Clinical characteristics and outcomes of primary intracranial alveolar soft-part sarcoma: A case report
INTRODUCTION
Alveolar soft part sarcoma (ASPS) accounts for less than 1% of soft-tissue sarcoma[1]. Christopherson[2] first described ASPS as a unique variant from general softtissue sarcoma in 1952. ASPSs are characterized by pseudoalveolar architecture and various cytoplasmic inclusion bodies with diastase-resistant periodic acid-Schiff crystalline[3].-(or-), a fusion gene, has been shown to contribute to tumor genesis and be particularly informative in diagnosing ASPS[4,5]. While the exact cell (myogenic or neurogenic) origin of ASPS is disputable, the sarcoma entity is mainly found in the lower extremities and, to a lesser extent, in the upper extremity or trunk, head and neck, and abdomen[6]. ASPSs tend to metastasize, and brain is one of the most common targets[7,8]. Accordingly, intracranial ASPS presents as primary and metastatic ASPS, with the former being less common. The current understanding of primary intracranial ASPS (PIASPS) was based on 8 case reports (9 cases)[3,9-15]. In this study, we firstly reported 5 consecutive cases from our institute to delineate the clinical characteristics of this disease. Then, the cases from previous studies were pooled to evaluate the efficacy of treatment options in patients' outcomes with PIASPS.
CASE PRESENTATION
Chief complaints
There were 5 patients with PIASPS between 2005 and 2019, including 2 males and 3 females (Table 1). The median age of the 5 cases was 21 years (range: 8-54-years-old). One patient was asymptomatic, and the intracranial lesion was found because of routine computed tomography (CT) for a minor cranial injury. The other 4 patients suffered from various symptoms, including headache in 3 cases, aphasia, muscle weakness, each in 1 case.

History of present illness
For the 4 symptomatic patients, the median duration from the onset of symptoms to the diagnosis was 7.5 mo (range: 2-24 mo). Worsened headache (2/3) and muscle weakness (1/1) were reported after the onset of symptoms.
History of past illness
One patient had an injury in the spinal column in his childhood, which was well treated by surgery. No medical history was reported for the other 4 patients.
Physical examination
Critical and general signs were within the normal range for 5 patients. The neurological examination showed that papilledema was found in 2 patients, diplopia in 1 patient, and myasthenia of the upper right limb in 1 patient.
Laboratory examinations
Routine blood and urine tests of the 5 patients were normal.
Imaging examinations
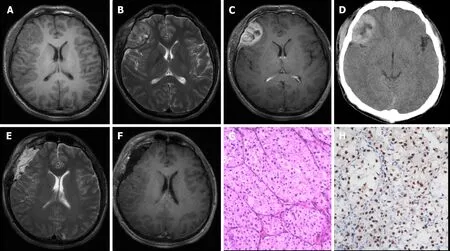
Pre-operative chest X-ray scans were normal in all patients. CT and/or magnetic resonance imaging were performed in all patients. The majority of lesions (4/5) presented as isointense/hypointense on T1 images, isointense/hyperintense on T2 images, and heterogeneous enhancement after the administration of gadolinium, with a heterogeneously high-density appearance on CT scan (Figure 1A-D). The median tumor size was 3.0 cm (range: 2.8-5.0 cm). Anterior skull-base ASPS was found in 1 case; the other 4 ASPSs were frontal, parietal, parieto-occipital, and temporal.
MULTIDISCIPLINARY EXPERT CONSULTATION
Multidisciplinary expert consultations were recorded for all patients, and one of them (the 10case in Table 1) was presented in this part.
Jia Wang, MD, Professor and Chief Doctor of Radiologist, Department of Radiology,General Hospital of the Yangtze River Shipping
The radiological appearance of this patient was not typical. Meningioma could be one potential diagnosis.
Jun-Yu Chen, MD, Attending Doctor of Neurosurgeon, Department of Neurosurgery,General Hospital of the Yangtze River Shipping
Based on symptoms, signs, physical examinations, and radiological scans, a presumed diagnosis was right frontal meningioma. Surgical treatment should be planned to remove the brain tumor and obtain a pathological diagnosis.
None of these patients was treated outside regarding the intracranial lesion. All of these patients accepted surgical treatments. In addition to routine hematoxylin and eosin staining (Figure 1G), immunohistochemical examination for TFE-3 was also employed (Figure 1H). Before establishing the diagnosis of PIASPS, extensive screenings were performed to exclude potential extracranial lesions, which included but were not limited to CT chest, abdomen and pelvis, and positron emission tomography.
