Positron emission tomography and magnetic resonance imaging combined with computed tomography in tumor volume delineation:A case report
INTRODUCTION
Hypopharyngeal carcinoma is one of the malignant tumors that occur in the head and neck, accounting for 0.15%-0.24% of the total malignant tumors. The anatomical structure is complex, the early symptoms are often unclear, and lymph node metastasis is easy to develop; thus, all three factors contribute to the poor prognosis of hypopharyngeal carcinoma, and the 5-year survival rate is only about 51.3%[1]. Therefore, it is of great significance to make an early diagnosis and plan the treatment accordingly. The main treatments for hypopharyngeal cancer are surgery and radiotherapy.
Currently, patients with previously untreated and newly diagnosed hypopharyngeal cancer have options for surgery to remove the primary tumor and lymph node metastasis, radiotherapy, systemic medical treatment, including traditional chemotherapy and immunotherapy. Radiotherapy can treat hypopharyngeal carcinoma in patients who are not suitable for surgery of the primary tumor. Besides, a small number of patients use radiotherapy as a palliative approach[2]. Intensitymodulated radiation therapy (IMRT) is the mainstream of modern radiotherapy technology and is an effective treatment method for head and neck cancer patients. IMRT can precisely deliver a high radiation dose to the tumor while maintaining a low dose target area for essential tissues and organs around the tumor. The proper delineation of gross tumor volume (GTV, including the gross tumor volume of hypopharyngeal tumor and the involved lymph node) is the key to realizing the overall radiotherapy effect of hypopharyngeal cancer. However, the wrong target volume affects the treatment and damages normal tissues and organs, mainly when critical anatomical structures frequently surround the head and neck tumor. The accurate delineation of GTV is essential for optimal radiation treatment of any tumor, as it can maximize radiation dose to the tumor and minimize that to nontumor tissue[3]. Before outlining GTV, most radiotherapy plans are based on computed tomography (CT) positioning images, which can be used directly in the calculation of radiotherapy dose because of the fast speed of spiral CT scanning, small image distortion, little influence by organs movement, and the linear relationship between CT value and human body density. However, the disadvantage of CT lies in its poor resolution of the boundary of human soft tissue and its inability to define the tumor area accurately. Therefore, only relying on CT images can no longer meet the needs of treatment. Besides, positron emission tomography (PET) and magnetic resonance imaging (MRI) have advantages in accurately diagnosing tumors. PET is an imaging technique that reflects the gene, molecule, metabolism, and functional state of lesions. It uses positron nuclide labeled glucose as an imaging agent to reflect the metabolic changes of lesions through the uptake of imaging agents and to provide clinical biometabolic information of diseases. As cancer cells multiply rapidly and metabolize profusely, only radionuclide-containing imaging agents can be used to contrast them. The advantage of MRI is that it has superior soft tissue contrast and fewer dental artifacts, which can clearly distinguish tumors from surrounding soft tissues[4]. Previous studies[5,6] have shown that it is challenging to delineate GTV based CT images alone; however, an accurate delineation can significantly improve while image fusion occurs between CT and PET or CT and MRI. So far, no relevant studies have combined the fusion images of PET-CT and MRI-CT to provide full play and combine their respective strengths to bring the images closer to the actual volume of tumor. Therefore, we would like to present a clinical case to emphasize the awareness of this condition and show that the combination can play a significant role in delineating tumor volume.
CASE PRESENTATION
Chief complaints
A 67-year-old male patient had pharyngalgia and dysphagia without an obvious cause. The symptoms gradually worsened, and he had later developed dyspnea. After completing relevant examinations, he was diagnosed with hypopharyngeal carcinoma.
His foot hurt, but it was nothing compared with his hunger, which made him go on until darkness fell. His blanket was wet, but he knew only that he was hungry. Through his restless7 sleep he dreamed of banquets8() and of food. The man woke up cold and sick, and found himself lost. But the small sack was still with him. As he dragged himself along, the sack became heavier and heavier. The man opened the sack, which was full of small pieces of gold. He left half the gold on a rock.
History of present illness
A pharyngeal mass biopsy revealed that the dimension of the tumor was 6.0 cm × 4.5 cm × 12.5 cm. The postoperative pathological diagnosis showed squamous cell carcinoma with small focal high-grade neuroendocrine carcinoma. The clinical stage was confirmed as T4N3Mx based on the results of MRI.
History of past illness
Do not thus afflict yourself, my good master. You have nothing else to do but to give me a bag13 and get a pair of boots14 made for me that I may scamper through the dirt and the brambles, and you shall see that you have not so bad a portion in me as you imagine.
Personal and family history
The patient was emaciated and anemic, and had multiple enlarged lymph nodes on both sides of his neck.
Physical examination
The patient claimed to have been an alcoholic for more than 20 years and did not have a history of smoking or a notable family medical history.
