Clinical characteristics of 72 cases with neuromyelitis optical associated optic neuritis
HAN Meng-yu, QIN Ya-li, JIAO Yu-juan, JIAO Jin-song, MA Chuan-zheng, JIN Ming✉
1. Ophthalmology Department, China-Japan Friendship Hospital, Beijing 100029, China
2. Guangdong Provincial Hospital of Traditional Chinese Medicine, Guangzhou 510120, China
3. Department of Neurology, China-Japan Friendship Hospital, Beijing 100029, China
4. Graduate School of Beijing University of Chinese Medicine, Beijing 100029, China
Keywords:Optic neuromyelitis Optic neuritis Clinical features
ABSTRACT Objective: To analyze the clinical characteristics of neuromyelitis optical associated optic neuritis (NMO-ON) patients, and to provide reference and basis for the prevention and treatment accordingly. Methods: The medical records of 72 NMO patients with ON as the first clinical manifestation in China-Japan Friendship Hospital from January 2016 to December 2019 were retrospectively analyzed and summarized, including general information, morbidity characteristics, course of disease, comorbid diseases, immunological tests, treatment response and prognosis, etc. Results: Totally 72 NMO-ON patients had a median age of 33 years. The ratio of male to female is about 1:5.54; The median course was 67 months, mainly "relapseremission". Totally 61.11% patients were successively involved in both eyes, the median incidence of ON was 2 times, and the median time of the second onset of ON was 3 months.The 1-year and 3-year recurrence rates were 55.56% and 73.61%, respectively. Around 91.67% of the patients had the onset of ON alone, and 81.94% of the patients had monocular involvement. About 19.44% patients were associated with inducement, the most common was upper respiratory tract infection; 15.28% patients were associated with systemic immune diseases, most commonly associated with Sjogren's syndrome and thyroid diseases and 75.64% patients had first visual acuity less than 0.1, aquaporin-4 immunoglobulin G (AQP4-IgG) status (P=0.032, OR =2.55) and onset age (P=0.037, OR=3.93) were independent risk factors for first visual acuity. Up to the last follow-up time, the rate of unilateral blindness was about 48.61%, and the median of unilateral blindness ON was 2 times. Other nervous system involvement occurred in 73.61% of patients, and spinal cord (61.11%) was the most common site of recurrence. Serum AQP4-IgG was positive in 80.00% (48/60) of patients. A total of 18 cases (25.00%) were associated with other systemic immune antibodies, most commonly associated with ANA antibody positivity. Conclusions: The first onset of NMO-ON patients is mostly ON alone, with unilateral involvement and high incidence in young and middle-aged women. Bilateral optic nerve involvement and repeated recurrence are common in the long course of disease. AQP4-IgG status and onset age are independent risk factors affecting the visual function of NMO patients for the first onset, and most patients have positive AQP4-IgG serum. Some patients are associated with systemic immune diseases represented by Sjogren's syndrome and thyroid disease, which are at high clinical risk and require early diagnosis and treatment intervention.
1. Introduction
Neuromyelitis optica (NMO) is an inflammatory astrocyte disease of the central nervous system with neuro-ophthalmic cross, high incidence in Asian population, dominated by humoral immunity, and involvement of various T cells (especially CD4+T cells) and related cytokines. The specific pathogenesis, which is caused by antiaquaporin-4 antibody(AQP4-IgG)binding to AQP4 on astrocytes and mainly involves the optic nerve and/or spinal cord, has attracted great attention due to its young age, high pathogenicity, high risk of recurrence and poor prognosis (blindness and disability) [1,2].With the deepening of the characteristics and clinical understanding of NMO disease, the concept of neuromyelitis optica spectrum disease has been proposed and internationally recognized, enabling NMO patients to receive earlier and timely and appropriate clinical diagnosis, so as to guide patients to formulate clinical prevention and treatment plans and improve prognosis [3,4]. Optic neuritis (ON) is a blinting optic neuropathy most easily suffered by young and middleaged patients in ophthalmology or neuroophthalmology. Acute ON is one of the typical clinical manifestations of NMO patients and may be the initial symptom of NMO, indicating a high risk of permanent visual loss. Foreign small-scale data show that ON is the initial symptom of more than 45% of NMO patients, and the typical clinical manifestations of ON can be seen in more than 60% of AQP4-igg seropositive NMO patients [5,6].
