Interference screws vs.suture anchors for isolated medial patellofemoral ligament femoral fixation:A systematic review
Filippo Migliorini*,Alice BronciniJ€org EschweilerMrkus TingrtNicol Mffulli
a Department of Orthopaedics,University Clinic Aachen,Rheinisch-Westf€alische Technische Hochschule(RWTH)Aachen University Clinic,Aachen 52074,Germany
b Department of Medicine,Surgery and Dentistry,University of Salerno,Baronissi 84081,Italy
c School of Pharmacy and Bioengineering,School of Medicine,Keele University,Stoke on Trent ST4 7QB,UK
d Centre for Sports and Exercise Medicine,Barts and the London School of Medicine and Dentistry,Mile End Hospital,Queen Mary University of London,London E1 4DG,UK
Abstract
Keywords: Femoral fixation;Medial patellofemoral ligament reconstruction;Patellofemoral instability
1. Introduction
Recurrent instability of the patellofemoral joint is a multifactorial disorder with higher prevalence in active and young populations.1-3 After the first dislocation, up to 96% of patients present damage to the medial patellofemoral ligament(MPFL).4MPFL reconstruction yields excellent outcomes and patient satisfaction,with a low rate of re-dislocations.5In fact,the centers performing MPFL reconstruction have doubled in the last decade.6Several studies have focused on ways to optimize the results of MPFL reconstruction. The semitendinosus tendon autograft for MPFL reconstruction has been shown to perform better than the gracilis.7A recent meta-analysis supported the use of a double bundle graft.8Concerning patellar fixation,suture anchors produced a lower rate of anterior knee pain and complications compared with the bone-tunnel technique.9To the best of our knowledge, no study concerning femoral fixation has been conducted. Several techniques have been described for femoral graft fixation, but the most common techniques are interference screws and suture anchors. Thus, we conducted a systematic review to compare interference screws and suture anchors graft fixation techniques for primary MPFL reconstruction in patients with recurrent patellofemoral instability. The present study focused on clinical scores and complications such as re-dislocation, revision, apprehension test, and persistent joint instability sensation. We hypothesized that both fixation techniques would achieve optimal fixation with a low rate of complications.
2. Methods
2.1. Search strategy
This systematic review of the literature was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses(PRISMA)guidelines.10The following PICOT algorithm guided the preliminary search:
-(P)Population:recurrent patellofemoral instability
-(I)Intervention:isolated MPFL reconstruction
-(C) Comparison: femoral fixation through interference screws vs.suture anchors
-(O)Outcomes:clinical scores,complications
-(T)Timing:mid-term follow-up
2.2. Literature search
The literature search was performed independently by 2 authors (FM and AB) in September 2020. The following databases were searched: PubMed, Embase, Google Scholar, and Scopus.The keywords used for the search were,in combination:“patellofemoral”, “ patellar”, “instability”, “recurrent”, “pain”,“syndrome”,“dislocation”,“luxation”,“subluxation”,“therapy”, “surgery”, “management”, “MPFL”, “rupture”,“tear”, “reconstruction”, “tendon”, “graft”, “femoral”,“fixation”, “sch€ottle”, “interference”, “screw”, and “anchor”.Titles and related abstracts were screened by the same 2 authors.If the topic matched, the full text of the article was accessed.The bibliographies were screened for additional articles.
2.3. Eligibility criteria
All studies reporting the outcomes of isolated MPFL reconstruction for recurrent patellofemoral instability via an autologous graft were eligible. Only articles indicating the type of femoral fixation were considered for inclusion. Missing information on end points or lack of quantitative data under the outcomes of interest warranted exclusion from the study. The minimum length of follow-up required for inclusion was 18 months. To obtain the most reliable results, studies reporting data from patients with elevated tibial tuberosity-tibial groove and/or patella alta were not included,along with those presenting trochlear dysplasia types C and D according to the Dejour classification.11Articles reporting data on first-time patellar dislocation patients were excluded.Articles with a level of evidence of I-IV,according to the Oxford Centre of Evidenced-Based Medicine,12were included.Given the authors’language capabilities, articles in English, German, Spanish, Italian, and French were included. Comments, letters, technique notes,protocols, editorials, guidelines, and registries were excluded.Computational, animal, biomechanical, and cadaveric studies were also excluded. Articles referring to patients who had received or planned to have knee arthroplasty were excluded.Articles referring to revision setting were excluded. Articles combining MPFL reconstruction with other proximal or distal alignment were excluded. Disagreements between the authors were debated and decided by a third author(NM).
