A comparison of maternal fear of childbirth,labor pain intensity and intrapartum analgesic consumption between primiparas and multiparas:A cross-sectional study
Yongfng Dng ,Yn Lin ,Liyun Yng ,Qiuxi Ling ,Biling Fu ,Huixin Li ,Huizhu Zhng ,Yn Liu
a Department of High-Risk Obstetric,Guangzhou Women and Children’s Medical Center,Guangzhou Medical University,Guangzhou,China
b Department of Nursing Administrative Office,Guangzhou Women and Children’s Medical Center,Guangzhou Medical University,Guangzhou,China
c Department of Gynaecology and Obstetrics,Guangzhou Women and Children’s Medical Center,Guangzhou Medical University,Guangzhou,China
d Institute of Pediatrics,Guangzhou Women and Children’s Medical Center,Guangzhou Medical University,Guangzhou,China
e Delivery and Labor Room,Guangzhou Women and Children’s Medical Center,Guangzhou Medical University,Guangzhou,China
Keywords:Epidural analgesia Fear Labor pain Obstetrics and gynecology department of the hospital Parity Parturition
ABSTRACT Objectives:To describe and compare fear of childbirth and in-labor pain intensity between primiparas and multiparas and explore the association between the amount of actual pain relief and fear of childbirth.Methods:A convenience sampling method was used.A total of 260 women undergoing spontaneous or induced labor,including 97 primiparas and 163 multiparas,were recruited in a large academic specialized hospital in Guangzhou,China,from February 2018 to August 2019.The clinical data of maternal and neonatal were extracted from a structured electronic medical record system.Other demographic information,such as employment and family monthly income,was collected by a questionnaire.The Numeric Rating Scale (NRS) and the Chinese version of the Childbirth Attitude Questionnaire(C-CAQ)were applied to assess maternal in-labor pain intensity and fear of childbirth.The analgesic consumption and the frequency of manual boluses as rescue analgesia were stored and collected from the analgesia pump.Results:Eighty-two (84.5%) primiparas and ninety-nine (60.7%) multiparas received epidural analgesia(P <0.001).In the epidural subgroup,the primiparous average fear of childbirth (36.46 ± 10.93) was higher than that of the multiparas (32.06 ± 10.23) (P=0.007).However,multiparas reported more intense in-labor pain[8.0(8.0,9.0)vs.8.0(7.0,8.0)],had more successful manual boluses per hour [2.68(1.65,3.85)vs.1.77(0.90,2.47)],more hourly analgesic consumption[23.00(16.00,28.25)vs.17.24(11.52,21.36) mL] and more average analgesic consumption [0.35 (0.24,0.45) vs.0.26 (0.19,0.35) mL/(h·kg)]than the primiparas(P<0.05).Spearman’s correlation analysis showed that the maximum in-labor pain was weakly positively correlated with fear of childbirth (r=0.09) (P <0.05),hourly analgesic consumption (r=0.16) (P <0.01) and average analgesic consumption (r=0.17) (P <0.05).No statistically significant association was uncovered between analgesic consumption and maternal fear of childbirth.Conclusions:Fear of childbirth is a potential predictor of labor pain intensity.Further study is needed to explore its role and value in pain management during delivery.Parity is not a determinant of pain relief use and should not be a preconceived preference of obstetric care team members to determine the distribution of epidural analgesia,especially when analgesia resources are insufficient.
What is known?
· Primiparas have a higher fear of birth than multiparas,are more sensitive to in-labor pain,and are more likely to ask for pain relief.
· A high level of childbirth fear is a potential influencing factor for laboring women who request pain relief.
· It is unclear how analgesic consumption is associated with childbirth fear.
What is new?
· In the epidural subgroup,the multiparas consumed more analgesics on average and had more successful manual boluses per hour than the primiparas.
· Fear of childbirth was not a strong predictor for pain,and parity was not a protective factor for multiparas in our study.
· Analgesic consumption was not proven to be associated with fear of childbirth.
1.Introduction
Currently,fear of childbirth(FOC)as a controversial concept has spawned a rich body of work[1];however,researchers and clinical participants have reached a consent that it does exist[2].Defined as a psychological disorder that some women may experience specific to giving birth [2],FOC consists of fear of not knowing and not planning for the unpredictable,fear of harm or stress to the baby,fear of the inability to cope with the pain,fear of potential harm to oneself during labor and the postnatal period,and so on[3,4].Even though research methods vary,it is a common condition with a prevalence of 6.3%-14.8% worldwide [1],and 6%-15% of women develop severe FOC,called tocophobia [5].While it is widely acknowledged that FOC negatively exerts effects on women before,during,and after birth,it may overshadow the whole pregnancy,leading to postpartum depression [6] and posttraumatic stress disorder (PTSD) [7].Further,more prolonged labor [8],stronger preferences for cesarean section [7,9],and greater labor pain [10]have been reported in women with FOC.
