Vestibular function of pediatric patients with sudden sensorineural hearing loss: based on vertigo symptom and vestibular function testing
an-Hong Li · Bing Liu · Yang aYng , · Min Chen · Wei Liu · Jian-Bo Shao · Xiao Zhang · Jie Zhang ·Xin Ni ,
Abstract
Keywords Prognosis; sudden sensorineural hearing loss · Vertigo · Vestibular function tests
Introduction
Sudden sensorineural hearing loss (SSHL) is clinically characterized by rapid onset of sensorineural hearing loss with hearing threshold of higher than 30 dB at three contiguous audiometric frequencies over the course of 3 days [ 1].Incidence of pediatric SSHL is relatively rare, with SSHL patients under 18 years of age comprising only 6.6% of all SSHL patients [ 2]. In spite of the low incidence of SSHL,it is known that several key differences distinguish children from adolescents with SSHL [ 3]. Nevertheless, few etiologic and prognostic studies have been focused solely on pediatric populations. Thus, at the present time, more researches should be carried out for better understanding of pediatric SSHL clinical characteristics towards optimization of treatments and identification of useful prognostic indicators [ 4].
Although SSHL appears to involve abnormal cochlear function, vestibular disturbances also may contribute to the disorder [ 5]. Generally, 30-60% of patients with SSHL present with vertigo, while 30%-80% present with abnormal vestibular function test results [ 6, 7]. Notably, previous studies have reported that vestibular functional anomalies had prognostic value for predicting SSHL patient outcomes;however, such studies were conducted in adults [ 8].
Several vestibular test methods have been used recently to diagnose patients suffering from SSHL; however, vestibular function testing requires a long testing period and will bring discomfort experiences, so such tests are unsuitable for use in diagnosing pediatric patients. Nevertheless,vestibular function tests provide objective vestibular damage assessment tools that can greatly facilitate identification of SSHL-associated vestibulocochlear lesion patterns and mechanistic pathways underlying SSHL [ 9]. By contrast,vertigo symptoms-based information collected from children is generally based on subjective data (feelings); although this information is easy to obtain, it is of questionable diagnostic value. Therefore, additional research is needed to determine whether pediatric SSHL patient symptoms assessments have any diagnostic or prognostic value, while identifying supplemental vestibular function tests for use as needed when symptoms assessments are deemed clinically inadequate for guiding and monitoring patient treatment.
To address the issues described earlier, the present study was designed to evaluate the relationship between vestibular function and hearing threshold levels in children with SSHL and to also explore the appropriate application method of vertigo symptom and vestibular function tests.
Methods
Patients
A total of 30 pediatric patients diagnosed with SSHL were enrolled in this study. All patients had experienced suddenonset idiopathic unilateral sensorineural hearing loss; a condition defined as hearing loss of > 30 dB over three contiguous frequencies occurring within 3 days. Patients who presented with chronic otitis media, inner ear deformity and a history of surgery in the affected ear were excluded.
Initial evaluations, including symptoms assessment (vertigo, tinnitus, imbalance), physical examination, pure tone audiometry and vestibular function tests, were conducted before treatment initiation. Hearing threshold levels were evaluated once after one month of treatment. All data were fully anonymized before analyses were conducted, and this study was approved by the Institutional Review Board of our hospital.
Treatment protocols
Steroid-based treatment comprised of high-dose intravenous dexamethasone (0.3 mg/kg/day) was administered for 3 days followed by administration of oral prednisolone (1 mg/kg/day of initial dose, decreased every 2 days by 10 mg) for 10 days. Vasoactive drugs were also administered (ginkgo biloba extract) for 14-30 days [ 10].
Audiometry and hearing outcomes
Pure tone averages (PTA) were recorded by averaging hearing thresholds at frequencies of 500 Hz, 1000 Hz,2000 Hz, 4000 Hz, and 8000 Hz. Initial hearing threshold levels, as determined via air conduction, were stratified into four hearing loss severity levels: mild (PTA 20-39 dB), moderate (PTA 40-59 dB), severe (PTA 60-79 dB) and profound (PTA ≥ 80 dB).
One month after treatment, patients underwent PTA follow-up, and the hearing improvement was evaluated by Siegel's criteria as follows: complete recovery to a final hearing threshold level greater than 25 dB; partial recovery by more than 15 dB of gain or a final hearing level between 25 and 45 dB; slight improvement by greater than 15 dB of gain and a final hearing level lower than 45 dB; no improvement,less than 15 dB of gain and a final hearing level lower than75 dB. Patient recovery status was also described using a twograde classification scheme: recovery (complete, partial and slight recovery) and no recovery [ 11].
