Characterization of focal hypermetabolic thyroid incidentaloma: An analysis with F-18 fluorodeoxyglucose positron emission tomography/computed tomography parameters
INTRODUCTION
The incidence of thyroid cancer has been increasing worldwide since the last few decades[1-3], although its mortality rate is relatively stable[4,5]. According to a recent report from a national institute of South Korea, the disease was ranked as the second most frequent cancer in women after breast cancer in 2018, and it was three times more common in women than in men[6]. Cancer predominantly occurs in older individuals; however, thyroid cancer and breast cancer have their highest frequencies at relatively young ages[7]. In both sexes, thyroid cancer is most frequently found between the ages of 15 and 34 years[6,7]. Moreover, the age-standardized incidence of thyroid cancer is reported to be 48.9 for both sexes, and it is 75.5 in women, which is higher than 65.6 for breast cancer[6]. Thyroid cancer is becoming more common among younger women.
But the children were awake, and had heard the conversation. When the old people were asleep Hansel got up, and wanted to go out and pick up pebbles again, as he had done the first time; but the woman had barred the door,27 and Hansel couldn t get out. But he consoled his little sister, and said: Don t cry, Gretel, and sleep peacefully, for God is sure to help us.
2 -Deoxy-2-[F] fluoroglucose or F-18 fluorodeoxyglucose (F-18 FDG) positron emission tomography-computed tomography (PET-CT) is used widely in the diagnosis, treatment evaluation, and follow-up of cancer. However, its role in thyroid cancer is not as definite as in other cancers. This imaging modality is rather limited and might be used for thyroid cancer in cases of elevated blood thyroglobulin without obvious abnormal iodine uptake on a whole-body scan after total thyroidectomy and/or radioactive iodine therapy[8-10].
In this situation, an unexpectedly detected thyroid lesion (thyroid incidentaloma, TI) with high F-18 FDG uptake (hypermetabolism) may have important implications. This retrospective study was conducted to distinguish malignant hypermetabolic TIs from benign disease by analysing FDG PET-CT parameters of hypermetabolic TIs on PET-CT performed at our hospital for non-thyroid purposes and to identify an optimal cut-off value.
MATERIALS AND METHODS
Patients
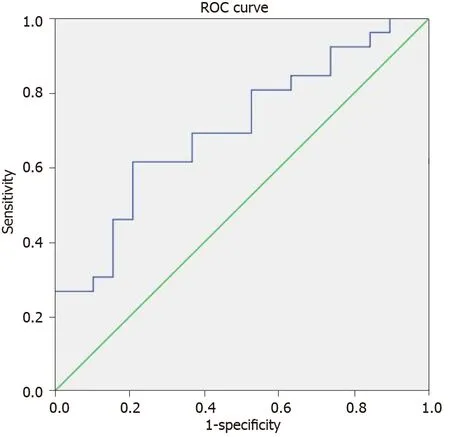
SUVwas chosen for the ROC curve. Based on the AUC[42,43], SUVhas a power of fair discrimination with approximately 70% probability for malignancy in an unexpectedly identified focal hypermetabolic thyroid lesion. The lesions with SUVhigher than 8.5 have a greater chance to be malignant with a sensitivity of 61.5% and a specificity of 78.9%. Some cases of Hurthle cell adenoma, which might have high FDG uptake[44-46], were included in the benign group and these could reduce the sensitivity and AUC, making the discrimination difficult. The reading of PET-CT images relies mainly on the naked eye qualitatively and it is not simple to distinguish malignant lesions from benign ones with a high FDG uptake. Relatively rare metastatic lesions from other cancers could also have a high FDG uptake[47-49]. Therefore, SUVwith a reference of suggested cut-off value should be measured in cases of hypermetabolic TI, and further active examination is recommended to characterize lesions above the threshold.