So far, there is no accurate epidemiological data of NMO and its correlation with ON in the world, and the existence of factors such as age, sex, race and AQP4-igg level seems to affect the course of disease and treatment effect [4]. Clinical data ON the pathogenesis, immunological results, therapeutic responses and prognosis of patients with NMO-ON are even scarce. Therefore,from the perspective of ophthalmology, sorting out, summarizing and analyzing the clinical data of NMO patients with ON as the first clinical manifestation has important and potential clinical guiding value and social significance. The purpose of this study was to make a retrospective analysis of the pathogenesis, clinical course,immunological characteristics, related treatment responses and prognosis of patients with NMO-ON in ophthalmology or neuroophthalmology combined Outpatient department of our hospital, in order to provide reference and help for the diagnosis and treatment of patients with clinical ON and NMO.
2. Data and methods
2.1 Subjects
According to the principles of Helsinki Declaration, a retrospective analysis of 72 NMO patients (72/159) with ON as the first clinical manifestation who were treated in ophthalmology or neuroophthalmology combined Outpatient Department of China-Japan Friendship Hospital from January 2016 to December 2019 was conducted. Including the patient's general information, clinical characteristics, disease progression, concomitant diseases,immunological test results, treatment response and prognosis,etc. Aqp4-igg was detected by cell-based immunoassay (CBA) in HEK293 cells transfected with M1 aquaporin 4. This study was approved by the Ethical Review Committee of Clinical Research of China-Japan Friendship Hospital (Ethical Batch Number: 2020-12-K09).
2.2 Diagnostic Criteria
Refer to the 2015 NMOSD diagnostic criteria [4], and see the following for details.
2.2.1 Diagnostic criteria for AQP4-igg positive NMO
(1) At least one core clinical feature; (2) AqP4-igg was detected by a reliable method; (3) Exclude other diagnoses.
2.2.2 NMO diagnostic criteria for negative AQP4-igg or unknown AQP4-igg status
(1) In one or more clinical episodes, at least 2 core clinical features and all of the following conditions are met: at least 1 core clinical feature is ON, acute LETM, or medulla oblongata final zone syndrome; Spatial multiple of 2 or more different core clinical features; Meet the additional conditions of magnetic resonance imaging (MRI); (2) AqP4-igg negative or not detected by a reliable method; (3) Exclude other diagnoses.
2.2.3 Core clinical features
(1) ON; (2) Acute myelitis; (3) Final zone syndrome, with hiccup,nausea and vomiting that can not be explained by other reasons;(4) Other brain stem syndromes; (5) Symptoms of paroxysmal sleeping sickness and diencephalic syndrome, brain MRI showed characteristic diencephalic lesions of NNO; (6) Cerebral syndrome accompanied by characteristic cerebral lesions of NMO.
2.2.4 Additional conditions of NMO MRI in negative aqP4-igg or unknown state
(1) Acute ON: brain MRI has one of the following manifestations:normal brain MRI or only non-specific white matter lesions; Optic nerve long T2 signal or enhanced T1 signal > 1/2 optic nerve length, or lesions involving optic chiasma; (2) Acute myelitis: long myelopathy > 3 consecutive vertebral segments or spinal atrophy > 3 consecutive vertebral segments in patients with a history of myelitis;(3) Final zone syndrome: dorsal medulla oblongata/final zone lesions; (4) Acute brainstem syndrome: brain stem periependymal lesions.
2.3 Inclusion Criteria
(1) The patient's diagnosis met the above NMO diagnostic criteria;(2) The first clinical manifestations of NMO patients included ON.
2.4 Exclusion Criteria
(1) Prior history of other ocular diseases that may affect visual function, including retinal diseases and non-ON optic neuropathy such as glaucoma, was excluded; (2) Patients during pregnancy and lactation were excluded; (3) Exclude those who cannot cooperate with the investigation or follow-up monitoring of disease changes;(4) Exclude incomplete medical records.