Vestibular function tests
All patients underwent a bithermal caloric test, while 11 patients were subjected to both ocular vestibular evoked myogenic potentials (o-VEMPs) and cervical vestibular evoked myogenic potentials (c-VEMPs) testing.
Bithermal caloric tests were performed by blowing air into the external auditory canal at 27 °C and 47 °C for 40 s. Using a nystagmography system, the maximum slow-phase velocity of evoked nystagmus was calculated automatically. Canal paresis (CP) was recorded as a percentage using Jonkee's formula: CP = 100 × (right side maximum slow-phase velocity - left side maximum slow-phase velocity)/(right side maximum slow-phase velocity + left side maximum slow-phase velocity). A CP of > 20% or an absence of amplitude was regarded as abnormal.
During c-VEMPs testing, the first positive and negative waves were recorded as p13 and n23, respectively, while the interaural amplitude difference ratio (IAD) was calculated as a percentage as follows: 100{(Au - Aa)/(Aa + Au)}in which Au is the p13-n23 amplitude on the unaffected side and Aa is the p13-n23 amplitude on the affected side.An interaural amplitude difference ratio (IAD) for c-VEMPs amplitude of greater than 20% or an absence of amplitude on either side was regarded as an abnormal c-VEMPs result.For o-VEMPs, the amplitude between first negative peak(n10) and the subsequent positive peak (p16) was measured from the contralateral eye. An IAD in o-VEMPs amplitude of higher than 20% or an absence of amplitude on either side was regarded as abnormal results [ 8].
Statistical analysis
Statistical analysis was performed using SPSS for Windows,version 22 (SPSS Inc, Chicago, IL, USA). TheMann-Whitneytest was used for comparing hearing thresholds between children with and without vertigo or between children with normal and abnormal caloric test results. The chi-test was used to compare recovery results between children with and without vertigo or between children with normal and abnormal caloric test results. To calculate cut-off values of hearing thresholds, ROC curves were used. A difference ofP< 0.05 was regarded as significant.
Results
All 30 pediatric patients enrolled in this study, of ages ranging from 5.9 to 13.0 years, presented with unilateral SSHL,which consists of 13 patients with hearing loss in left ear and 17 patients in right ear. Hearing impairments of all patients were relatively serious (Fig. 1) and 14 patients (46.6%)presented with profound hearing loss. More than half of patients experienced vertigo (60.0%) and tinnitus (86.7%),while abnormal caloric responses, o-VEMPs responses and o-VEMPs responses were also at high proportions (50.0%,81.8% and 81.8%, respectively). Of 18 children with vertigo, 12 children (66.7%) had abnormal caloric responses,a higher proportion than that of children without vertigo(66.7% vs 25%,P= 0.025). Using Siegel’s criteria of hearing outcomes, half of children (50.0%) exhibited no improvement at all, while 26.7% fully recovered.
Importantly, vestibular function was significantly associated with initial hearing thresholds of children with unilateral SSHL (Fig. 2). Initial hearing thresholds of children with vertigo were higher than thresholds of children without vertigo (92 dB vs 79 dB, respectively,P= 0.033).Initial hearing thresholds of children with abnormal caloric test results were higher than thresholds of children with normal caloric test results (93 dB vs 67 dB, respectively,P= 0.014).
To calculate hearing threshold cut-off values for vestibular function, ROC curve analysis was conducted (Fig. 2).Through ROC analysis, the Youden index was calculated followed by selection of sensitivity, specificity and cutoff values corresponding to the largest Youden index. For vertigo symptoms, the hearing threshold cut-off value was 86.000 dB HL (P< 0.05), and the area under the curve (AUC) was 0.708 with 95% confidence interval of 0.595-0.971. According to caloric test results, the hearing threshold cut-off value was 89.583 dB HL (P< 0.05),and AUC was 0.807 with 95% confidence interval of 0.625-0.989.
Notably, vestibular function of pediatric patients with unilateral SSHL was also significantly associated with patient outcomes (Fig. 3). Children with vertigo had lower recovery rates than children without vertigo (33% vs 75%,P= 0.025);Children with abnormal caloric test results had lower recovery rates than children with normal caloric test results (25%vs 73%,P= 0.039).
