Simultaneous endoscopic and video-assisted retroperitoneal debridement in walled-off pancreatic necrosis using a laparoscopic access platform: Two case reports
Lars Lindgaard,Morten Laksafoss Lauritsen, Srdan Novovic,Erik Feldager Hansen, John Gasdal Karstensen,Palle Nordblad Schmidt
Abstract
Key Words: Acute necrotizing pancreatitis; Walled-off necroses; Minimally invasive surgical procedures; Multiple organ failure; Natural orifice transluminal endoscopy;Sepsis; Case report
INTRODUCTION
Infected walled-off necrosis (WON) is a potentially life-threatening complication of necrotizing pancreatitis. Traditionally, such patients were treatedviaopen surgery, but during the last decade an endoscopic or surgical step-up approach using minimally invasive techniques has become the treatment of choice[1 -5 ].
Whereas some patients can be treated by drainage alone, many patients also need evacuation of the infected debris. In such cases, it is our experience that central necroses in relation to the pancreatic bed are most easily reached by endoscopic,transluminal drainage followed by endoscopic necrosectomy (EN), whereas necroses that involve the paracolic gutters and the pelvis are more effectively treated with percutaneous drainage and video-assisted retroperitoneal debridement (VARD).
We report on two patients who needed a combination of endoscopic and percutaneous drainage and necrosectomy for their large, infected WONs.Furthermore, we introduce a laparoscopic access platform (Figures 1 and 2 ) as a useful adjunctive to EN and VARD.
CASE PRESENTATION
Chief complaints
Case 1: A 36 -year-old male with a history of proctocolectomy and J-pouch due to ulcerative colitis was admitted to a local hospital because of jaundice.
Case 2: An 18 -year-old boy was admitted to another hospital with severe necrotizing pancreatitis of unknown etiology.
History of present illness
Case 1:Magnetic resonance imaging raised suspicion of a cholangiocarcinoma in the liver hilum, a diagnosis that was subsequently confirmed. An endoscopic retrograde cholangiopancreatography revealed multiple intra- and extrahepatic bile duct strictures consistent with primary sclerosing cholangitis but failed to relieve the obstruction. Subsequent percutaneous transhepatic biliary drainage was carried out.After the endoscopic retrograde cholangiopancreatography, the patient developed post-endoscopic retrograde cholangiopancreatography pancreatitis, severe sepsis, and multiple organ failure and was admitted to the intensive care unit (ICU).

Figure 1 GelPOINT path transanal access platform.

Figure 2 Endoscopic-laparoscopic retroperitoneal debridement. A: GelPOINT path transanal access platform with access channel placed in the videoassisted retroperitoneal debridement incision; B and C: Necrotic debris evacuated through the access channel during endoscopic, transluminal necrosectomy; D:Corrugated drainage sheet placed in the video-assisted retroperitoneal debridement incision at the end of the procedure.
Case 2: On day 2 , he was referred to the ICU with respiratory and circulatory failure.On day 3 , he developed intra-abdominal hypertension and renal failure with the need for dialysis.
FINAL DIAGNOSIS
Case 1: After 6 wk, which included severe episodes of gastrointestinal bleeding that needed coiling and laparotomy with creation of an ileostomy, he was referred to our hospital for endoscopic drainage of a large (12 cm × 14 cm × 38 cm), infected, left-sided WON extending from the spleen down through the left paracolic gutter into the left groin (Figure 3 A).
Case 2: On day 43 , he was referred to the ICU at our hospital with septicemia and a large (16 cm × 24 cm × 32 cm), infected, left-sided WON extending from the pancreatic bed into the pelvis (Figure 4 A).
TREATMENT
Case 1: Between days 57 and 143 , the patient underwent one endoscopic transluminal drainage, four EN, two VARD, and seven combined EN/VARD procedures.
Case 2:The same day, VARD was performed. Five days later, after only one VARD and one EN session, he was discharged from the ICU. The patient underwent a total of one endoscopic transluminal drainage, four VARD, two EN and two combined VARD/EN procedures, with the last procedure occurring on day 77 .
OUTCOME AND FOLLOW-UP
Case 1: There was complete regression of the large WON (Figure 3 B).
Case 2: There was complete regression of the large WON (Figure 4 B).
DISCUSSION
In this paper, we describe 2 patients with necrotizing pancreatitis who needed treatment with a combination of EN and VARD. Both patients were referred to our hospital with signs of sepsis due to very large, infected WONs. We chose to combine two minimally invasive techniques to control the infection as quickly as possible in order to accelerate the treatment course.
EN is ideal for treating central WONs, whereas VARD is especially suitable in the case of lateral collections extending into the paracolic gutters and the pelvis. Even though flexible endoscopes can reach remote parts of the retroperitoneum, an isolated endoscopic approach can prove more time-consuming and delay evacuation of large collections as compared to a combined approach. Furthermore, large fluid collections may become compartmentalized over the course of treatment, creating isolated portions of the WON that can no longer be reachedviathe transluminal route. A successful combination of EN and VARD has been described elsewhere[6 ,7 ].
VARD has been thoroughly described in the literature[8 ,9 ]. However, use of a laparoscopic platform has not to our knowledge been documented. With the GelSeal cap closed and CO2insufflation through the platform, the large cavity could be expanded during the procedure, thus making debridement easier. During transgastric necrosectomy, debris was removed through the access channel of the platform by the surgeon or endoscopy assistants, reducing the procedure time. Finally, the platform facilitated debridementviathe percutaneous route using the flexible endoscope. The success of the method needs to be investigated in prospective studies evaluating the risk of recurrence and fistula formation as well as matters relating to costs of the technique.
CONCLUSION
We conclude that simultaneous transluminal and percutaneous necrosectomy is practical and hypothesize that it may accelerate treatment in cases of complex WONs due to acute pancreatitis. Furthermore, a laparoscopic access platform is a useful adjunctive to the procedure.