2.4. Outcomes of interest
Two of the authors (FM and AB) performed the following data extraction: generalities (author, year, journal, and type of study), patient demographics (number of knees and mean patient age), follow-up duration, and surgical techniques (type, fixation, source, and bundle insertion of the graft). The following outcomes of interest were collected:Kujala Anterior Knee Pain Scale,13Lysholm Knee Scoring Scale,14Tegner Activity Scale,15and complications. Complications of interest included the positive apprehension test, persistent sensation of instability, revision, and re-dislocation. In accordance with Nikku et al.,16sensation of persistent instability was defined as recurrence and/or subjective sensation of subluxation or instability.
2.5. Methodological quality assessment
For the methodological quality assessment, the Coleman Methodology Score(CMS)was used.17The CMS is widely used to evaluate the methodological quality of systematic reviews and meta-analyses and is highly reliable.18-20 This score allows for an analysis of the included papers based on several points of interest, including study size, follow-up duration, surgical approach, type of study, description of diagnosis, surgical technique, and rehabilitation. Additional outcome criteria assessment, the procedures for assessing outcomes and the subject selection process were also evaluated. The CMS rates articles with values between 0 (poor)and 100 (excellent). Articles with values of greater than 60 are considered satisfactory.
2.6. Statistical analysis
For statistical analysis, SPSS software (Version 25.0; IBM Corp., Armonk, NY, USA) was used. The mean difference(MD)was used for continuous variables.For binary variables,the odds ratio effect measure was adopted.For binary comparisons, the confidence interval was set at 95%. The unpaired t test was performed for conitnuous variables, while the chi--quare test for binary data.Values of p<0.05 were considered statistically significant.
3. Results
3.1. Search results
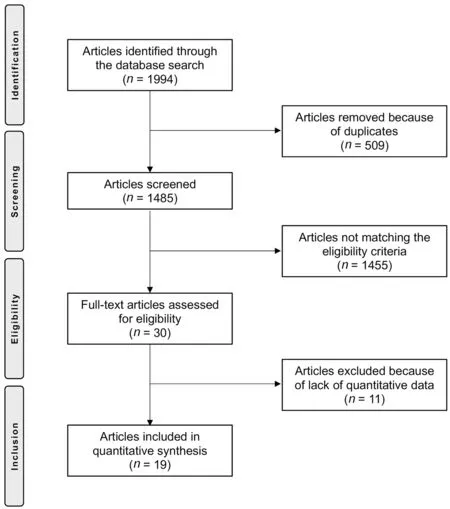
Fig.1. Flow-chart of the literature search.
The literature search resulted in 1994 articles being identified. Of these, 509 duplicates were excluded. An additional 1455 articles were excluded because of one of the following reasons: language limitation (n=36), acute onset (n=15),revision setting(n=21),presence of pathoanatomical risk factors (n=471), short follow-up term (n=114), using an allograft or xenograft or synthetic graft (n=39), type of study(n=401), patients with planned or previous knee arthroplasty(n=13), combined surgeries (n=278), uncertain results(n=11), and other reasons (n=56). Ultimately, an additional 11 articles were excluded because they lacked quantitative data under the outcomes of interest. This left 19 articles for inclusion, 5 on the use of suture anchors and 14 on the use of interference screws(Fig.1).
3.2. Methodological quality assessment
The CMS identified some limitations and points of strength in the present study. The study size and follow-up duration of the included articles were acceptable.Surgical approach,diagnosis, and rehabilitation were well-described in most articles.Outcome measures and timing of assessment were often defined, providing moderate reliability. General health measures were rarely reported. The procedures for assessing outcomes and subject selection were often biased and not satisfactorily described. The CMS for the articles was 75%,attesting to this study a good quality of the methodologies for the included articles.The CMS is reported in Table 1.
3.3. Patient demographics
Data were retrieved for 615 patients. The age was 24.4 §6.7 years(mean§SD).The mean follow-up was 46.5§20.9 months.There were 76 patients in the anchor group and 539 in the screw group. Comparability was found with regard to age and follow-up duration between the 2 study groups.The autografts used for reconstruction were semitendinosus (n=11),gracilis (n=6), quadriceps (n=2), hamstring (n=2), and patellar(n=1).A double-bundle patellar fixation was reported on in 12 cohorts,and 6 cohorts reported on a single bundle fixation. Patellar fixation was achieved via suture anchors(n=10), bone tunnel (n=5), soft tissue (n=2), Endobutton(n=1),and transosseous suture (n=1).Study generalities and patient demographics baseline are shown in Table 2.