Imaging of F-18 FDG PET-CT
All patients were required to fast for 4-6 h and had their blood glucose level checked before acquiring F-18 FDG PET-CT to ensure optimal image quality. When the blood glucose level was greater than or equal to 11 mmol/L (200 mg/dL), the scan was rescheduled. Scanning was performed 60 min after intravenously injecting 185 MBq F-18 FDG. Images from the skull base to the upper thigh were acquired using a dedicated PET-CT scanner, Biograph mCT 128 (Siemens Healthcare GmbH, Erlangen, Germany). Individually optimized images with lower patient radiation exposure were obtained with the emission scan performed for 3 min per bed by the step and shoot method and the CT scan performed in the continuous spiral mode with functions such as CareDose4D and CARE kV based on the default values of 60 mAs and 120 kVp, respectively. No contrast material was used for the CT scan. Both PET and CT images were reconstructed by the iterative reconstruction method, and fusion PET-CT images were generated on the dedicated image acquisition workstation provided with the PET-CT equipment.
The number of diagnoses of thyroid cancer has been increasing for several decades, and this includes TIs identified by PET-CT, CT, magnetic resonance imaging, and US conducted for non-thyroid purposes. Well-differentiated thyroid cancers such as papillary and follicular cancers, which develop from thyroid follicular cells, comprise more than 85% of all thyroid cancers[11,12]. Well-differentiated thyroid cancers are known to be less aggressive and have a better prognosis than other thyroid cancers such as poorly differentiated thyroid cancer, anaplastic thyroid cancer, or Hurthle cell cancer; however, up to 5% of well-differentiated thyroid cancers could become dedifferentiated and aggressive[13-15]. Dedifferentiated thyroid cancer is generally not very responsive to radioactive iodine therapy, while well-differentiated cancer shows a good response. FDG is easily taken up by aggressive cancers with less/noniodine-avidity or by tumors with increased malignancy due to the elevated expression of glucose transporter 1. As the majority of thyroid cancers are slow-growing welldifferentiated types, they are generally less FDG avid, and F-18 FDG PET-CT has a limited role in the initial evaluation. It is usually only used for the evaluation of recurrences after resection and/or iodine therapy when the thyroglobulin level in the serum is suspicious without definite abnormal findings on US or an iodine wholebody scan. Therefore, the focus of this study is not on the initial evaluation of thyroid cancer but on unexpectedly identified FDG uptake by the thyroid on PET-CT performed for the diagnosis or follow-up of other cancers.
Analysis of the F-18 FDG PET-CT images and cytological/histological results
Two nuclear medicine physicians examined the F-18 FDG PET-CT images. Once they identified an abnormal FDG uptake by the thyroid, they looked up the patient’s medical record to obtain the US and cytological/histological reports, then the lesion was categorized as malignant or benign according to the cytological/histological report when available. The maximum, peak, and mean of the semi-quantitative standardized uptake value (SUV) of focal TI were measured. SUVs of the contralateral thyroid were also measured. Additionally, the metabolic tumor volume (MTV) of TI was measured. The volume of interest (VOI) for measuring MTV can be drawn differently using different SUV thresholds. In this study, multiple SUV thresholds from 2 to 5 with an increment of 0.5 were used to obtain multiple MTVs. Finally, total lesion glycolysis (TLG) was calculated by multiplying MTV by the mean SUV. All imaging analyses were performed on a dedicated PET-CT workstation equipped with SyngoMMWP (Siemens Healthcare GmbH, Erlangen, Germany). These five parameters were compared between malignant and benign TIs, and receiver operating characteristic (ROC) curve analysis was performed to identify a cut-off value.
Statistics
Both parametric and non-parametric methods were used to compare SUV, SUV, SUV, MTV, and TLG between the malignant and benign lesions. Point biserial correlation was performed for the parameter(s) and malignancy. ROC curves were plotted, and the area under the curve (AUC) was calculated to determine an optimal cut-off value. Statistical analysis was performed using SPSS 16 (IBM, Armonk, New York, United States). Avalue of less than 0.05 was considered statistically significant.
He paused to listen, and heard the King of the Ants complaining: If only men with their awkward beasts would keep clear of us! That stupid horse is crushing my people mercilessly to death with his great hoofs17
Ethics
This retrospective study was approved by the institutional review board of our hospital (IRB no. GAIRB2020-297), and the requirement to obtain informed consent was waived. The study was conducted in accordance with the 1964 Declaration of Helsinki and later amendments.