Laboratory examinations
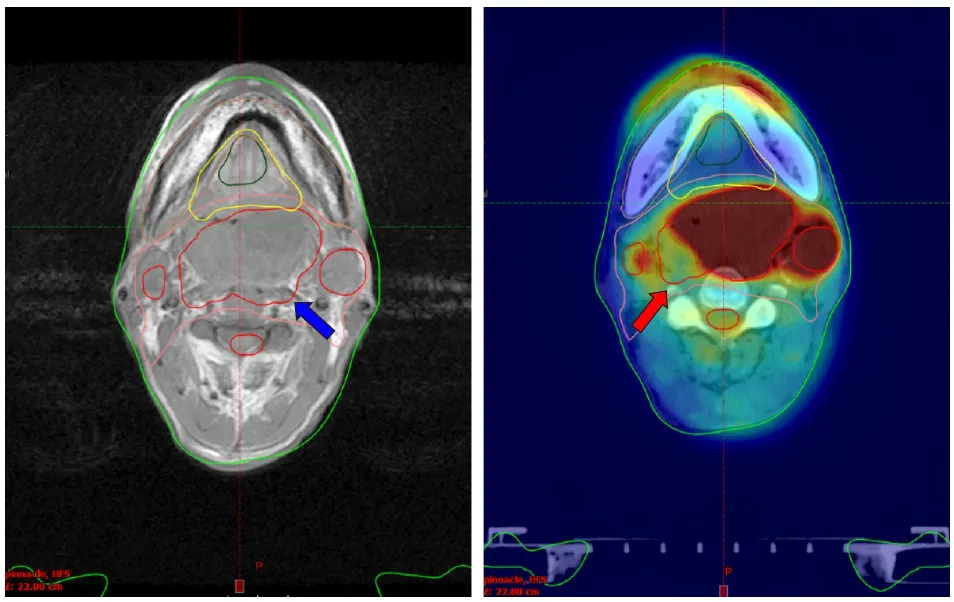
Neither surgery nor chemotherapy was applied to the patient due to multiple associated diseases, such as diabetic nephropathy, renal insufficiency, and emphysema. Besides, surgery could not achieve a radical cure. Hence, radiotherapy was the only option to control tumor progression after a multi-department consultation in our hospital. He was examined by CT, MRI, and 18-fluorodeoxyglucose (FDG)-PET for his treatment plan, including CT fused with PET and MRI to delineate the tumor volume (Figure 1).
Imaging examinations
Fortunately, the patient recovered and was discharged after radiotherapy. The patient was reexamined by MRI scans 3 mo later and showed no signs of tumor recurrence.
No data were available.
FINAL DIAGNOSIS
Hypopharyngeal carcinoma.
TREATMENT
No data were available.
OUTCOME AND FOLLOW-UP
MRI of the nasopharynx and neck showed thickened left piriform fossa wall with a soft tissue mass, filling of the laryngopharynx oropharynx cavity, and involving the right piriform fossa, consistent with hypopharyngeal carcinoma. There were multiple lymph nodes in the bilateral neck, of which the larger one was located in bilateral neck areas II-III, suggesting lymph node metastasis.
When we were eating I choked with that very button(). I felt as if a little stone was stuck in my throat – neither could breathe in nor breathe out. Understanding that if I wouldn’t be able to clear my throat now I would go west. At this thought I became unconscious…
DISCUSSION
MRI permits multi-sequencing and multi-parametric imaging with higher soft tissue resolution than CT, making the actual boundary between tumor and soft tissue more precise, and causes no radiation damage[7]. MRI-CT image fusion can avoid overestimation of clinical tumor volume by CT images only. Tzikas[8] compared fused MRI-CT with only CT images in radiotherapy plan, and found that the dose distribution generated by fused MRI-CT image could achieve better treatment results, leading to a lower complication rate of principal organs at risk than that of CT images. Although MRI complements the lack of soft tissue resolution of CT images, both have a limited sensitivity and specificity concerning the presence or extent of nodal involvement, because they mainly rely on the size criterion. Thus, MRI-CT fusion images cannot reveal nodal disease in normal-size lymph nodes. Besides, accuracy is lacking in defining the dimension of malignant bone infiltrationconcomitant infectious bone reactions[9]. Our research also showed that MRI-CT fusion images failed to show the bone invasion site.
In PET, 18F-labeled FDG (F-FDG fluorinated deoxyglucose) is used as the tracer. The level of glucose utilization can determine the tumor and invasion site, and metabolic imaging is one of the most sensitive methods for the early diagnosis of malignant tumors. PET can reflect the differences in the metabolic status and biochemical changes of tumor tissues at the molecular level by providing living biological information while determining the clinical tumor volume, making up for the shortcoming of CT to provide information of the vitality of tumors. PET-CT image fusion can simultaneously show metabolic activity and anatomical location to achieve a more accurate delineation of GTV and provide more effective protection for the surrounding normal organs and tissues. However, the distribution of 18F-FDG is not limited to malignant tissues; thus, PET-CT fusion images can also lead to false negative and false positive results in tumor diagnosis[7]. False-positive results in PET-CT may occur due to inflammation, limited spatial resolution, and lack of a standard method for segmentation[4]. However, false-negative results may occur in some slow-growing or low-malignant tumor cells or in necrotic tumor tissues, where glucose metabolism is reduced.
His elder brothers, who had in vain gone in pursuit of the thief of the golden apples, were furious over their younger brother s good fortune, and plotted and planned how they were to kill him
CONCLUSION
The image fusion of MRI-CT and PET-CT has both advantages and disadvantages. Hence, combining the two can cover the GTV of hypopharyngeal cancer more accurately than CT images alone, which is more likely to improve the radiotherapy effect and reduce the risk of recurrence and is worthy of further development in clinical practice.
World Journal of Clinical Cases2022年1期
- World Journal of Clinical Cases的其它文章
- Hepatitis B virus reactivation in rheumatoid arthritis
- Paradoxical role of interleukin-33/suppressor of tumorigenicity 2 in colorectal carcinogenesis: Progress and therapeutic potential
- Changes in rheumatoid arthritis under ultrasound before and after sinomenine injection
- Benefits of multidisciplinary collaborative care team-based nursing services in treating pressure injury wounds in cerebral infarction patients
- Outcomes and complications of open, laparoscopic, and hybrid giant ventral hernia repair
- Surgical resection of intradural extramedullary tumors in the atlantoaxial spine via a posterior approach