3.4. Outcomes of interest
There was comparability between the 2 groups for the scores at baseline. At last follow-up, the mean Kujala score was greater in the screw group(+2.1%;p=0.04),while no difference was found with regard to the Lysholm (+1.7%;p=0.05) and Tegner (+15.8%; p=0.05) scores. These results are shown in detail in Table 3.
Although complications occurred almost exclusively in the screw cohort, no statistically significant difference between the 2 groups was found. The complications related to each technique are shown in detail in Table 4.
4. Discussion
The present systematic review evaluated femoral fixation techniques for autograft for isolated MPFL reconstruction in patients with recurrent patellofemoral instability at mid- to long-term follow-up.The main findings in our study indicated that femoral fixation through interference screws produced clinical scores similar to those produced by suture anchors.No differences were found for rates of positive apprehension tests,persistent joint instability,re-dislocation,or revision.
The MPFL is the most important dynamic restraint to patellar lateralization during the first 30˚of flexion.21,22Several studies have investigated efforts to improve reconstruction techniques,but to the best of our knowledge the effects of femoral fixation (interference screw vs. suture anchors) have notyet been investigated.Our study offers new insights regarding the issue of femoral fixation,evidencing remarkable similarity between interference screws and suture anchors.We acknowledge that our study has several limitations,which were mainly due to the lack of studies in the literature.
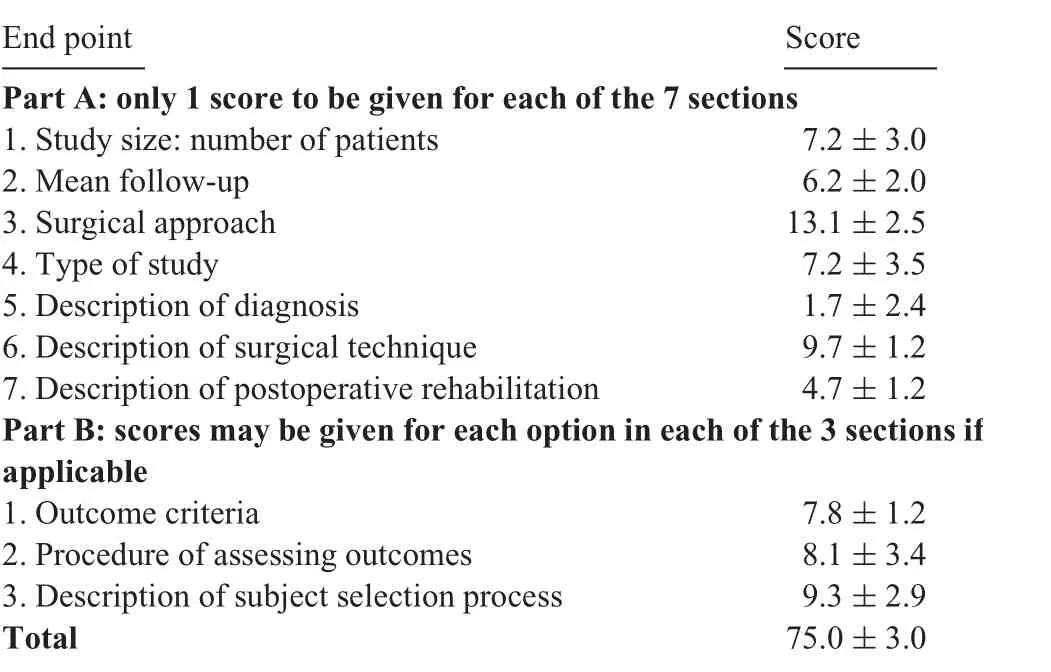
Table 1 Coleman Methodology Scores for the included articles(mean§SD).
