These factors are diverse and complex; additionally, advanced cancer and trauma from major surgery are important factors that affect PCT blood levels.In clinical practice, all of the aforementioned factors make distinguishing the postoperative inflammatory response from the true infection difficult.How to effectively decrease the non-cancer mortality among cancer patients in the perioperative period, identify the infection on time, reasonably apply the antibiotics, and improve the prognosis, are important topics in the study of critically ill cancer.
Can PCT level be used as a predictor for the disease severity in cancer patients within the perioperative period? To maximize the consistency of baseline information, cancer patients treated with mechanical ventilation in the ICU were selected as the subjects of this study.We conducted a preliminarily study on the correlation between the initial PCT level and disease severity in patients from different sources, and investigated the predictive value of the initial PCT level for disease severity in critically ill cancer patients during the perioperative period.
Methods
General data
A total of 53 critically ill cancer patients with endotracheal intubation admitted to the ICU of Tianjin Medical University Cancer Institute and Hospital from January 2020 to May 2020 were retrospectively selected.According to the patient source, 35 cases were assigned to the ORIG, and 18 cases were assigned to the General Ward to ICU group (GWIG).
Inclusion criteria: i, Patients treated with endotracheal intubation or patients with endotracheal tube unremoved after surgery and treated with mechanical ventilation; ii, Critically ill cancer patients, with old age (age ≥ 65 years), multi-system chronic diseases (such as hypertension, type 2 diabetes, coronary atherosclerotic heart disease,atrial fibrillation, cerebral infarction, and chronic kidney disease), use of chemoradiotherapy drugs, or other high-risk factors, based on the confirmed diagnosis of cancer; iii, Patients who had received surgery for cancer in the recent period (within 2 weeks).Exclusion criteria: i,Patients aged below 18 years; ii, Patients with consciousness disorders(such as coma or vegetative state) caused by brain parenchymal damage and sputum expectoration malfunction, whose ventilator may not be removed quickly; iii, Patients with a tracheotomy, or long-term retention of artificial airways; iv, Patients who experienced sudden cardiac arrest, malignant arrhythmia, acute pulmonary embolism,acute cerebrovascular accident, aortic dissection, or other acute and critical illnesses before or after ICU admission (the aforementioned conditions could affect the study results and cause serious bias, so these patients were excluded); v, Patients with mental disorders who were not cooperative.
Methods
i, At the ICU admission, all eligible patients’ age, sex, surgical site of tumor, reason for ICU, and other data were recorded to form a database; blood samples were collected within 15 min after ICU admission, the PCT, BNP, hsTni, Cr, Cys-c and other indicators were detected in the laboratory department of Tianjin Medical University Cancer Institute and Hospital; ii, Scores of APACHE II and SOFA were marked 24 h after ICU admission; iii, Proportion of Antibiotics, Time Antibiotic Application, and Time Indicators (Ventilator support Time,Endotracheal Intubation Time, ICU Stay Time) were recorded during the period from ICU admission to ICU discharge.
Statistical method
The SPSS 25.0 statistical software was used for analysis.
The measurement data that conformed to normal distribution were expressed as mean ± standard deviation and assessed using the t-test,whereas those that did not conform to normal distribution were expressed as (Q1, Q3) and assessed using the Mann-Whitney U test.The chi-squared test was used to assess count data expressed as a percentage.Correlation analysis was performed using Spearman’s correlation coefficient.Note: *P< 0.05, **P< 0.01, compared between the two groups.
Results
Subject screening
A total of 252 critically ill cancer patients were admitted to the ICU of Tianjin Medical University Cancer Institute and Hospital from January 2020 to May 2020.Of the 252 patients, 64 were screened out, while 188 were excluded because they did not require mechanical ventilation; the 64 patients were then further screened to enroll those who had received surgery for cancer treatment within the previous 2 weeks; finally, a total of 53 critically ill cancer patients treated with mechanical ventilation during the perioperative period were enrolled,and they were divided into the ORIG and GWIG based on patient source (Figure 1).

Figure 1 Flow Chart of Patient Enrollment 252 Critically ill cancer patients were admitted to the ICU of Tianjin Medical University Cancer Institute and Hospital from January 2020 to May 2020.Finally,53 Critically ill cancer patients with perioperative period were put on ventilators.