2.5 Clinical evaluation
We assessed in patients with NMO-ON the following factors: the onset of demographic data (age, gender, race, residential area),clinical characteristics (symptom, cause, total number of attacks especially ON attack number of times, ON the secondary attack time, recurrence, disease duration, accompanied diseases especially in autoimmune diseases), laboratory data, Aqp4-igg serum status,immunological antibody test results), imaging findings, visual acuity and visual outcome of the first attack of ON, treatment history, follow-up time and visual outcome at the last follow-up,and general discomfort symptoms accompanying the remission stage. The diagnosis of previous ON history was determined by the same ophthalmologist and neuroophthalmologist based ON the patient's previous medical records, history, or optic nerve MRI results. Recurrence was defined as neurological symptoms lasting 24 hours and occurring at least 30 days after the previous event.The date of onset, symptoms experienced, lesion location, treatment(intravenous steroids, plasmapheresis, or intravenous gamma globulin), visual acuity and convalescent visual acuity were recorded for each relapse. Details of symptoms are provided by the patient and confirmed by reference to contemporaneous medical records and related examination results. Annualized relapse rate (ARR) is the number of relapses divided by the number of observation days(years). Convalescent visual acuity refers to the best corrected visual acuity 3 months after each ON episode. Binocular involvement was calculated as two eyes; During the visual acuity prognosis assessment, fractional visual acuity was converted into Snellen score records and visual acuity was assessed for each eye respectively. The assessment criteria [7] were as follows: 0 score: VA > 0.5; 1 score:0.5 VA > 0.2; 2 = 0.2 VA acuity 0.1 or higher; 3 score= 0.1 > VA.
2.6 Statistical processing
The data in this study were analyzed and processed by SPSS 25.0 statistical software. T test was used for measurement data conforming to normal distribution, and non-parametric test was used for measurement data conforming to normal distribution. Pearson Chi-square test was used for comparison of counting data, P<0.05 indicated statistically significant difference. Descriptive methods were used for other statistics (proportion and percentage were used to summarize classification data, mean ± standard deviation was used for continuous data of normal distribution, and median(minimum and maximum) was used for continuous data of nonnormal distribution); Univariate and multivariate logistic regression analyses were used to assess prognostic factors.
3. Results
3.1 General Information
3.1.1 Age at onset
Among the 72 NMO patients, the youngest was 10 years old, the oldest was 77 years old, and the median age of onset was 33 years old. According to the data, the onset age of patients was divided into five age groups, and the high onset age of NMO patients with ON as the first episode was 25 to 38 years old (34.72%).
3.1.2 Gender and course of disease
Among 72 patients with NMO, the male to female ratio was 1:5.54(11/61). At the last follow-up, the median course of disease was 67 months (4-369), and the main characteristic was "relapse-remission".58 cases (85.29%) had a relapse-remission course, and the ratio of monophasic to relapse-remission was about 1:5.8.
3.2 Clinical Characteristics
3.2.1 Initial symptoms
Among the 72 patients with NMOON, 66 cases (91.67%) had THE onset of ON alone, 1 case had the complication of ON and myelitis,1 case had the complication of posterior polar zone syndrome, 2 cases had the complication of cerebral syndrome, and 2 cases had the complication of ON, posterior polar zone syndrome and cerebral syndrome. Right eye was involved in 34 cases (47.22%), left eye in 25 cases (34.72%), and bilateral simultaneous involvement in 13 cases (18.06%). The main symptoms of the patients were acute or subacute vision loss, including acute or subacute vision loss alone as the chief complaint in 31 cases, with eye distension in 1 case, with eye pain or rotational pain in 19 cases, with visual field defect or occlusion in 27 cases, with visual color abnormality in 2 cases.
3.2.2 Cause of disease
14 patients (19.44%) were accompanied by predisposing factors,including upper respiratory tract infection (8 cases), childbirth (2 cases), diarrhea (2 cases), fever (1 case) and trauma (1 case).
3.2.3 With autoimmune diseases
11 cases (15.28%) associated with autoimmune diseases, including 3 cases of sjogren's syndrome, 7 cases of thyroid disease (2 cases of hypothyroidism and thyroid function hyperfunction + 1 case of sjogren's syndrome, hypothyroidism and hashimoto's thyroiditis 1 case, hashimoto's thyroiditis 1 case), systemic lupus erythematosus(SLE) in 1 case, dermatomyositis + hashimoto's thyroiditis 1 case.
3.2.4 First sight
The first visual acuity of 59 eyes was less than 0.1, accounting for about 75.64%. Factors that may affect first-episode visual acuity were taken as independent variables, including gender of patients, age of onset, inducible factors, aqP4-igg antibody level and autoimmunity antibody level. First-episode visual acuity was an ordered four-category dependent variable, and ordered logistics regression analysis was conducted to screen pathogenic factors that may affect first-episode visual acuity. Visual acuity is divided into four grades according to clinical assessment: 0,1,2,3. The age of onset was 1 < 21; 2 21; Dummy variable of AQP4-igg was set as: 0: -; 1: + - +-; 2: + +; 3: +++, with 0 as the reference category;The model evaluation showed P =0.017 (χ2=13.819), indicating that after all variables were included, at least one variable was statistically significant and the modeling was successful (Table 1).After adjusting for other variables, the one-grade higher first-episode visual acuity of < 21 years was associated with a 392.7% increased risk compared with 21 years; For each grade of AQP4-igg serum,the risk of higher first visual acuity increased by 255.0%. Other independent variables had no statistical significance (Table 2).