RESULTS
The higher the semi-quantitative SUV on F-18 FDG PET-CT, the higher is the possibility of cancer with various reported cut-off values, and this is related to the prognosis and overall survival[23-26]. Among the five PET parameters associated with SUV and the metabolic volume of the tumor, SUVshowed good performance in discriminating malignant lesions from benign ones. The mean value of SUVwas higher in the malignant group and presented a statistical significance difference comparable to SUVin some conditions (SUV threshold of 2.0 and 2.5). This could be associated with a larger volume of benign lesions with the same SUV thresholds. There was no statistical significance for the SUVwith other SUV thresholds where the volumes were all larger in the malignant group. In a situation with a low SUV threshold, the VOI might include areas outside the tumor, and consequently, the final measured volume could be larger than the real volume. SUVmight be influenced and reduced as the volume of benign lesions is unintentionally larger, and this could lead to a significant statistical difference from that of malignant lesions. The mean values of SUVand TLG were higher in the malignant group but without statistical significance, although SUVcaught our attention with a-value of 0.058, which was close to significance.

PET-CT parameters
Five representative parameters of PET-CT (SUV, SUV, SUV, MTV, and TLG) were compared to evaluate the differences between malignant and benign lesions. Table 3 shows an example of these parameters. The average SUVof 26 malignant lesions and their contralateral isometabolic thyroid areas without US-identified lesions was 10.8 ± 7.5 and 2.5 ± 1.2, respectively, with a statistically significant difference (< 0.05). Similarly, the average SUVof benign lesions and their contralateral thyroid areas was 6.5 ± 3.0 and 2.1 ± 0.7, respectively, also with statistical significance. There was a significant difference between the SUVof malignant and benign focal thyroid lesions (= 0.012). The SUVof contralateral thyroid areas of both malignant and benign lesions presented no significant difference. Point biserial correlation resulted in a statistically significant positive linear correlation (= 0.339) between SUVand the malignant cytological/histological report (< 0.05).
He was the president of a major advertising1 firm and I was a very young management consultant2. I had been recommended to him by one of his employees who had seen my work and thought I had something to offer. I was nervous. At that stage in my career, it wasn’t very often that I got to talk to the president of a company.
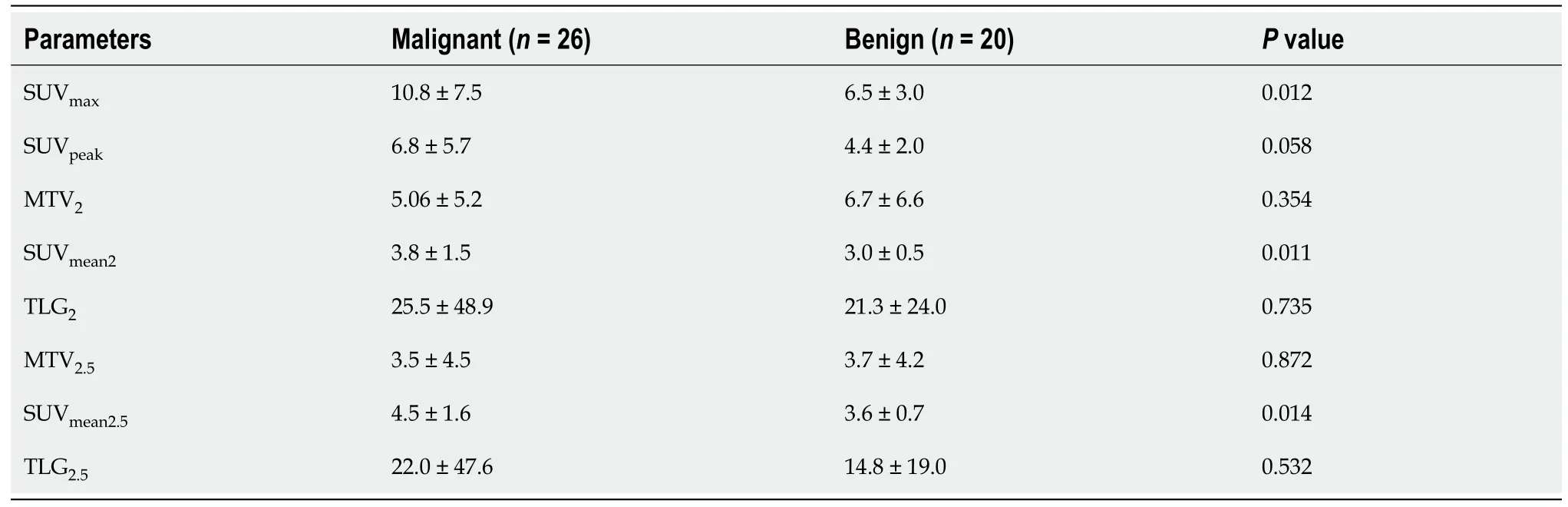
SUVpresented no statistical significance with a-value of 0.058, which was close to significance. The SUVshowed statistical significance with a threshold of 2 (= 0.011) and 2.5 (= 0.014). The SUVwith other thresholds, MTV, and TLG failed to show any statistical significance.