General characteristics of enrolled patients
No statistical difference was noted between the two groups of patients in age and sex (P> 0.05, Table 1).The enrolled patients had an average age of 64.25 years and were mostly elderly, with men accounting for more than 60% of the total.The mean age in the ORIG was older than in the GWIG, but there was no statistical difference; the ORIG had a lower proportion of males than the GWIG, but there was no statistical difference.
Disease severity was assessed using the APAHCE II and SOFA.From the overall level, the mean APAHCE II score was 16.02 and the mean SOFA score was 6.09, presenting the characteristics of critical illness.When comparing groups, the GWIG significantly increased its APAHCE II score and SOFA score when compared to the ORIG, and the differences were statistically significant (P< 0.01, Table 1).
When patients were transferred to ICU, their Surgical Site of Tumor and Reason for ICU were recorded.According to the statistical findings, the majority of patients were in the perioperative period of gastrointestinal surgery.Only the difference in colorectal cancer was statistically significant when comparing groups (P< 0.05, Table 1).In terms of reason for ICU, the poor physical foundation, acute respiratory failure, sepsis, and other situations were noted in 65.7%,14.3%, 8.6%, 2.9%, and 8.6% of patients, respectively, in the ORIG,and poor physical foundation was the biggest reason; the acute respiratory failure, sepsis, and other situations were noted in respectively 27.8%, 44.4%, and 27.8% of patients in the GWIG, and sepsis was the biggest reason.Compared between groups, the difference in sepsis was statistically significant (P< 0.05, Table 1).
In terms of infection, statistics of the Proportion of Antibiotics,Focus of Infection, and Time Antibiotic Application were made.From the overall level, only 17% of patients did not use antibiotics, and postoperative prevention (49.1%) was the biggest reason for antibiotic application; the other reasons for antibiotic application were Pulmonary Infection (24.5%) and Other Site Infection (9.4%); the Time Antibiotic Application was on the 7th day after surgery in 75% of patients.The GWIG had a higher proportion of patients who did not use antibiotics than the ORIG; however, the reasons for antibiotic application in the ORIG were Pulmonary Infection (44.4%), Other site Infection (27.8%), and postoperative prevention (0); furthermore, no significant difference was found between the ORIG and the GWIG in each reason for antibiotic application (P> 0.05, Table 1).However,the GWIG had a significantly longer Time Antibiotic Application than the ORIG, and the difference was statistically significant (P< 0.01,Table 1).