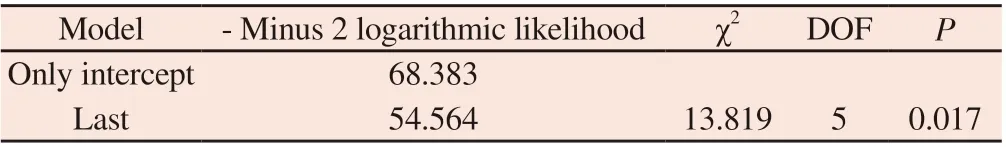
Tab 1 evaluation of ordered Logistics regression analysis model
Tab 2 Ordered logistic regression results of risk factors affecting first-episode visual acuity in NMO-ON patients
3.2.5 Vision during recovery (3 months)
The results of this study suggest that there is heterogeneity in the treatment methods of NMOON patients in China during acute episode, including intravenous glucocorticoid shock(different amount and course of treatment), oral glucocorticoid injection (different amount and course of treatment), postbulbous glucocorticoid injection, and no treatment. The visual acuity of 56 eyes (71.19%) recovered to 0.1, and only 20 eyes remained below 0.1. ON this basis, we evaluated the therapeutic effect of glucocorticoid in the acute phase of nmoon, and here we defined the definition of "glucocorticoid therapy": methylprednisolone ( 0.5 g)intravenous shock ≥ 3d + sequential reduction of oral glucocorticoid.The results indicated that 62 eyes of 54 patients received glucocorticoid treatment. Before treatment, 21 eyes (33.87%)had NLP, 17 eyes (27.42%) had LP, 5 eyes (8.06%) had HM, 4 eyes (6.45%) had CF, 3 eyes (4.84%) had 0.02 - 0.1, and 12 eyes(19.35%) had 0.1 or above. After treatment, 1 eye (1.61%) had NLP,1 eye (1.61%) had LP, 8 eyes (11.11%) had HM, 6 eyes (8.33%) had CF, 4 eyes (5.56%) had 0.02 - 0.1, and 42 eyes (58.33%) had 0.1 or above. χ2test showed a statistically significant difference in visual acuity distribution after and before glucocorticoid treatment (χ2=61.80, P < 0.000 1) (Table 3).

Tab 3 Comparison of visual acuity distribution before and after glucocorticoid treatment in NMO-ON patients [Number of eyes]
3.2.6 Frequency of ON attacks, annual recurrence rate and visual function at the last follow-up
By the time of follow-up, 44 (61.11%) NMO-ON patients were successively involved in both eyes. The median number of ON episodes was 2 (1-11), and the median number of second ON episodes was 3 months (1-156). The median duration of the overall second attack in NMO patients was 5.5 months (0-312 months), and the median number of total recurrences was 4 (1-23). The 1-year(ON) and 3-year (ON) recurrence rates were 0.56 (40/72), 0.74(53/72), and the median annual recurrence rate was 0.76 (0-4.8). Six patients had a 5-year delay in the first and second onset of ON.
In addition, we also calculated that the unilateral blindness rate of NMO-ON patients was about 48.61%, the median number of ON episodes caused by unilateral blindness was 2 times (1-5 times),and the median time of unilateral blindness was 3 months (1-228 months).
The median follow-up time of 72 patients with NMO-ON was 9.5 months (2-39 months). The visual function results of the last followup showed that 40 eyes (51.28%) were greater than 0.1, and 38 eyes(48.72%) were less than 0.1.
3.2.7 Involvement of other NMO sites
Of the 72 patients with NMO-ON, 53 (73.61%) had other nervous system involvement during the course of disease. Including spinal cord, brain, brainstem and medulla oblongata, the order of occurrence frequency was spinal cord (168 times) > medulla oblongata (36 times) > brainstem (8 times) > brain (1 time). The proportion of spinal cord injury was 61.11% (44 cases), medulla oblongata injury was 23.61% (17 cases), brain stem injury was 6.94% (5 cases), and brain injury was 1.39% (1 case).