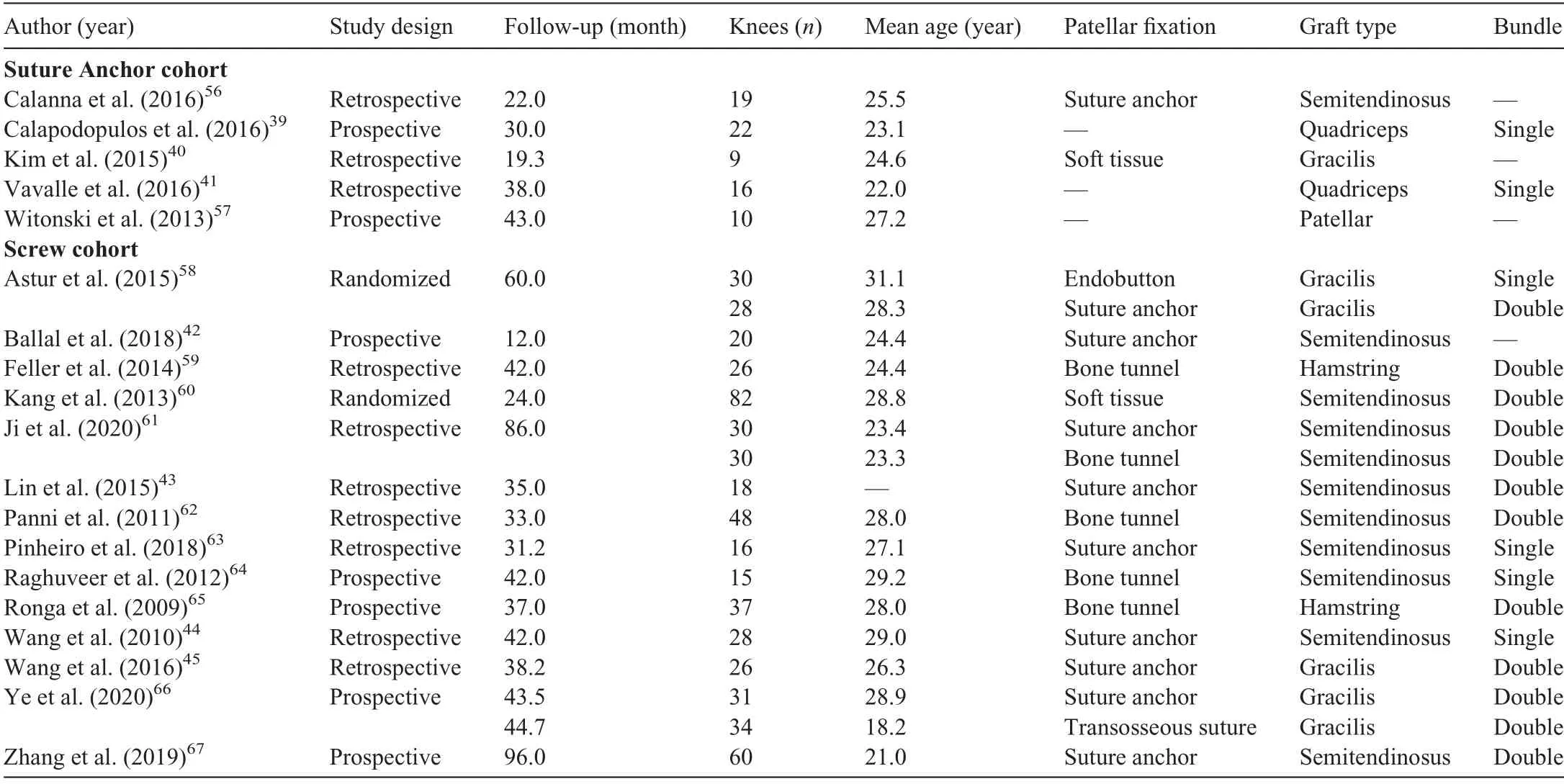
Table 2 Study generalities and patient demographics baseline.
In the present study,complications(even though not statistically significant) occurred almost exclusively in the interference screw cohort. Fixation through interference screws increased local pressure around the tendon-cancellous bone interface, which should provide quicker healing.23Bone mineral density,material properties,core diameter,pitch or thread height, geometry, placement, length, insertion torque, and gap size influenced the fixation.24-26 Several mechanisms of failure for interference screws have been described:graft pullout,26slippage and laceration by the screw threads,25and/or fatigue fracture during screw insertion.27The use of suture anchors has spread rapidly in the past few years.Anchors may have become less expensive and now have a lower risk of overtightening. Furthermore, their use does not affect thegrowth plates, which offers an attractive alternative in skeletally immature patients. These features make suture anchors favorable. However, anchors do not provide better surgical outcomes than interference screws. In the studies included in our review, different types of interference screws and suture anchors were used, thus leading to biased results. On the other hand, the literature presents a large variability in instrumentation;thus,it was not feasible to directly compare 2 specific implants in our systematic review.