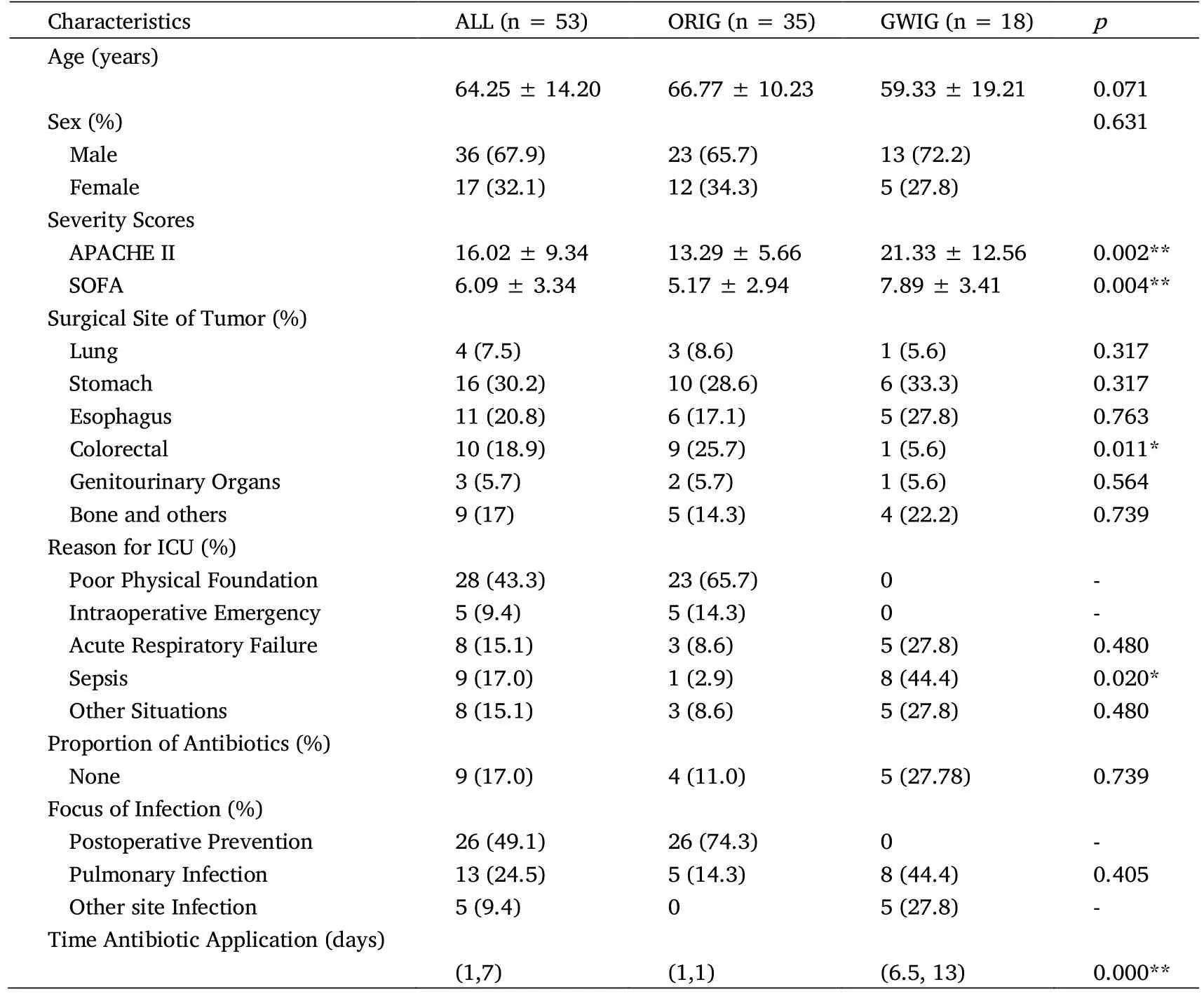
Table 1 Characteristics of Enrolled Patients In the ICU
Indicators of enrolled patients
In terms of blood indicators, PCT, BNP, and hsTNi levels were elevated in the GWIG, compared with the ORIG, and the differences were statistically significant (P< 0.01, Table 2); no statistical differences were noted in Cr and Cys-C (P> 0.05, Table 2).In terms of time indicators, the Ventilator support Time, Endotracheal Intubation Time, and ICU Stay Time were prolonged in the GWIG compared with the ORIG, and the differences were statistically significant (P< 0.01,Table 2, Figure 2).

Table 2 Indicators of Enrolled Patients In the ICU

Figure 2 Display Time Indicators with Survival Figure
Correlation between PCT and Time Indicators
Correlation between PCT and Time Indicators was analyzed and showed a positive correlation between the PCT level and the Ventilator support Time and Endotracheal Intubation Time, with a statistical significance (P< 0.01, Table 3); and a negative correlation between the PCT level and the ICU Stay Time, with a small r(correlation coefficient) value and no statistical significance (P>0.05, Table 3).

Table 3 Correlation between PCT and Time Indicators
Discussion
Infectious disease remains one of the leading causes of death in the ICU.A large epidemiological survey in China demonstrated that 1/5 of the patients admitted to ICU developed sepsis, with a mortality rate of up to 35.5% [4].Relevant research has discovered that serum PCT has high clinical values in the early diagnosis of sepsis and the assessment of disease severity [5-7].PCT is a calcitonin propeptide with no hormone activity, 116 amino acids, and a molecular mass of 13 kDa.Normally, the serum PCT level in the body is extremely low (< 0.1 ng/ml).However, after the occurrence of infections especially sepsis, a large amount of PCT is produced by many tissues and organs in the body under the action of inflammatory factors and released into the blood.At last, the serum PCT level is significantly elevated, and its elevation speed and range are positively correlated with the degree of the inflammatory response caused by the infection.As a result, PCT level can directly reflect the severity of the infection and has high specificity and sensitivity for the diagnosis of bacterial infectious diseases [8, 9].