Discussion
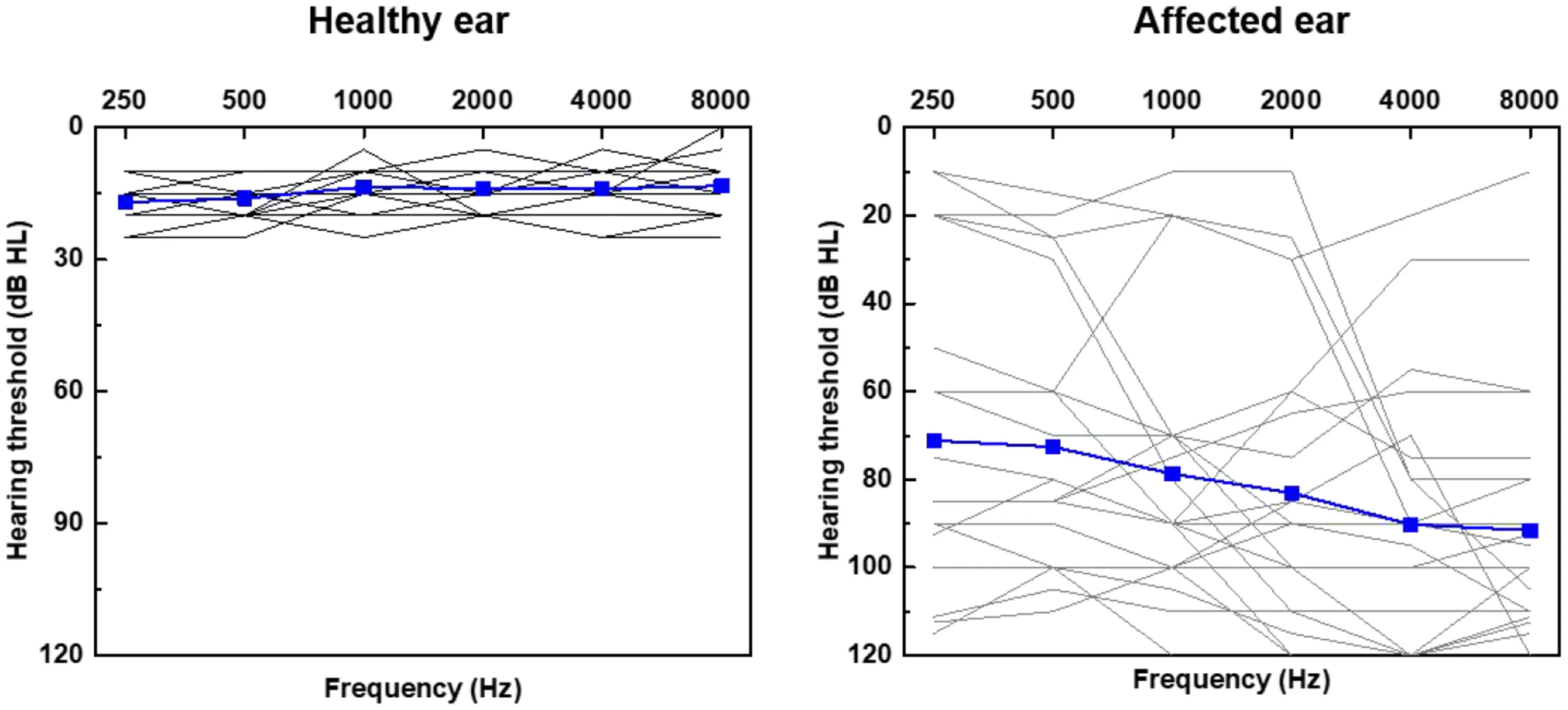
Fig. 1 Pure tone audiometric hearing thresholds for healthy ear and affected (hearing loss) ear. Gray lines represent individual patient thresholds,blue solid lines represent mean thresholds for the cohort
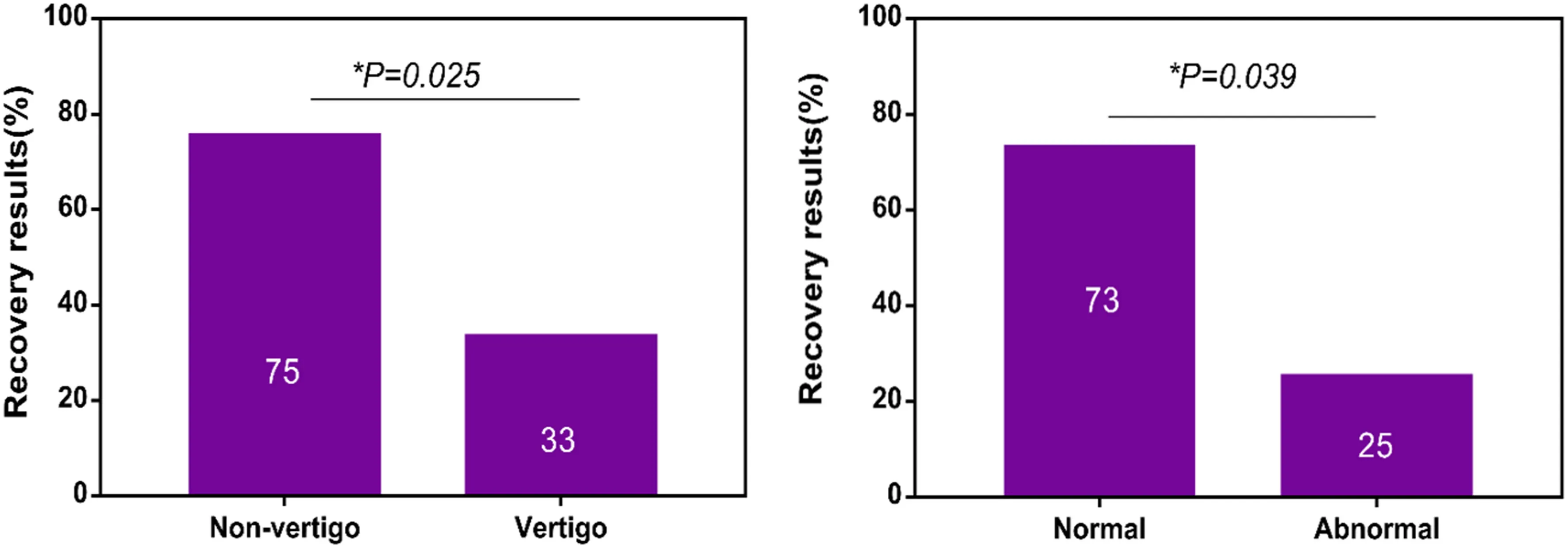
Fig. 3 Relationship of prognosis and vestibular function. Children with vertigo had lower recovery rates than children without vertigo ( P = 0.025); children with abnormal caloric test results had lower recovery rates than children with normal caloric test results( P = 0.039). *Significance was set at P < 0.05
In the pediatric patients with SSHL, the incidence of SSHL is low and evaluating vestibular function is very difficult,so few studies have been carried out focusing on vestibular function. To our knowledge, only one SSHL study in the pediatric population has been reported. In the other study,vestibular function assessment was based largely on electronystagmography results [ 12]. We found that additional assessment tests are needed to address clinical needs of pediatric SSHL patients.
We found high rates of vertigo symptoms and abnormal vestibular function, which aligns with previous research results reported in the literature [ 13]. Owing to the unreliability of symptoms-based information relayed by the children, vertigo symptoms were not often reported in enough detail to permit classification of vertigo symptoms into more than one category. Importantly, proportion of patients with abnormal VEMPs results exceeded that of patients with abnormal caloric test results. Intriguingly, subjective vertigo symptoms and objective abnormal vestibular function test results were consistent: most patients with vertigo also exhibited abnormal caloric responses. Thus, for children who could not easily speak out symptoms clearly, objective vestibular function tests could provide information to assess discomfort levels experienced by those patients.
Importantly, different SSHL etiologies have been shown to induce different distribution patterns of damage within vestibular organs. In a study by Iwasaki, the utricle was most susceptible to damage in SSHL [ 14]. However, higher rates of lesion formation in the semicircular canal have also been reported [ 15]. Thus, no consensus currently exists regarding vestibular organ lesion characteristics in SSHL patients, warranting additional clinical vestibular function studies, basic pathological studies, and animal experiments to address this issue.
In our work symptoms of vertigo were associated with initial hearing impairment severity: The more severe the initial hearing loss, the more frequently patients complained of vertigo. In addition to vertigo symptoms, vestibular function was also associated with initial hearing status: The more severe the initial hearing loss, the greater the likelihood that vestibular organs were damaged. Researchers have speculated that vestibular damage is etiologically tied to cochlear damage. According to inner ear anatomic characteristics,blood flow to both cochlear and vestibular organs originates in the internal auditory artery, while both vestibular and cochlear nerves reside within the internal auditory canal[ 16]. Although etiological and mechanistic factors underlying SSHL development in children differ from corresponding factors underlying SSHL disease in adults, vestibular and cochlear prone to be joint damaged regardless of vascular disease and viral infection [ 17].