Previous studies have discussed a consistent relationship between FOC and labor pain and concluded that women with FOC were sensitive to pain.The greater the fear of delivery was,the greater the labor pain[10],and the more frequently pain relief was requested [11].The maternal self-rating pain score by the visual analog scale (VAS) or numeric rating scale (NRS) determines pain relief administration for women in labor in a clinical setting.Epidural analgesia is now considered to be the standard for pain relief during delivery.With the development of analgesia technology and the advent of a programmed intermittent epidural bolus technique[12],women in labor can receive manual boluses as rescue analgesia whenever they feel more pain.Even when the block-out interval is set in place,analgesic consumption every hour and a manual bolus can reflect actual painful maternal experiences during labor[13,14].Therefore,it is reasonable to conclude that the more intense the labor pain,the more frequent analgesic and manual bolus consumption will be.
With labor pain being inevitable and intense during childbirth,women experience labor pain quite differently and are under physiological and psychological influences.Although no consistent conclusions have been drawn regarding on the differences between primiparous and multiparous labor pain perceptions [15-18],due to clinical experience and clinical prejudice,the thought that primiparous labor pain is more intense than that of multiparas has infiltrated into health care providers’mindset[19].This expectation is indeed convincing in some studies [15,20,21].Concerning childbirth fear,parity is as well reported to be a greatly significant factor in the severity of childbirth fear [22].Influential factors of levels of childbirth fear have been reported to encompass trait anxiety,state anxiety,age,and a previous experience of miscarriage[23].In addition,depression symptoms,decisional conflict,low self-efficacy,and lack of social support predicted high and severe fear levels as well [24,25].The results,conversely,acted within a spectrum of consent and dissent as follows.Alehagen et al.[19]reported that primiparas had an increased risk of higher levels of fear during the early stage of active labor compared with multiparas.Similar findings were reported in studies by Toohill J.et al.’s[25] and Rouhe H.et al.’s [26] studies,in which severe FOC was more common in nulliparous women than in parous women.Nonetheless,one recent systematic review concluded that nulliparous and parous women had similar levels of birth fear for various reasons [24].Nulliparous women were mainly afraid of not knowing what they might experience intolerable pain during childbirth or of negative birth stories told by others who passed on frightening information or more mood-related problems.In contrast,multiparous women would develop a fear of delivery;and the particular reason for this circumstance is a previous negative experience of childbirth [24].
What is of paramount concern in this study,on the other hand,is that previous findings failed to provide specific and objective evidence to convince the association of childbirth fear with actual maternal needs for pain relief.They did not provide enough evidence to prove how the severity of fear was associated with the amount of pain relief consumed by women in labor,which would increase with the more labor pain they experienced.Moreover,FOC,regarded as a psychological variable,was primarily measured before[8,9,23,27-29] or after [6] childbirth or in both periods simultaneously in the same study[10,11].Few studies address the effects of FOC on women during labor.Even though tocophobia refers to the fear of both childbirth and pregnancy,the symptoms of tocophobia seemed to be more associated with delivery than pregnancy[5].
In contrast,less evidence was found on tocophobia during labor.The question to be answered is whether fear of birth vanishes,or is it nonexistent during labor? Even though researchers insist that women in labor suffered from fear of childbirth [19,30],relevant studies are scarce.Hence,this study aimed to test three hypotheses:1) a greater fear of childbirth during labor will be reported in primiparas;2) primiparous women will require more analgesic consumption and request more manual boluses for rescue analgesia,and 3)fear of childbirth is positively correlated with the amount of pain relief needed by women in labor.
2.Methods
2.1.Study design and participants
This is a cross-sectional study conducted from February 2018 to August 2019 in a large academic specialized hospital.The annual number of births was approximately 30,000 in recent years,ranking first in Guangdong Province.Women undergoing spontaneous or induced labor were recruited by convenient sampling immediately after being admitted to the delivery and labor room at the onset of the labor process.The inclusion criteria were 20-to 45-year-old women with singleton cephalic term pregnancies (gestational age ≥37 weeks) without severe pregnancy complications,such as heart disease,uncontrolled hypertension,and gestational diabetes mellitus.Women who had a scarred uterus underwent artificial insemination for the current pregnancy,had a history of a significant psychiatric disorder,could not read and write Chinese,and had any contraindication to epidural analgesia were excluded.Three midwives and two nursing assistants in the labor and delivery room were trained to be investigators.Laboring women who were once transferred to the delivery room and agreed to participate in this study were invited to rate their pain and fill out the required questionnaires to report their feelings about childbirth.
2.2.Measurements
2.2.1.Sociodemographic and obstetrical characteristics
Demographic and obstetrical characteristics were retrieved from the structured electronic medical records system,including maternal age,body mass index (BMI),gravidity,gestational week,labor duration,neonatal gender,birth weight,length,etc.In addition,a questionnaire was used to survey women’s occupation and their family monthly income per capita.