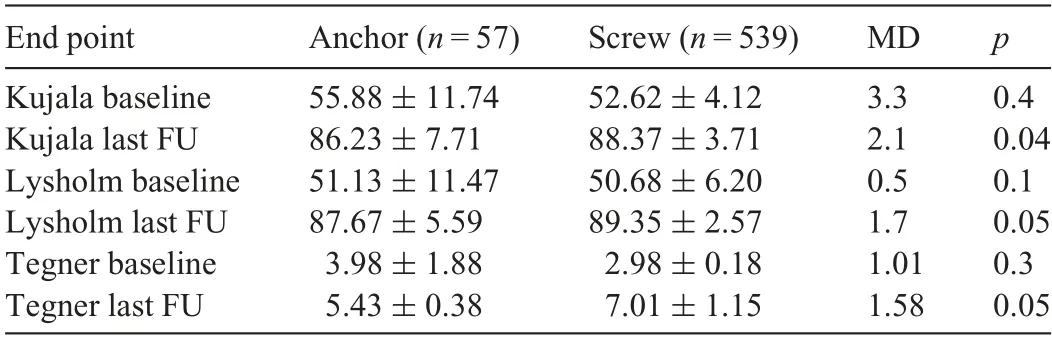
Table 3 Analyses of scores(mean§SD).
Improper femoral fixation leads to a high risk of failure.28In a cadaveric study, the femoral insertion of the MPFL was reported to have been approximately 1 cm wide,with an oblique decussation originating from the superficial medial collateral ligament.29The femoral origin of the MPFL is located between the adductor tubercle and the medial epicondyle, but it is closer to the adductor tubercle, just 2 mm anterior and 4 mm distal to this prominence.30The optimal landmarks for graft insertion have been described by Sch€ottle et al.31The first anatomical reference is represented by the tangent to theposterior femoral cortex. Two lines perpendicular to the first line are drawn:one at the posterior aspect of the Blumensaat’s line32and one at the transition of the posterior femoral condyle curves. The Sch€ottle point is 2 mm anterior to the posterior cortical line between these 2 perpendicular lines. To find this point, it is essential to obtain a perfect lateral of the distal femur.Indeed,minimal position variations also lead to nonanatomic femoral graft fixation. A fixation that is too proximal increases graft tension during flexion,thus enhancing the contact pressure between the medial patellar and trochlear facet joints, whereas a fixation that is too distal reduces graft tension,causing lateralization of that patella and maltracking.
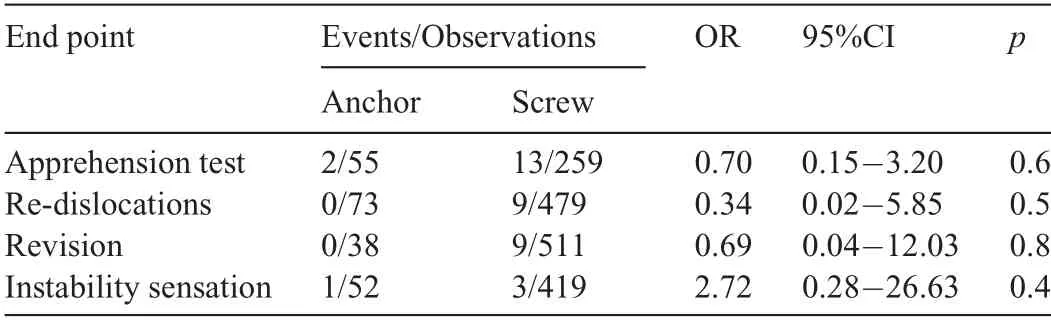
Table 4 Analyses of complications.
Skeletally immature patients require special consideration.The literature presents conflicting evidence about the relationship between the femoral insertion of the MPFL and the distal femoral physis. MPFL reconstruction is considered to be the optimal treatment for skeletally immature patients;33,34however, given the adjacent physis, the treatment requires additional considerations because it is controversial whether the Sch€ottle point should be placed proximally or distally to the physis. Following the criteria described by Sch€ottle et al.,31Shea et al.35found that the optimal placement was approximately 2-5 mm proximal to the physis. However, other evidence supports its location distally to the physis.36These data have been also confirmed by further magnetic resonance37,38and cadaveric studies.29,30
Our investigation included 7 studies39-45 that involved trochlear dysplasia types A and B according to the Dejour classification.11MPFL reconstruction alone cannot compensate for severe trochlear dysplasia because bony surgery aiming to restore the physiological morphology would be indicated in these patients.46,47The exclusion of patients with severe trochlear dysplasia may represent a limitation to our study.However, several studies investigated the use of isolated MPFL reconstruction in patients with mild dysplastic abnormalities and reported excellent results.48-51 For this reason(and because of the lack of studies on patients who had no pathoanatomical risk factors),we included them in our review.The underlying morphology of bony and soft tissues is responsible for instability, and most of the patients in the studies we included presented 2 or more pathoanatomical risk factors that predisposed them to dislocation.52-54 However, in the presence of mild to moderate pathoanatomical risk factors,isolated MPFL reconstruction with a thicker graft may compensate for the tendency to lateralization,providing good patellar tracking and avoiding more invasive procedures.