An ROC curve was plotted for SUV(Figure 2), and the AUC was 0.702 (< 0.05, 95% confidence interval: 0.550-0.855). The SUVcut-off value was 8.5 with a sensitivity of 0.615 and a specificity of 0.789.
DISCUSSION
He was not much older than the Princess, and was as handsome a Prince as you would see in a day s journey, and really, for his age, not so very scatter- brained
No, indeed; the most singular flowers and plants grow there; the leaves and stems of which are so pliant4, that the slightest agitation5 of the water causes them to stir as if they had life
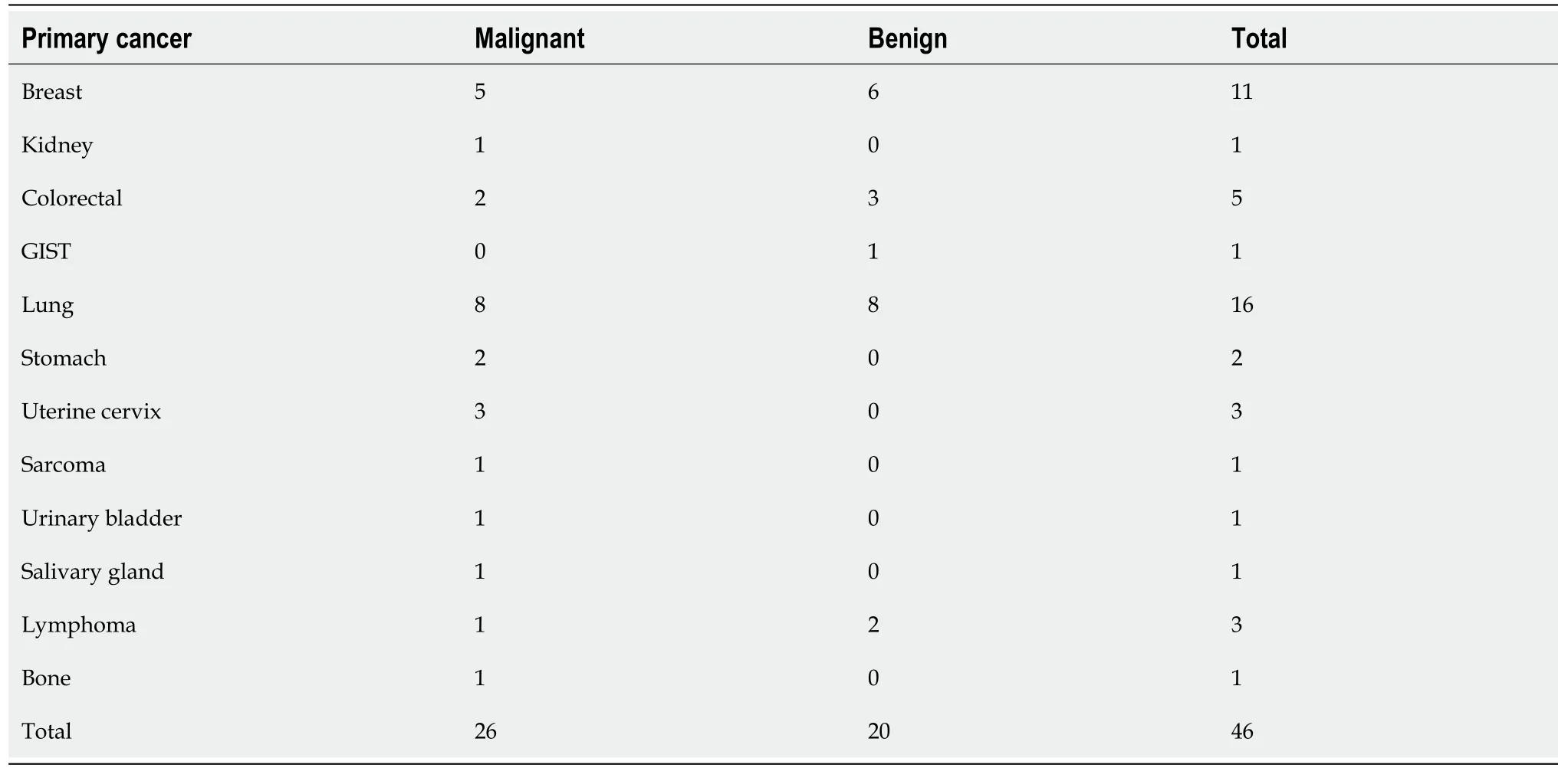
Diffuse thyroid FDG uptake has a greater chance of being benign thyroid diseases such as thyroiditis or hypothyroidism than cancer[16,17]. However, about 25%-50% of focal hypermetabolic TIs, with a prevalence of 2.5%-5%, have malignant cytological/histological reports[18-22]. In other words, approximately half of hypermetabolic TIs could have a risk of malignancy, and therefore, it is critical to differentiate them as malignant or benign. In this study, 2.7% of total available PET-CT images had either diffuse or focal abnormal thyroid hypermetabolism, and 13.6% (46/339) of these presented focal hypermetabolism. Finally, 56.5% of the latter were diagnosed as cancer and, within the known range, 88.5% (23/26) of the pathologically confirmed malignant lesions were well-differentiated thyroid cancers. From this, it is suggested that any 2 out of 1000 FDG PET-CT scans have a possibility of incidentally finding thyroid cancer.
Of the 23 well-differentiated malignant lesions of this study, 19 were available for the BRAF mutation test, and 100% (19/19) lesions were proved to have the mutation. This (dedifferentiation) could be associated with a change in FDG avidity from low to high. As this study was conducted on any hypermetabolic lesions discovered with the naked eye, lesions not yet advanced, which is why they had low FDG uptake and therefore had less chance to be observed on images, were likely excluded from the study. This unrecognized selection bias probably resulted in a high FDG uptake even in lesions of well-differentiated thyroid cancer. Conversely, if thyroid cancer was diagnosed pathologically first and then FDG PET-CT was performed, there would be more lesions with low FDG uptake.
More than half of the focal hypermetabolic TIs on F-18 FDG PET-CT were revealed as malignant. SUVwas the best parameter for discriminating malignant and benign lesions. The unexpected focal hypermetabolic TIs with an SUVabove the cut-off value of 8.5 may have a greater than 70% chance of malignancy; therefore, further active assessment is required to characterize these lesions.