Because vestibular function was also related to initial hearing threshold level in this study, we calculated hearing threshold cut-off values according to vestibular functions,a task that had never been reported. This cut-off value is of great significance for pediatric patients for several reasons.First, communication of discomfort by pediatric patients yields relatively unreliable information that tends to lead to underreporting of discomfort. Second, helpful vestibular function tests are not readily available for use in pediatric patients. Thus, it is commendable that hearing threshold could predict vestibular function. Here, threshold cut-offvalue was about 90 dB HL, the cut-off value commonly used in audiology for assessing hearing loss [ 18], and was calculated for children with profound SSHL, associated with serious vestibular dysfunction requiring medical attention.However, owing to the small sample size in this study, cutoff values determined here require further verification.
In addition to initial hearing threshold levels, vertigo symptoms and vestibular function tests are helpful for formulating pediatric SSHL patient prognoses, as has been verified in adults in numerous reports [ 8, 19]. Due to poor pediatric patient, appropriate methods to predict prognosis must be considered for pediatric population. Acquisition of symptoms is more appropriate than examinations, which would cause discomfort and poor coordination. However,vestibular function tests could infer objective vestibular function situation and could help infer pathology and etiology of SSHL [ 20]. Therefore, we recommend that vertigo symptoms be predominantly used to initially prognosis pediatric SSHL cases, with vestibular function tests conducted as supplementary tests as needed.
This study had several limitations. Due to poor patient tolerance of vestibular function tests, some children failed to complete VEMPs examinations and thus could not be comprehensively assessed for vestibular function. In addition, the small sample size and short follow-up period may have diminished the strength of our findings. More research efforts should be taken to explore vestibular function of pediatric patients with SSHL which will lead to qualitatively improved diagnostic and prognostic tools and treatments for these patients.
In conclusion, pediatric SSHL patients are prone to vestibular function impairment. For these patients, pediatricians should focus on treating both cochlear disorders as well vestibular system impairments, especially since the vestibular system plays a huge role in children's growth and development. Importantly, diagnosing vestibular disorders in the pediatric population should be taken seriously and should be systematically based on both vertigo symptoms and vestibular assessments to assess disease severity and predict patient outcomes.
Acknowledgements The authors would like to thank clinical vestibular center with gathering of data for this study.
Author contributions YHL is responsible for conceptualization, formal analysis, methodology, and original draft writing; BL is responsible for data curation, methodology, and original draft writing; YY and WL are responsible for investigation. MC is responsible for resources.JBS is responsible for software; XZ is responsible for validation; JZ is responsible for conceptualization, project administration, and review and editing; XN is responsible for project administration. YHL and BL contributed equally to this paper.
Funding This study was supported by the Special Fund of the Pediatric Medical Coordinated Development Center of Beijing Hospitals Authority, No. XTYB201828 and Beijing Hospitals Authority’ Ascent Plan, No. DFL20191201.
Data availability statement The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Compliance with ethical standards
Conflict of interest The authors declare that they have no conflict of interest.
Ethical approval and informed consent This study was approved by the University Hospitals institutional review board with a waiver of informed consent. None of the authors serves as a current Editorial Team member for this journal.
 World Journal of Pediatrics2021年6期
World Journal of Pediatrics2021年6期
- World Journal of Pediatrics的其它文章
- Haploidentical hematopoietic stem cell transplantation for pediatric patients with chronic active Epstein-Barr virus infection:a retrospective analysis of a single center
- Treatment of pediatric mild persistent asthma with low-dose budesonide inhalation suspension vs. montelukast in China
- Comparison of clinical outcomes between unrelated single umbilical cord blood and “ex-vivo” T-cell depleted haploidentical transplantation in children with hematological malignancies
- Muscle strength and its association with cardiometabolic variables in adolescents: does the expression of muscle strength values matter?
- Consensus statement on the epidemiology, diagnosis, prevention,and management of cow's milk protein allergy in the Middle East:a modified Delphi-based study
- Evaluation of a new frequency-volume chart for children with primary monosymptomatic nocturnal enuresis: a prospective, comparative study