In addition to the above limitation, our study has a few others.First,half of the included studies were retrospective in nature, and many lacked randomization. This leads to a high risk of selection bias and uncertain results. None of the included studies used any blinding methods, thus increasing the risk of detection bias. Given the paucity of studies in the literature reporting data on anchor fixation,we included only 5 such studies in our analysis. However, we believe that even with an increase in the number of anchor fixation procedures,the rate of complications experienced in the use of the 2 techniques would remain comparable. The lack of the evaluation of predisposing risk factors among the participants is another important limitation. An analysis of surgical outcomes of MPFL reconstruction based on pathoanatomical bony morphology would achieve more reliable results and should be addressed in future studies. Moreover, our study did not compare or evaluate the length of stay in the hospital,the duration of the surgery,or the cost effectiveness of the procedure.Similarly, there were end points that may have been relevant but were not analyzed,such as the infection rate.55There are several other techniques for achieving MPFL graft femoral fixation, including bone plugs, Endobuttons staples, and soft tissues fixation on the tendon of the adductor magnus.Furthermore, we did not evaluate the position of the femoral attachment, which affects patellar stability and functional results of MPFL reconstruction. Another potential limitation that may have influenced the outcomes was the differing patellar fixation techniques, autografts, and bundles used in MPFL reconstruction.Given the lack of data on these issues,we were not able to address them in our study. Other important limitations involve the heterogeneous type of graft used for reconstruction (quadriceps, patellar, hamstring, semitendinosus, or gracilis), the type of graft insertion (double or single bundle),and the type of patellar fixation used (tunneling techniques,Endobutton, or soft tissue procedures). Some of the included studies investigated the use of a lateral retinacular release in the event of high lateral patellar pression.Despite the absence of any clearly stated guidelines, this technique is often performed in combination with MPFL reconstruction. Future studies should investigate its effect on patellofemoral biomechanics, as well as its surgical indication. Some studies were included despite the fact that participants had had previous knee surgeries.This may have negatively affected the surgical outcomes and led to heterogeneity.However,given the lack of data on these outcomes, further subgroup analyses were not possible. Given these limitations, the results from our study should be interpreted with caution, and the limitations should addressed in future investigations.
Important strengths of our work include the strict eligibility criteria we used and the comprehensive nature of our literature search. The use of isolated MPFL reconstruction in patients presenting elevated tibial tuberosity-tibial groove,patella alta,and severe dysplasia is controversial, and the debate about its value continues. Therefore, studies including patients with pathoanatomical risk factors that predispose them to instability were not included in our analysis.
5. Conclusion
Femoral autograft fixation using interference screws or suture anchors reported similar clinical scores and rate of positive apprehension test, persistent joint instability, re-dislocations, and revisions. The results of our review must be interpreted with its limitations in mind.
Authors’contributions
FM performed the literature search,data extraction,statistical analyses, and writing; AB performed the literature search and data extraction; JE made revisions; MT supervised; NM made the final revisions and final approval. All authors have read and approved the final version of the manuscript,and agree with the order of presentation of the authors.
Competing interests
The authors declare that they have no conflicts of interest.
 Journal of Sport and Health Science2022年1期
Journal of Sport and Health Science2022年1期
- Journal of Sport and Health Science的其它文章
- Does eccentric exercise stimulate sarcomerogenesis?
- The Beijing 2022 Winter Olympics:An opportunity to promote physical activity and winter sports in Chinese youth
- Beijing 2022 Winter Olympic Games:Commitments to science and public health
- Corticospinal activity during a single-leg stance in people with chronic ankle instability
- Knee biomechanics of patients with total knee replacement during downhill walking on different slopes
- Biceps femoris long head sarcomere and fascicle length adaptations after 3 weeks of eccentric exercise training