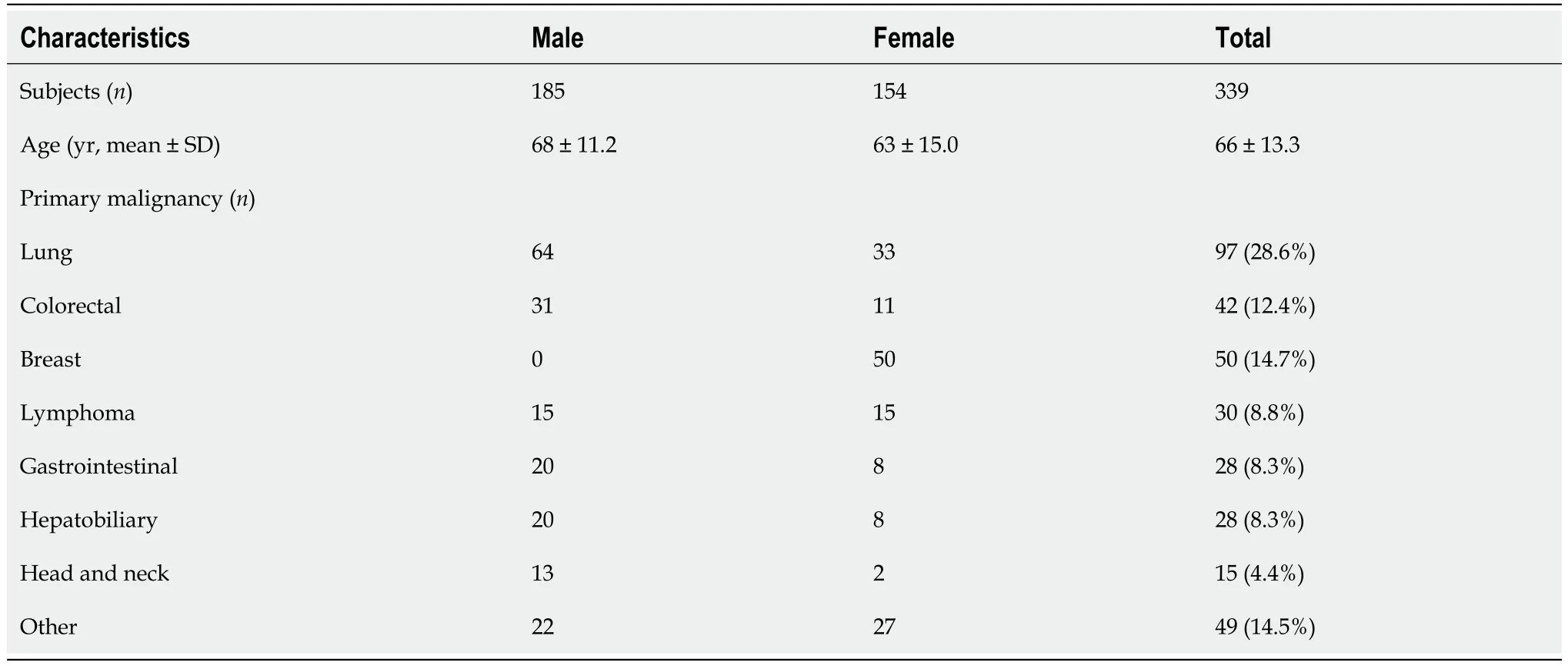
Approximately 2.7% (339/12761) of all FDG PET-CT images reviewed initially showed abnormal thyroid hypermetabolism. The demographic and clinical characteristics of these 339 patients are shown in Table 1. Amongst the 339 non-thyroid disease patients [185 men (mean age: 68 ± 11.2) and 154 women (mean age: 63 ± 15.0 years)] with incidental suspicious hypermetabolism of the thyroid gland, 46 patients [13.6%, 12 men (mean age: 62 ± 13.1 years) and 34 women (mean age: 60 ± 12.0 years)] had focal hypermetabolism on PET-CT, and the hypermetabolic location was identified as a nodule on US and confirmed by cytological/histological analysis. Figure 1 shows some representative PET-CT images of such cases. Overall, 56.5% (26/46) of the cases were malignant, and the rest 43.5% (20/46) were benign. Amongst malignancy cases, 84.6% (22/26) were papillary, 3.8% (1/26) follicular, 3.8% (1/26) poorly differentiated, and 7.7% (2/26) Hurthle cell malignancies. Their primary cancers and cytological/histological results are presented in Table 2. Additionally, of the 23 well-differentiated thyroid cancer lesions, BRAF mutation test results were available for 19 cases, and all the 19 lesions were confirmed to have the mutation.
“But we have the best bird after all,” said one, and then they would have the bird sing again, although it was the thirty-fourth time they had listened to the same piece, and even then they had not learnt it, for it was rather difficult. But the music-master praised the bird in the highest degree, and even asserted that it was better than a real nightingale, not only in its dress and the beautiful diamonds, but also in its musical power. “For you must perceive, my chief lord and emperor, that with a real nightingale we can never tell what is going to be sung, but with this bird everything is settled. It can be opened and explained, so that people may understand how the waltzes are formed, and why one note follows upon another.”