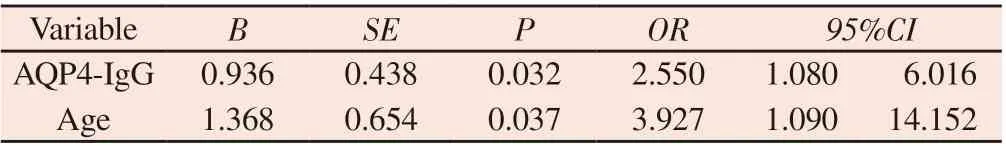
3.3 Laboratory examination
80% (48/60) of the patients were serologically positive for AQP4-igg (9 patients were strongly positive 3+) and serologically negative for 12 patients. We classified aqP4-igg antibody status (positive or negative) and compared the general information and clinical characteristics of the patients. The detailed results were shown in Table 4. The median age of NMO-ON onset was 22 years (13-62 years) in AQP4-igg-positive patients, and 33 years (10-77 years)in AQP4-Igg-negative patients, the difference was statistically significant (P < 0.05).
Three patients (25%) were serologically positive for MOG-igg. In addition, 18 patients (25%) were found to be co-positive for other autoimmune antibodies. Among them, 14 patients showed positive ANA antibody, 5 patients showed positive anti-RO52 antibody,4 patients showed positive anti-SSA antibody, 2 patients showed positive anti-SSB antibody, and 1 patient showed positive antithyroid peroxidase antibody, anti-RNP antibody, anti-AHA antibody,anti-mitochondrial antibody, and anti-merosite antibody.
3.4 Imaging Features
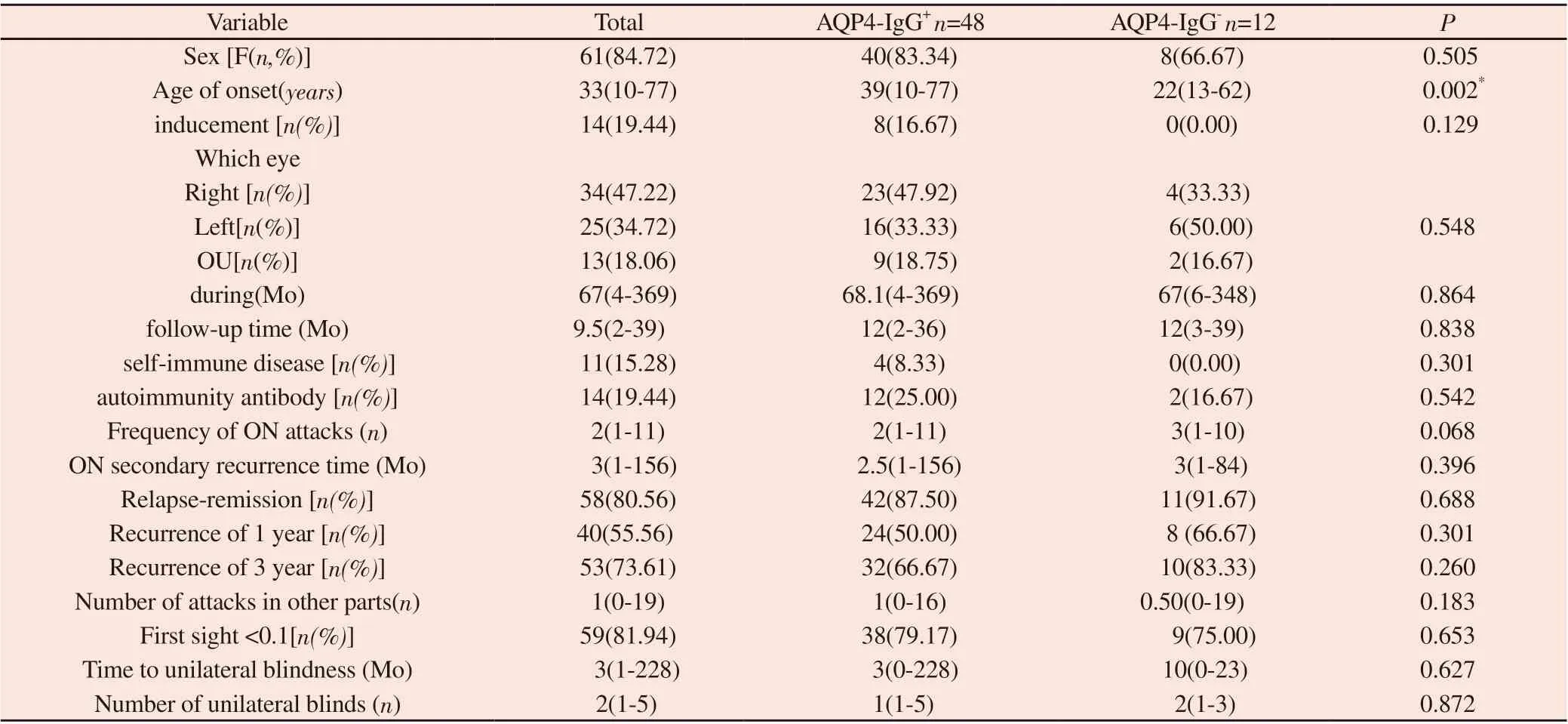
Orbital MRI examination of 23 cases of NMO-ON showed that NMO-ON mostly involved the posterior optic path, and the length of the lesions was more than half of the optic nerve, which could reach the optic chiasma and other parts. In the acute stage, the main manifestations were thickening and swelling of optic nerve, high signal on T2WI and gadolinium enhancement on T1WI, and blurred boundary, as shown in Figure 1. In chronic stage, tapering and atrophy of the optic nerve can be seen, and the "dual track sign" can be seen in typical cases, as shown in Figure 1A.MRI results of 53 patients (73.61%) showed involvement of other nervous systems, the spinal cord (48 cases, 90.57%) was the most common site of the disease, and the medulla oblong (20 cases,37.74%) was the most frequently involved site of the brain (Figure 2). Forty-five patients (84.91%) had myelopathy with 3 cones,and spinal cord swelling in the lesion