Figure 3 Case 1 . Coronal computed tomography with walled-off necrosis. A: Before drainage; B: After 86 d and 14 procedures.
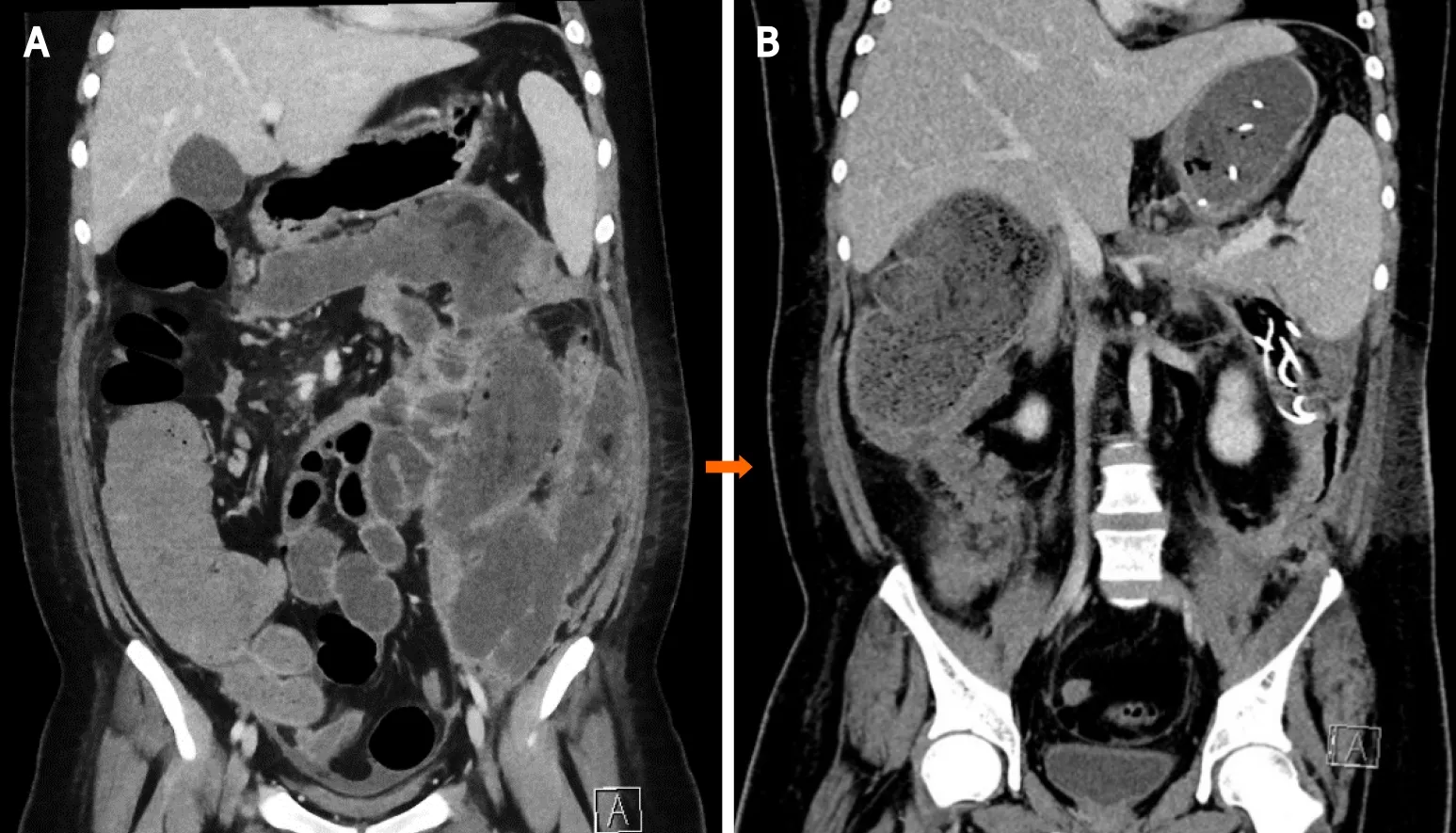
Figure 4 Case 2 . Coronal computed tomography with walled-off necrosis. A: Before drainage; B: After 34 d and nine procedures.
 World Journal of Gastroenterology2022年5期
World Journal of Gastroenterology2022年5期
- World Journal of Gastroenterology的其它文章
- Curative resection with endoscopic submucosal dissection of early gastric cancer in Helicobacter pylorinegative Ménétrier’s disease: A case report
- Viral hepatitis: Innovations and expectations
- Effect of Bacillus subtilis, Enterococcus faecium, and Enterococcus faecalis supernatants on serotonin transporter expression in cells and tissues
- Connective tissue growth factor expression hints at aggressive nature of colorectal cancer
- Abnormal liver chemistries as a predictor of COVID-19 severity and clinical outcomes in hospitalized patients
- Colorectal cancer screening and surveillance in patients with inflammatory bowel disease in 2021