There are studies on TIs reporting that MTV, TLG, or both are useful parameters in distinguishing malignant lesions from benign ones[27-31], while other reported different conclusions[32]. The roles of MTV and TLG in other cancers are still open to debate[33-36]. In this study, both MTV and TLG were not useful in the discrimination. TLG was expected to be a good discriminator initially like SUV, but it was not. This might have something to do with MTV. There are reports that a specific range of thyroid nodule sizes had a greater prevalence of malignancy, while others found no increased risk of malignancy over a specific nodule size[37-41]. These findings imply that a larger size does not necessarily mean a higher possibility of malignancy. MTV might be thought of in a similar way, and thus a larger MTV does not always mean malignancy. In this way, there is a possibility that TLG, which is the product of SUVand MTV, might not reflect the risk of malignancy well. Finally, SUVwas the only reliable discriminator, while SUVmight be a candidate. In contrast, the other parameters had no discernible statistical impact.
We retrospectively reviewed the imaging data of 12761 patients who underwent F-18 FDG PET-CT to evaluate or follow-up their newly or previously diagnosed malignant disease, except for thyroid cancer, at our hospital between January 2016 and December 2020. We identified 339 patients (185 men and 154 women with mean age 68 ± 11.2 years and 63 ± 15.0 years, respectively) whose images presented incidentally abnormal hypermetabolism in their thyroid. From those, we selected patients with focal thyroid hypermetabolism after exclusion of the cases with known thyroid lesions and diffuse FDG uptake in or around the thyroid. The reports of ultrasonography (US) and, as a gold standard, cytological/histological examinations from fine-needle aspiration cytology or thyroidectomy were collected for the selected patients. Those with the reports of all three examinations were eligible for inclusion in this study.
CONCLUSION
All of the patients involved in this study already had one type of cancer but not thyroid cancer, and we excluded PET-CT images acquired for benign diseases or health check-ups. This patient selection might influence the malignancy rate, especially since there is a report describing the prevalence of TI being higher in patients with cancer than in healthy subjects[19].
ARTICLE HIGHLIGHTS
Research background
Thyroid incidentaloma (TI) is detected on imaging studies for non-thyroid purposes and the lesion may harbor a risk of malignancy. It is critical to distinguish malignant TI from benign disease.
Research motivation
The higher the metabolism on F-18 fluorodeoxyglucose (FDG) positron emission tomography-computed tomography (PET-CT) image, the higher the possibility of malignancy. TI might be characterized depending on the FDG metabolism.
Research objectives
To distinguish malignant hypermetabolic TIs from benign disease by analyzing F-18 FDG PET-CT parameters and to identify a cut-off value.
AllisonClark,Clark 78,Allison35,……Allison and her husband, Clark, who is much older than she, spend an evening carving1 pumpkins3 until early the next morning.
Research methods
The values of parameters from FDG PET-CT of 46 focal hypermetabolic thyroid lesions were measured, calculated, and compared. Receiver operating characteristic (ROC)curve was plotted to determine a cut-off value.
Research results
Standardized uptake value (SUV)was the only statistically significant discriminator in differentiation. From the ROC curve, the AUC was 0.702 and the SUVcut-off value was 8.5.
Research conclusions
TIs with SUVabove the cut-off value 8.5 may have a greater than 70% chance of malignancy. A further active assessment is required.
Research perspectives
Other studies and controversies on the parameters included in this study are ongoing.Further studies with a large number of subjects are guaranteed.
World Journal of Clinical Cases2022年1期
- World Journal of Clinical Cases的其它文章
- Hepatitis B virus reactivation in rheumatoid arthritis
- Paradoxical role of interleukin-33/suppressor of tumorigenicity 2 in colorectal carcinogenesis: Progress and therapeutic potential
- Changes in rheumatoid arthritis under ultrasound before and after sinomenine injection
- Benefits of multidisciplinary collaborative care team-based nursing services in treating pressure injury wounds in cerebral infarction patients
- Outcomes and complications of open, laparoscopic, and hybrid giant ventral hernia repair
- Surgical resection of intradural extramedullary tumors in the atlantoaxial spine via a posterior approach
