HER2 changes to positive after neoadjuvant chemotherapy in breast cancer: A case report and literature review
INTRODUCTION
As the most common cancer in women, breast cancer is the leading cause of death. Most patients are initially diagnosed as stage I-III. Among those without distant metastases, 64% are local tumors and 27% are regional tumors[1]. Patients in stage IIAIIIC and those who meet the breast-conserving criterion with the exception of tumor size can consider neoadjuvant chemotherapy (NACT).
At last, an old car drove up in front of the vet s. Two kids raced to the door. They scooped2 Minnie into their arms and rushed her out to their grandfather, who was waiting in the car. I hurried behind them to see his reaction to Minnie.
It is worth noting that the status of tumor cell biomarkers is not consistently static. Endocrine-related estrogen receptor (ER), progesterone receptor (PR) and human epidermal growth factor receptor 2 (HER2) encoded by erythroblastic leukemia viral oncogene homolog 2 gene can all alter from positive to negative or, especially in luminal B subtype after NACT[2]. In addition, determination of HER2 status currently mainly relies on immunohistochemistry (IHC) and fluorescencehybridization (FISH), but FISH is commonly used when the result of IHC is uncertain. HER2 is regarded as negative when the IHC result is 0/1+ without the addition of FISH. To the best of our knowledge, this is the first report of a case harboring HER2 status transformation and IHC1+ with positive amplification by FISH after NACT.
CASE PRESENTATION
Chief complaints
A mass was discovered in the right breast of a 49-year-old woman during a routine examination.
History of present illness
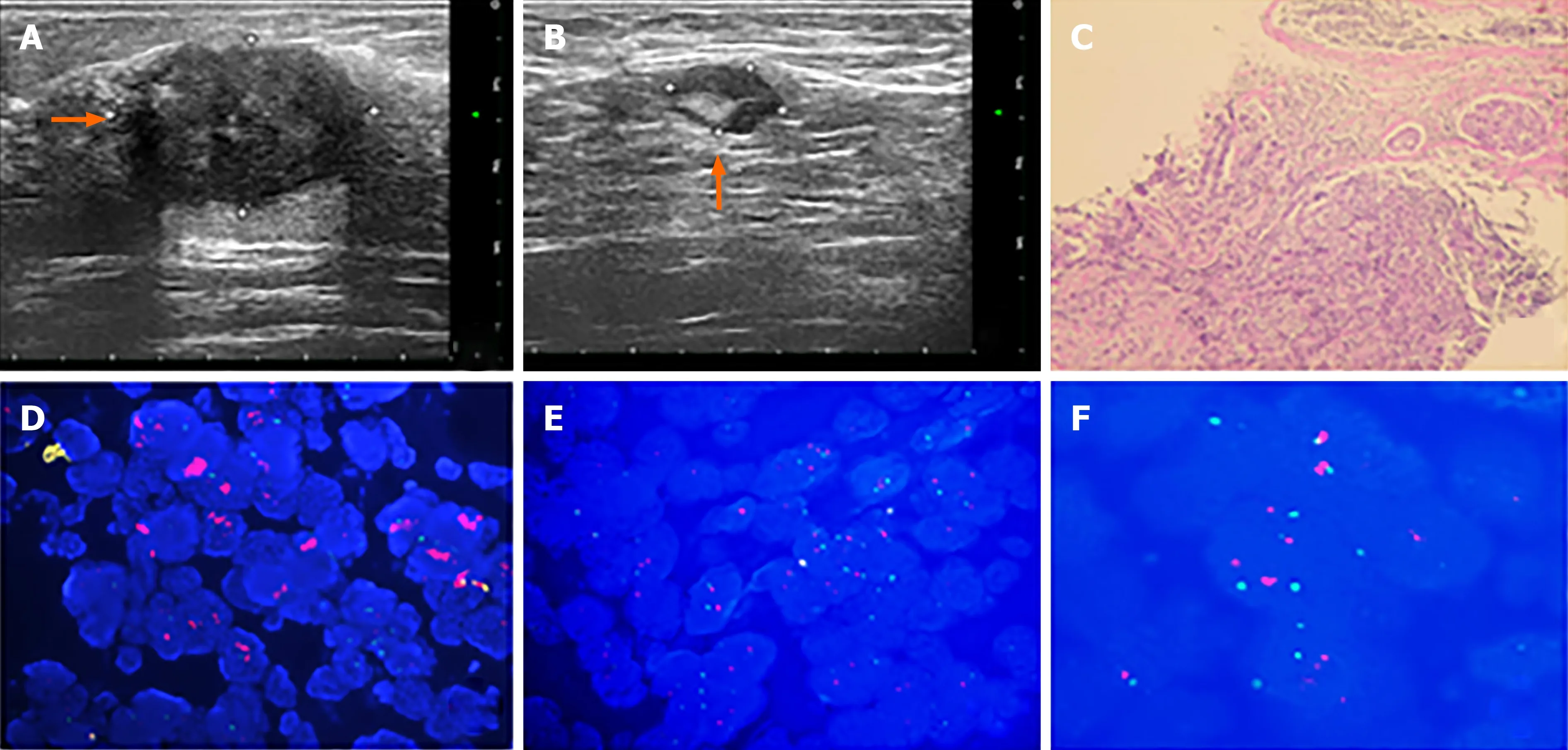
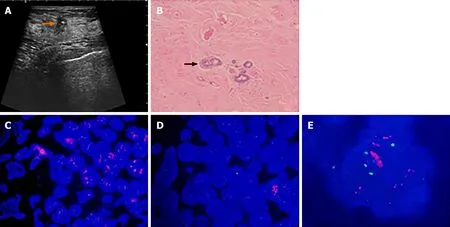