Generally, patients treated with mechanical ventilation during the perioperative period are affected by various factors, such as infection,surgery-related factors, poor physical foundation, diaphragm elevation, and respiratory muscle paralysis, but infectious factors are the most common.According to one study, the PCT level can rise sharply in a short period due to surgery and then gradually fall back to normal within 48 h, indicating that a positive PCT result does not always indicate infection [10].These factors all work together to impede an accurate and timely diagnosis of the infection.In this study,the ORIG had a significantly lower PCT level and less Time Antibiotic Application than the GWIG, indicating that infections in the ORIG were significantly less severe than those in the GWIG.These findings suggest that in critically ill cancer patients who need ventilator support after surgery, the elevated PCT level may be associated with surgery rather than infection, so more evidence should be collected for antibiotic application.
Antibiotic resistance is growing more and more serious, with irrational use of antibiotics as the main cause.In this study, we discovered that the proportion of antibiotics used in the ORIG was higher than that used in the GWIG, with the primary reason being postoperative prevention.However, the time distribution for antibiotic application was only 1 day in both groups, and the total dose of antibiotic application in the ORIG was lower than that in the GWIG, meeting the principles for rational use of antibiotics and discontinuation as soon as possible.The Time Antibiotic Application in the GWIG, on the other hand, was much longer than in the ORIG.These findings suggest that intensive postoperative care for critically ill cancer patients may help to avoid serious emergencies, reduce antibiotic use, and have a positive effect on reducing irrational antibiotic use.Meanwhile, relevant data show that the average number of ICU beds per hospital in China is 5.8-8.7 [11, 12], which accounts for only about 1.1% of the total beds.As a result, 80 percent of sepsis patients and 40% of septic shock patients cannot be admitted to the ICU for systematic treatment [13].In this study, the majority of patients in the ORIG asked ICU doctors to help them assess the severity of their disease before surgery, and they were immediately transferred to the ICU after surgery.The results showed that patients in the ORIG had a shorter Time Antibiotic Application, Ventilator support Time, Endotracheal Intubation Time, and ICU Stay Time than patients in the GWIG.The levels of blood indicators were lowered in the ORIG compared with the GWIG.These indicate that the intensive care and life support provided to critically ill cancer patients in the ICU during the perioperative period have shortened the disease course, and improved the utilization rate of ICU beds.However, if patients are transferred to the ICU after developing severe respiratory failure or even sepsis, the disease course and ICU Stay Time will be prolonged.
In this study, we found that the initial PCT level of critically ill cancer patients treated with mechanical ventilation during the perioperative period, was positively correlated with the Ventilator support Time and Endotracheal Intubation Time.This finding suggests that the higher initial PCT level corresponds to the longer Ventilator support Time.However, no significant positive correlation was found between the ICU Stay Time and the initial PCT level in the correlation analysis.The reason for this could be that, aside from changes in respiration and infection status, patients are transferred out of the ICU for a variety of reasons, including circulation, consciousness, and nutritional status; besides, the possibility of the positive result being caused by the small sample size cannot be ruled out.
Patients in the ICU have complex and changeable conditions, long disease course, and long hospital stay time, which put more strain on ICU resources.Complications can be decreased in cancer patients through postoperative intensive care.Seemingly, the transfer to ICU after surgery has employed the ICU resources, but in essence, it prevents severe potential complications, shortens the hospital stay time, and reduces the total dose of antibiotic application, so it saves the ICU resources and even medical data.As a result, increasing the proportion of patients transferred to ICU after surgery may be an important measure to reduce non-cancer mortality among cancer patients during the perioperative period, use antibiotics more wisely,and improve prognosis.The above conclusions must still be validated by a large sample from multiple centers and regions, which will be one of the clinical trial’s focal points.
Conclusion
The initial PCT level can predict the disease severity in critically ill cancer patients treated with mechanical ventilation during the perioperative period.
 Precision Medicine Research2022年1期
Precision Medicine Research2022年1期
- Precision Medicine Research的其它文章
- Advances in Mig6 gene in tumor research
- Clinical research progress of first-line immunotherapy for extensive-stage small cell lung cancer
- Identification of nasopharyngeal carcinoma-related microRNAs based on weighted gene co-expression network analysis
- Recognition of prognostic biomarker and its association with immune infiltrates in breast cancer associated with inflammation