area was observed in the acute stage, which showed specular or patchy enhancement after enhancement, usually in strip-like fusion, and sometimes in linear enhancement (Figure 2). Spinal cord atrophy, intermittent long T2 signal, and even cavity formation without enhancement can be seen in remission or recovery. In the whole course of the disease, 47.17%(25/53) had concurrent or successive cervical and thoracic lesions(FIG. 2B and C). 30.19% (16/53) had only cervical spinal cord lesions (Figure 2A); 22.64% (12/53) only involved the thoracic pulp(FIG. 2D); No sacral or lumbar involvement was observed.
Tab 4 Comparison of general data and clinical characteristics between AQP4-IgG positive and negative patients(n=72)

Fig 1 Typical MRI findings of orbit in NMO-ON patients
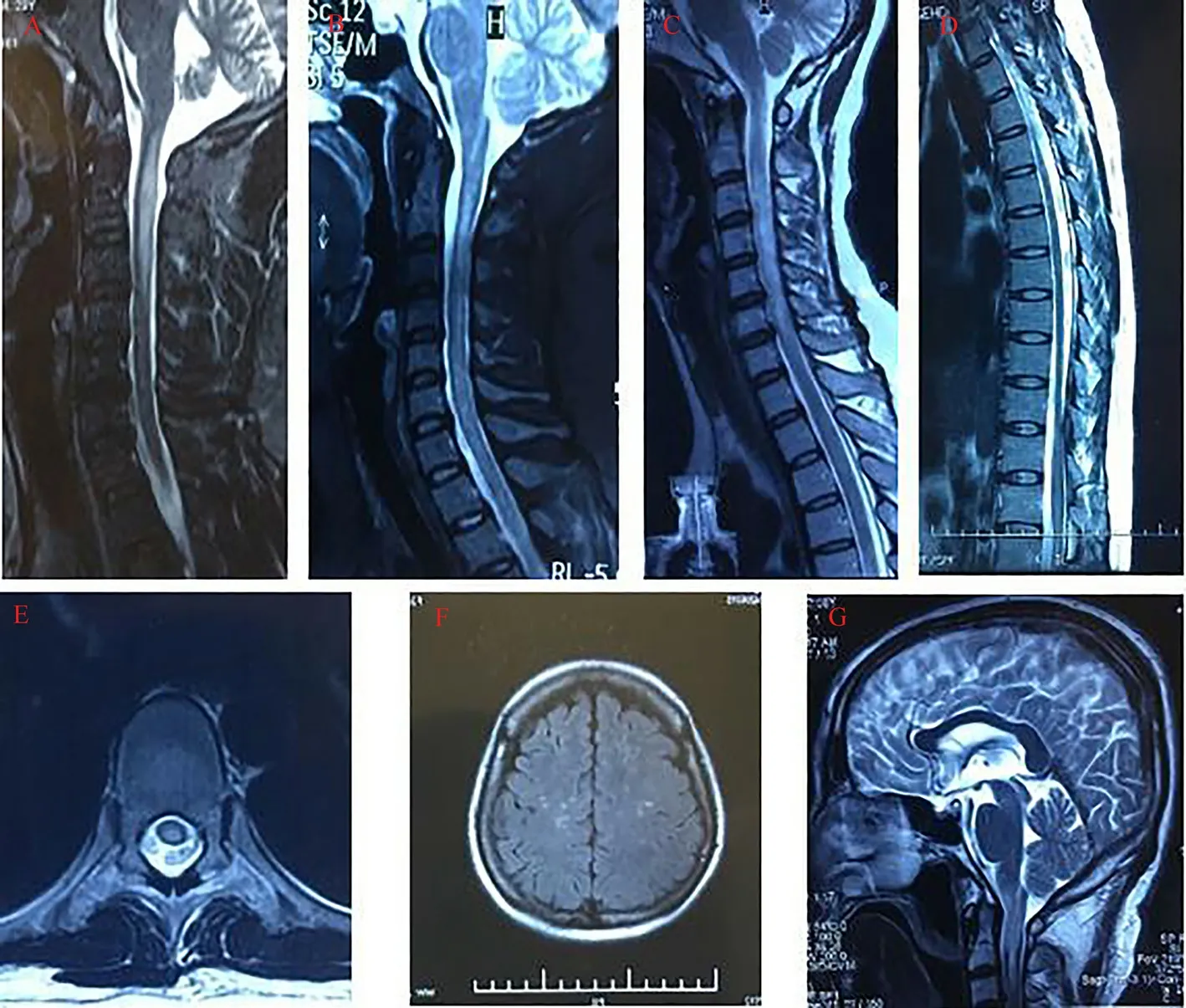
Fig 2 Involvement of other nervous system sites in NMO-ON patients
4. Discussion
At present, there is a lack of literature data summarizing the clinical pathogenesis of NMO patients from the perspective of optic nerve involvement. In this study, 72 cases of ON were included as the first clinical manifestation among 159 patients with NMO,and the results showed that ON alone accounted for about 91.67%of the onset of the disease, and unilateral optic nerve involvement accounted for 91.94%, which is worthy of in-depth clinical study and promoting the understanding of the immune pathogenesis of the disease. Foreign studies have pointed out that in the long course of disease, NMO patients are prone to bilateral optic nerve involvement and often show a relapse process, resulting in poor long-term prognosis of visual function [1]. This was similar to the results of our study, the median course of disease of 68 patients was 67 months (5.58 years), bilateral optic nerve involvement was successively involved in 61.11% of NMO patients, and recurrence was observed in 85.29% of NMO patients, with a single-phase to recurrence ratio of about 1:5.8. At the same time, our study also showed similar results with previous studies in terms of aqP4-igg serological status, female dominance, and age at first onset in each affected eye [8-13]. More importantly, we found that the onset age of AQP4-igg-negative NMO-ON patients was younger than that of AQP4-igg-positive patients. 