The patient discovered a mass in her right breast and underwent diagnostic workup, including a mammogram which showed a nodule and ultrasound that revealed a mass measuring 2.73 cm × 2.13 cm × 2.57 cm, as well as several enlarged axillary lymph nodes with the largest measuring 1.2 cm × 0.9 cm. Biopsies of the right breast lesion and axillary lymph nodes were obtained. The results pointed to invasive ductal carcinoma with the IHC result for ER (80%), PR (60%), Ki-67 (20%) and ambiguous expression of HER2 (IHC 2+) with negative amplification by FISH (HER2/CEP17 ratio of 1.13) (Figure 1). Computed tomography (CT) of the chest, abdomen, and pelvis showed no sign of metastatic foci and emission computed tomography (ECT) showed negative results. Accordingly, the patient was classified as stage IIB. The patient received NACT with epirubicin and cyclophosphamide for 4 cycles followed by docetaxel every 3 wk for 4 cycles and she was also supported by long-acting injections to improve the quantity of leukocytes. As a result, the lesion significantly reduced in size and the patient achieved a partial remission according to the RECIST1.1 criteria, and ultrasound showed that the focus had reduced to 0.8 cm × 0.7 cm and no obvious echo of enlarged lymph nodes in the axilla. The patient subsequently underwent lumpectomy of the right breast tumor. Pathological findings of the surgically resected sample supported invasive ductal carcinoma with the tumor measuring 1.1 cm × 0.8 cm × 0.5 cm and had spread to one of fifteen dissected lymph nodes. Retesting of the specimen showed that the tumor was positive for ER (2+, 85%) and PR (2+, 10%) but negative for HER2 by IHC (1+). Also Ki-67 had dropped to 2%. However, HER2 amplified by FISH showed a HER2/CEP17 ratio of 2.46 (Figure 2). The patient completed radiotherapy after surgery. Currently, she is undergoing endocrine treatment with tamoxifen and dual targeted therapy with trastuzumab and pertuzumab. Follow-up which included breast ultrasound, abdominal ultrasound and chest CT were regularly performed every 3 mo without evidence of recurrence.
A movable mass measuring approximately 2.7 cm × 2.0 cm × 2.5 cm in the right breast and an ipsilateral enlarged axillary lymph node measuring 1.2 cm × 1.0 cm were identified. There was no evidence of disease in the contralateral breast and axillary lymph node.