Fei Hu, MD, Professor and Chief Doctor of Neurosurgeon, Department of Neurosurgery, General Hospital of the Yangtze River Shipping
Craniotomy should be performedthe right frontal approach.
Asmund, who was extremely fond of his sister, readily consented, and they had a very happy time together, carrying over all their pet treasures, and Signy s jewels and other ornaments, and arranging them in the pretty little rooms inside the trees
Jing Lv, MD, Professor and Chief Doctor of Pathologist, Department of Pathology,General Hospital of the Yangtze River Shipping
ASPS is a rare tumor with a slow high metastatic rate. Prior research has shown that GPNMB (glycoprotein nmb), a transcriptional target of ASPSCR1-TFE3, might exert a critical role during its systemic metastasis[16]. The brain is one of the most vulnerable sites of metastases[7]. Accounting for the terminal event and primary reason for death among patients with ASPS[8,12], brain metastasis reportedly features an incidence of 11%-21%[1,6,17,18]. However, the incidence of PIASPS is less common. In addition to the 5 cases treated at our institute, only 9 cases with PIASPA were reported[3,9-15]. Our findings based on pooled cases revealed that PIASPS affected young adults with female predominance; GTR (PFS) and the use of radiotherapy (OS) contributed to better prognoses.
Fang-Cheng Zhang, Department of Neurosurgery, Wuhan Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, Hubei,China
A year had passed quickly and her friend came with an envelope, containing an invitation card for the guy s wedding. The girl was completely shattered10. When she opened the letter, she saw her name in it instead.
FINAL DIAGNOSIS
Night had fallen over the North African desert, and our battalions1() tanks were huddled2(,) in a protective circle. A group of my fellow soldiers stood around a radio. As I approached, one of them put his finger to his lips.
Positron emission tomography or combinations of x-ray chest film, abdominal ultrasound scan, and/or CT should be performed to evaluate extracranial lesions. The diagnosis of PIASPS was only made when there was no evidence of extracranial ASPS.
TREATMENT
The old man seized her hands eagerly, but no time was given him to ask any questions, for the maiden drew him into the house, and set food before him, and waited on him herself
Postoperatively, gross total resection (GTR) and NGTR were achieved in 3 and 2 patients, respectively. Among the patients who received GTR, 1 patient received no adjuvant therapies and another 2 patients accepted local radiation therapy because of a high Ki-67 index (> 10%). Both NGTR patients received radiotherapy. Consequently, 4 patients received adjuvant radiotherapy postoperatively. The radiation doses available in three patients were 42 Grays, 46 Grays, and 52 Grays. Only 1 patient received chemotherapy (doxorubicin and ifosfamide), which followed NGTR plus radiotherapy.
OUTCOME AND FOLLOW-UP
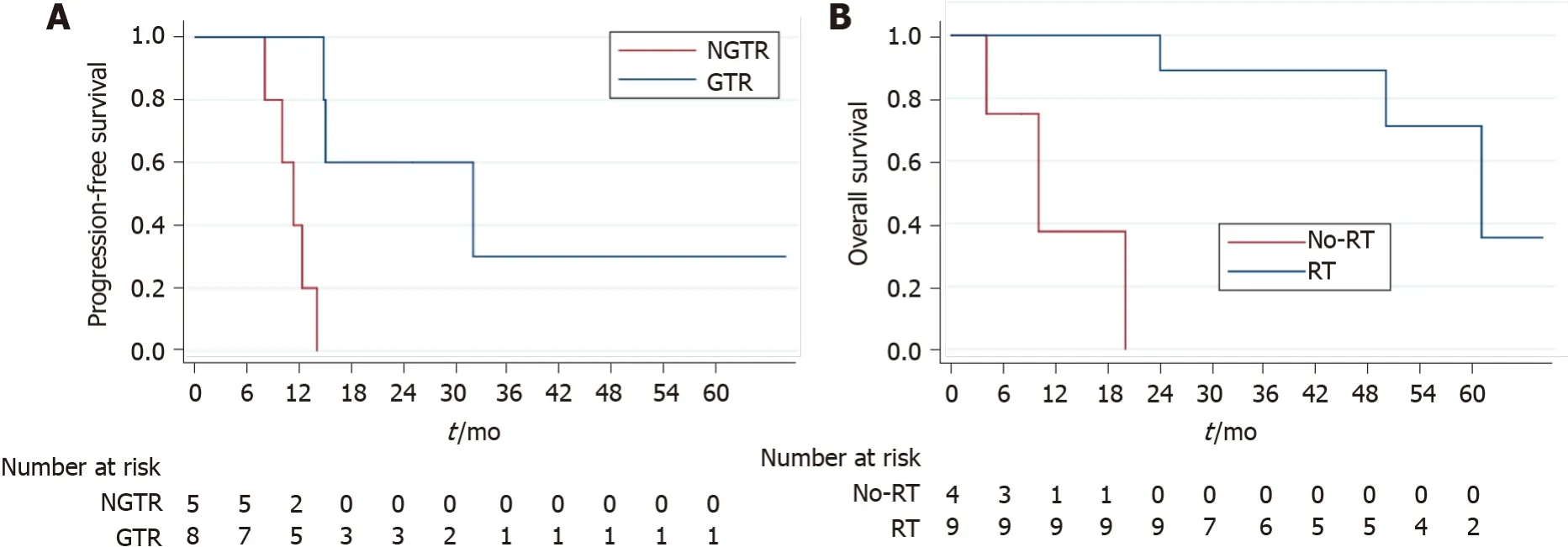