15.28% of NMO-ON patients were associated with systemic autoimmune diseases, which was slightly higher than previous foreign reports. Sjogren's syndrome and thyroid diseases (hyperthyroidism, hypothyroidism and Hashimoto's thyroiditis) were most commonly associated with NMO-ON. These findings will contribute to further understanding of the pathogenesis of NMO-ON. Related studies have reported the existence of AQP4 in thyroid follicular cells [14], and the common epitope antigens of aquaporin 5 in salivary glands and AQP4 in CNS [15]. 25% of NMOON patients were serologically associated with positive systemic immune antibodies, the most common being ANA antibodies,which was consistent with previous literature reports [16]. The visual function of PATIENTS with NMOON is often accompanied by sharp visual impairment accompanied by pain of eye movement or visual field defect, abnormal color vision, etc. Our study also verified this point, 59 eyes (75.64%) had visual acuity less than 0.1 in the first attack, and 56 eyes (71.19%) had visual acuity 0.1 in the recovery period (3 months) after the first attack, but this figure was lower than foreign research reports [8,11], which may be consistent with the medical level of different regions in China. The result of the difference in treatment plan of patients. We, in turn, may be associated with patients with first onset vision impact factors, an orderly logistic regression analysis, the results suggest AQP4 - IgG levels and the onset of age are independent risk factors influence the starting vision (table 2), especially the onset age, can see the first sight with the patient significantly associated with the degree of combat, combined with the specific clinical data can be obtained,Early onset (< 21 years old) can predict the severity of the first visual impairment in NMO patients, which is consistent with the data just published abroad [17].