History of past illness
A mammogram showed a nodule and ultrasound revealed a mass measuring 2.73 cm × 2.13 cm × 2.57 cm, as well as several enlarged axillary lymph nodes with the largest measuring 1.2 cm × 0.9 cm. CT of the chest, abdomen, and pelvis showed no sign of metastatic foci and ECT showed negative results.
Physical examination
Sunrise on the eastern coast is a special event. I stood at Dolphin s Nose, a spur jutting1 out into the Bay of Bengal, to behold2 the breaking of the sun s upper limb over the horizon of the sea. As the eastern sky started unfolding like the crimson3 petals4 of a gigantic flower, I was overcome by a wave of romantic feelings and nostalgia5(,) -- vivid memorie not diminished by the fact that almost ten years had passed.
Laboratory examinations
All laboratory examinations were in the normal range.
Imaging examinations
The patient was healthy without a history of chronic disease or other breast diseases.
FINAL DIAGNOSIS
Before 2010, the status of HER2 was only determined by FISH, and since then, the results of IHC analysis have been combined. According to the ASCO/CAP guidelines,if the IHC result is 3+-, it can be diagnosed as HER2 positive, and if the IHC result is 0/1+-, it is regarded as HER2 negative. In an equivocal situation (IHC2+-), that is, the complete membrane staining of > 10% of tumor cells is weak to moderate intensity, in situ hybridization (ISH) must be performed to determine whether HER2 is amplified or not. Therefore, it is not necessary to supplement FISH to further confirm the status of HER2 in cases with an IHC score of 0 or 1+-. However, as luminal subtypes are more likely to reveal biomarker conversion and limited therapeutic efficiency which is attributed to the decreased expression of Ki-67 in luminal cases after NACT, we chose to perform FISH on the postoperative specimens of this patient. The results suggested that although the IHC score was 1+-, HER2 was actually proved to be amplified. When reviewing previous literature, we found that despite the low positive rate of gene amplification in IHC0/1+- cases, there was always a small discrepancy between IHC and FISH. Only 2% of the gene was amplified in negative (0/1+-) expression cases by FISH among Chinese patients in the study by Shui[4] and was approximately 4% in other populations[5].
TREATMENT
Follow-up including breast ultrasound, abdominal ultrasound and chest CT were regularly performed every 3 mo without evidence of recurrence.
OUTCOME AND FOLLOW-UP
Epirubicin and cyclophosphamide for 4 cycles followed by docetaxel every 3 wk for 4 cycles and then surgery.
DISCUSSION
In her novelization of the tale, titled Deerskin, Robin83 McKinley gives Donkeyskin a talent with animal husbandry, specifically dogs, which she cares for on the prince s estate.Return to place in story.
It has been several years since NACT was recommended for invasive breast cancer patients by the National Comprehensive Cancer Network guidelines. Compared with postoperative adjuvant chemotherapy, NACT not only has the advantage of downgrading the clinical stage to make lumpectomy available for some patients, it also helps to eliminate micro-metastases. In addition, NACT also provides a novel, rapid and low-cost way to evaluate the effectiveness of systemic treatment. In contrast, observation of the efficacy of postoperative adjuvant therapy requires more time, energy and labor. With the popularization of NACT in locally advanced breast cancer, we have compiled the results over the past ten years (Table 1) and found that, compared with the biomarkers in samples obtained by fine needle aspiration or hollow needle biopsy before surgery, postoperative tissue receptors can occasionally produce completely opposite conclusions. The average conversion rate of ER is 7.3%, PR is 15.0% while HER2 is only 6.8% which is consistent with previous data, that is, the status of PR is most inclined to change while HER2 is relatively more stable[3].

The patient was diagnosed with HER2-positive and hormone receptor-positive invasive ductal carcinoma.