Surgical resection remains the mainstay of the treatment for IASPS[19-21]. Indeed, we found that GTR subgroup achieved a higher 3-year PFS rate when compared with the NGTR in this study. Meanwhile, there was a report[22] stating that surgery was not only associated with improved survival but also with better neurological outcomes. All accessible lesions should be completely removed to achieve better outcomes[19], and staged surgeries have been performed to accomplish this goal[21]. However, statistical analyses failed to prove that GTR could improve the OS in this study, which could be attributed to the relatively small cohort size.
DISCUSSION
An extensive search using the medical subject heading term "alveolar soft-part sarcoma" was conducted in OVID MEDLINE, EMBASE, Cochrane Database, and PubMed. Published cases were included as long as candidates were pathologically diagnosed with PIASPS and reported in the English literature. Cases with the concurrent presence of IASPS and other malignant tumors were excluded. Chen JY and Zhang FC scrutinized the resources of each patient to rule out duplicate cases. The clinical data of interest included the following: Age at diagnosis, sex, tumor location, the extent of surgery, radiotherapy, chemotherapy, progression-free survival (PFS), and overall survival (OS). Statistical analyses of the role of treatment options in prognoses (PFS and OS) were assessed by the Log-rank test using STATA 15.0 (Stata Corp, Lakeway Drive College Station, TX, United States). When-value < 0.05, the difference is considered significant statistically.
To investigate this disease comprehensively, the cases from our center and previous studies were pooled to conduct survival analyses. In brief, the female predominance was confirmed, as the integrated data (= 14) 5 males and 9 females (Table 1). The median age of 14 patients was 19 years, ranging from 8 to 53 years. One patient's follow-up detail was not reported[11]; the other 13 patients were available regarding follow-up data, with a median follow-up being 36 mo (range: 4-68 mo). Tumor progression was found in 8 (61.5%) cases and death due to disease was observed in 4 (30.4%) cases. The 3-year PFS and OS were 15.5% and 67.1%, respectively. According to log-rank tests, GTR (3-year PFS of GTRNGTR was 36.0%0;= 0.011) (Figure 2A) could prolong PFS but not the use of radiotherapy (= 0.128) or chemotherapy (= 0.090). Only radiotherapy (3-year OS of radiotherapyno radiotherapy was 87.5%0;< 0.001) (Figure 2B) resulted in longer OS, and neither GTR (= 0.071) nor chemotherapy (= 0.064) did.
Under the microscope, the specimens from hematoxylin-eosin staining showed a characteristic appearance of nests of cells loosely arranged along fibrous septa. Immunohistochemistry staining revealed tumor cells were positive for TEF-3. Pathological findings were consistent with the diagnosis of ASPS.
After a median follow-up of 36 mo (range: 25-61 mo), 1 patient remained tumor-free, but tumor progression was noticed in 4 patients. Local recurrence (LR) was observed in 3 patients, and the durations for LR were 8 mo, 10 mo, and 15 mo. All three patients with LR received surgical treatment, with one receiving radiotherapy and chemotherapy after surgery. Another patient suffered from leptomeningeal metastases, and the patient declined further treatments. When this study ended, 3 patients died of the disease (20 mo, 50 mo, and 61 mo after surgery).
After a pathological diagnosis was established, further diagnostic work-up was conducted when necessary. The final diagnoses of the 5 patients were PIASPS.