Relapse is a major feature in the course of NMO-ON patients, but there are few literature reports about the onset of ON, the impact ON vision and the outcome of visual function in NMO patients at home and abroad. Our results suggest that by the last follow-up, the median number of ON episodes was 2, and the median time of the second episode of ON was 3 months. NMO patients had an overall median time of a second episode of 5.5 months and a median total number of relapses of 4 months. In addition, we also found that the unilateral blindness rate of NMO-ON patients was about 48.61%, the median number of ON episodes caused by unilateral blindness was 2, and the median time of unilateral blindness was 3 months. These data will further provide support for patients to formulate treatment plans and explain clinical outcomes.
The onset of ON and myelitis can occur simultaneously but usually in succession [18,19]. The onset interval between myelitis and ON can be very long, ranging from a few months to decades [20,21].Our study adds to this data. In the acute stage of the first onset of NMO-ON, only 8.33% patients had involvement of the nervous system other than the optic nerve, but in the subsequent course of the disease, 53 patients (73.61%) had involvement of other nervous systems. Including spinal cord (most common), brain, brainstem,medulla oblongata, etc. This is similar to previous reports in that the frequency of spinal cord injury observed in this study (61.11%) falls in the middle of the results observed previously (36-63%)[22-24].The frequency of other recurrence types was the same as in previous studies, and recurrence of intracranial or other brain features was not common in NMO [24]. Orbital MRI examination of 23 cases of NMO-ON showed that NMO-ON mostly involved the posterior optic path, and the length of the lesions was more than half of the optic nerve, which could reach the optic chiasma and other parts. These radiological findings support the widespread longitudinal changes of the retrobulbous optic nerve commonly observed clinically in NMOON.
Relevant studies suggest that NMO-ON patients have poor visual impairment recovery even after receiving the above conventional treatment, and 60% of patients have at least one eye amaurosis or walking disorder within 7 to 8 years after onset [25,26]. Our final follow-up visual function results also supported this view, with about half (48.72%) of NMO patients having visual acuity less than 0.1. This result is slightly lower than the previous report that 50-70% of PATIENTS with NMO-ON have at least one eye final visual acuity ≤0.1[25-30], which may be related to the improvement of visual function of patients by actively treating NMO-induced optic atrophy with acupuncture combined with Traditional Chinese medicine in some patients.
In conclusion, this study further retrospectively summarized and analyzed the clinical data of 72 patients with NMO-ON using ON as the entry point. The acute onset of NMO-ON poses a great threat to patients' visual function, and most of them are accompanied by multiple relapses and low or even blinding visual function outcomes.The spinal cord is most frequently involved in the recurrent course of the disease. For NMO patients with ON as the onset of disease,early serological aqP4-igg antibody or MOG-igg antibody detection,orbital and other nervous system MRI examinations are often helpful for rapid diagnosis of the disease and the formulation of standard,long-term treatment plan, to prevent the recurrence of the disease and the resulting blindness and disability. These data not only provide reference for guiding the diagnosis and treatment of patients and predicting clinical outcomes, but also reflect the urgency of rapid and correct diagnosis and standardized treatment of NMO-ON.
Authors' contribution:
Han Meng-yu, Qin Ya-li, Ma Chuan-zheng: Collected clinical data of patients and collated data of articles, made statistics and wrote articles; Jiao Yu-juan, Jiao Jin-song, Jin Ming: Responsible for patient diagnosis, treatment plan formulation, etc.
All authors declare no conflict of interest.
 Journal of Hainan Medical College2022年22期
Journal of Hainan Medical College2022年22期
- Journal of Hainan Medical College的其它文章
- Research advances in functional heartburn based on Rome Ⅳ criteria
- Research progress on modern pharmacological action of Radix bupleuri
- Tanreqing injection auxiliary in the treatment of heart failure with pulmonary infection: A systematic review
- Mechanism of total flavonoids in the treatment of rheumatoid arthritis based on network pharmacology
- Application of SOAT1 combined with multiple markers in the auxiliary diagnosis of hepatocellular carcinoma
- Study on the relationship between psoriasis vulgaris and GC gene in Hainan Han nationality based on target gene capture sequencing