At present, there is no concensus on the mechanism of NACT on HER2 status. Some researchers believe that the small tissue samples obtained by fine needle aspiration are insufficient to represent the phenotypic characteristics of the entire tumor as different molecular expressions may be displayed in specimens. Some studies have taken heterogeneity within the tumor into account. It has been speculated that NACT kills cells that are sensitive to chemotherapy and the remaining cells gradually dominate during the treatment process resulting in a different appearance with subsequent unfavorable characteristics and composition[6]. Another group assumed that a low level of estrogen in the body after NACT down-regulates the expression of ERs in tumor cells[7]. The management of HER2 expression is partly dependent on ER and the status transition also affects each of these parameters[8]. Therefore, NACT indirectly affects the status of HER2. One study has recently discovered that HER2 targeted therapy can also result in differential expression of genes[9]; thus, we predict that NACT can induce subtle changes in gene stability. In addition, it is worth noting that drugs that target cell microtubules such as paclitaxel can lead to polyploidization of cells, that is, all chromosomes multiply, including those that carry HER2. This is followed by increased copy number of the HER2 gene and the outcome is not equal to the actual amplification of HER2, which seems to explain why some patients are resistant to drugs even if the copy number of HER2 increases[10]. Although statistical and staining biases are rare and the criteria for defining IHC ambiguity (IHC 2+-) varies among trials, they should not be ignored. On the contrary, Parinyanitikul[11] analyzed HER2 mRNA level after treatment and the results indicated that the level of HER2 expression in most patients remained stable.
The prognosis of these receptor discordances after NACT are multifarious. For patients with locally advanced breast cancer, HER2 overexpression is an independent risk factor regarding 5-year disease-free survival (DFS). In the multivariate analysis by Tural[12], clinical stage of the tumor, transformation of HER2 from positive to negative and triple negative receptor status significantly influenced DFS. Li[13] included 2847 patients from eight studies and found that patients with hormone receptors (HR) which changed from positive to negative had worse DFS. Moreover, compared with patients who maintained negative HR status after NACT, those with negative HR which changed to positive tended to have longer DFS and overall survival. However, there are a variety of cut-off values to define HR positivity including 1%, 5% and 10% with few employing the Allred score, therefore they came to a contradictory conclusion regarding the prognosis of negative conversion of ER and PR status after NACT[2,14]. We cannot simply attribute this to different definitions as the total number of patients and their characteristics may also play a role. Additionally, the level of the protein encoded by the MKI67 gene (Ki67) is another independent predictive factor. A high Ki-67 index before surgery is associated with achieving a complete clinical response to NACT[15], whereas a high Ki-67 proliferation index in post-NACT samples is related to shorter DFS.
She said no, and would not hear of it; so the man went out again, and settled with the White Bear that he should come again next Thursday evening, and get her answer
Nowadays, the status of HER2 can easily be influenced due to the combination of NACT and HER2-targeted therapy. Therefore, verification procedures should routinely be performed pre- and post-NACT. The decision whether or not to administer HER2-targeted therapy or endocrine therapy is largely based on the result. The estimation of rates of recurrence and outcome can also be affected. We expect the patient in this report to benefit from the use of trastuzumab and pertuzumab in the days to come.
Next morning she sat down beneath the walls of the castle to play with the golden apple, and the first person she saw was the maiden23 with the long nose, who was to have the Prince
CONCLUSION
The conversion of the status of biomarkers including ER, PR, HER2 and Ki-67 is important. Reassessment of the status of these biomarkers after NACT is recommended, especially in patients with luminal subtypes.
World Journal of Clinical Cases2022年1期
- World Journal of Clinical Cases的其它文章
- Hepatitis B virus reactivation in rheumatoid arthritis
- Paradoxical role of interleukin-33/suppressor of tumorigenicity 2 in colorectal carcinogenesis: Progress and therapeutic potential
- Changes in rheumatoid arthritis under ultrasound before and after sinomenine injection
- Benefits of multidisciplinary collaborative care team-based nursing services in treating pressure injury wounds in cerebral infarction patients
- Outcomes and complications of open, laparoscopic, and hybrid giant ventral hernia repair
- Surgical resection of intradural extramedullary tumors in the atlantoaxial spine via a posterior approach