ASPS reportedly responded to radiotherapy, and several authors insisted that on the postoperative administration of radiotherapy to patients with insufficient surgical margins or even as a routine schedule[9,12,15]. Interestingly, when GTR was achieved, some centers still recommended adjuvant radiotherapy[13,15], while other centers did not[3,11,14]. Based on our experience, those patients with a high Ki-67 index or incomplete tumor resection were suitable for radiotherapy. While it was seemingly impossible to evaluate the role of radiotherapy in PIASPS based on previous case reports, pooling cases together indicated that radiotherapy could significantly improve OS. Only 6 cases reported radiation doses in the pooled cohort, which precluded further evaluation of increasing radiation doses' efficacy and safety in treating PFS. Unfortunately, our analyses failed to demonstrate that radiotherapy enabled significantly to prolong PFS. Future studies on optimal radiation modalities, radiation doses, and the optimal radiotherapy administration time are warranted to improve the efficacy of radiotherapy.
Anthracycline- or ifosfamide-based regimens, which were considered effective in treating other soft tissue sarcomas, lacked efficacy in resolving ASPS[7]. Only 3 patients were administrated with chemotherapy in the pooled cohort (Table 1)[10,13]. Consequently, our results failed to find evidence for the efficacy of chemotherapy, in prolonging either PFS or OS. Novel agents, including vascular endothelial growth factor-predominant tyrosine kinase inhibitors (, pazopanib[5]) and the mesenchymal epithelial transition factor receptor[1] (a protein encoded by the ASPSCR1-TFE3 fusion gene), seem to provide more therapeutic options to patients with ASPS. Emerging data showed that ASPS patients benefited from immune checkpoint inhibitors[23,24]. Recently, Su[25] reported an advanced lung ASPS with multiple metastases, including brain. With combined tyrosine kinase inhibitor and immune checkpoint inhibitor therapy, partial remission in brain metastases was achieved. Benefits from these novel treatments based on limited cases addressed the necessities to verify the response of ASPS in large-scale clinical trials. Therefore, in clinical practice, PIASPS patients should be encouraged to be involved in clinical trials, just similar to primary glioblastoma[26].
She cast one more lingering, half-fainting glance at the prince, and then threw herself from the ship into the sea, and thought her body was dissolving into foam
The results based on the pooled data should be carefully interpreted, as they were from various centers and distributed among the past 3 decades. However, we tried our best to minimize the bias by retrieving the objective parameters. Finally, this study, to the best of our knowledge, firstly assessed the PFS and OS of patients with PIASPS and the role of treatment options in improving patients' prognoses with PIASPS.
She then went to look into her mouse-trap, where she found six mice,33 all alive, and ordered Cinderella to lift up a little the trapdoor, when, giving each mouse, as it went out, a little tap with her wand, the mouse was that moment turned into a fine horse, which altogether made a very fine set of six horses of a beautiful mouse-colored dapple-gray. Being at a loss for a coachman, the godmother could not think of what to use.
CONCLUSION
PIASPS is a rare malignancy and predominately affects young females. Patients with PIASPS suffer from poor outcomes, characterized by a high tendency of recurrence. Surgical treatment is the first choice, and GTR should be achieved when the tumor is feasible. Patients with PIASPS benefit from radiotherapy, which should be considered as a part of treatment therapies. Future studies are needed to investigate effective radiation modalities and novel agents.
But alas37! the world of the air seemed as empty of her as the world below, and Souci was beginning to despair, and to think that he must go and search the world that lay in the sea
ACKNOWLEDGEMENTS
We appreciated Prof. Jia Wang (Department of Neurosurgery, General Hospital of the Yangtze River Shipping) and Jing Lv (Department of Pathology, General Hospital of the Yangtze River Shipping) for their contributions in multidisciplinary expert consultation.
World Journal of Clinical Cases2022年1期
- World Journal of Clinical Cases的其它文章
- Hepatitis B virus reactivation in rheumatoid arthritis
- Paradoxical role of interleukin-33/suppressor of tumorigenicity 2 in colorectal carcinogenesis: Progress and therapeutic potential
- Changes in rheumatoid arthritis under ultrasound before and after sinomenine injection
- Benefits of multidisciplinary collaborative care team-based nursing services in treating pressure injury wounds in cerebral infarction patients
- Outcomes and complications of open, laparoscopic, and hybrid giant ventral hernia repair
- Surgical resection of intradural extramedullary tumors in the atlantoaxial spine via a posterior approach