2.2.2.Fear of childbirth
Fear of childbirth was self-reported once women were admitted to the delivery room and before pain relief was administered if needed.The Chinese version of the Childbirth Attitude Questionnaire(C-CAQ)[31]was applied to assess maternal fear of childbirth.This questionnaire was improved by Tanglakmankhong[32],where footholds are on the original English version validated by Lowe[33].Then the questionnaire was translated and adapted by Wei et al.[31].The C-CAQ comprises 16 items with a Likert response scale of 1-4 and sum scores that range from 16 to 64,with higher scores(≥27) representing more elevated levels of fear.Four dimensions were encompassed in the C-CAQ,namely,fear of baby safety(FBS),fear of losing control (FLC),fear of labor pain (FLP),and fear of the environment(FE)during labor.Wei’s study reported good internal consistency reliability and validity for the C-CAQ [31] with 351 pregnant women from 28 to 34 gestational weeks.The Cronbach’s α coefficient was 0.910 for the total scale and 0.678-0.853 for the dimensions.The test-retest reliability for the full scale and each dimension were 0.803 and 0.812-0.921,respectively.In this study,the Cronbach’s α coefficient for each dimension's total scale was 0.910 and 0.711,0.850,0.829,and 0.650,respectively.
2.2.3.Labor pain
A numerical rating scale(NRS)of 0-10 was adopted to evaluate maternal pain,with 0 describing no labor pain and 10 describing the most severe labor pain.The higher the score,the more severe the labor pain is.Women were asked to report their labor pain score whenever they felt pain until labor was completed,and the maximum in-labor pain(P0) was recorded.In addition,those with epidural analgesia were also invited to report the current pain intensity at the time that the epidural analgesia was administered(P1),15 min(P2)after,and 30 min(P3)after its administration,and at the time of full dilation presented (P4).Two midwives were trained to record maternal pain scores.Pain scores were used in the final analyses.
2.2.4.Epidural anesthesia administration
The anesthesiologists initiated patient-controlled epidural anesthesia (PCEA) for women who requested it,and the cervical dilation was ≥2 cm for primiparas or ≥1 cm for multiparas.PCEA was administered following an anesthesia protocol routinely used in our medical center.PCEA was administered with 10 mL of 0.1%bupivacaine with 5 μg sufentanil as the first dose.A continuous background infusion (6 mL/h of a mixture of 0.0625% bupivacaine and 0.4 μg/mL sufentanil) was then set in place.If the background infusion was insufficient to relieve the pain,women could have a manual bolus of 6 mL at a lockout interval of 15 min for rescue analgesia.After PCEA was administered,the anesthetist taught each woman how to control the pump and ensure that the woman had mastered the skills to use the pump when necessary.Then,the anesthetic pump was closed when the woman was fullly dilated as a routine clinical practice to avoid a prolonged second stage of labor,and whether to use epidural anesthetic during labor was treated as a dichotomous variable.The total epidural analgesic consumption and successful manual bolus from the implementation of epidural administration to full cervical dilation were recorded automatically by the anesthetic pump.Besides,three nursing assistants in the delivery room were trained to check the anesthetic pump and record the data manually.
2.3.Ethical and legal considerations
The institutional ethics review board at our medical center approved the study (NO.2019-33301).The study was conducted following the ethical guidelines of the Declaration of Helsinki of the World Medical Association.Written informed consents were obtained from all participants as soon as they arrived in the delivery and labor room.Data used in this study were anonymous,and no identifiable personal data of the patients were available for analysis.
2.4.Data analysis
Data were analyzed using SPSS software version 23.0 (IBM Company,Armonk,NY,USA).The internal consistency of the C-CAQ was assessed using Cronbach’s α coefficient.Descriptive analyses were conducted to determine the demographic,clinical,and psychological characteristics of the participants.Continuous variables are expressed as the mean±SD or median(P25,P75),depending on their distribution,and categorical variables are presented as frequencies (percentages).The disparities between primiparas and multiparas were compared with independent samples t-tests or Mann-Whitney tests for continuous variables and chi-square tests for categorical variables.Spearman's correlation analysis was used to show the association of childbirth fear,in-labor pain intensity,and analgesic consumption.
Power analysis was calculated using a Mann-Whitney test to test for noninferiority hypothesis with a significance level of 0.05.The means or medians of the sample were used for ‘mean1’ and‘mean2’.A sample size of 97 from the primiparas and 163 from the multiparas achieves >90.0% power to detect the difference in successful manual boluses per hour between the two groups(assumed SDs ≤2.0).For the volume of hourly consumed analgesics,the sample size achieves >85% power to reject the null hypothesis(assumed SDs ≤20.0).The sample size achieves >71.2% power for the average analgesic consumption to reject the null hypothesis(assumed SDs ≤0.3).However,the sample size achieves no more than 32.7% power to reject the null hypothesis for average FOC(assumed SDs ≤20.0).A sample size of 260 achieves 32.0%power to detect a correlation of 0.093 between the maximum in-labor pain and FOC.Power analysis was performed using NCSS PASS-11.
3.Results
3.1.Demographic and clinical characteristics
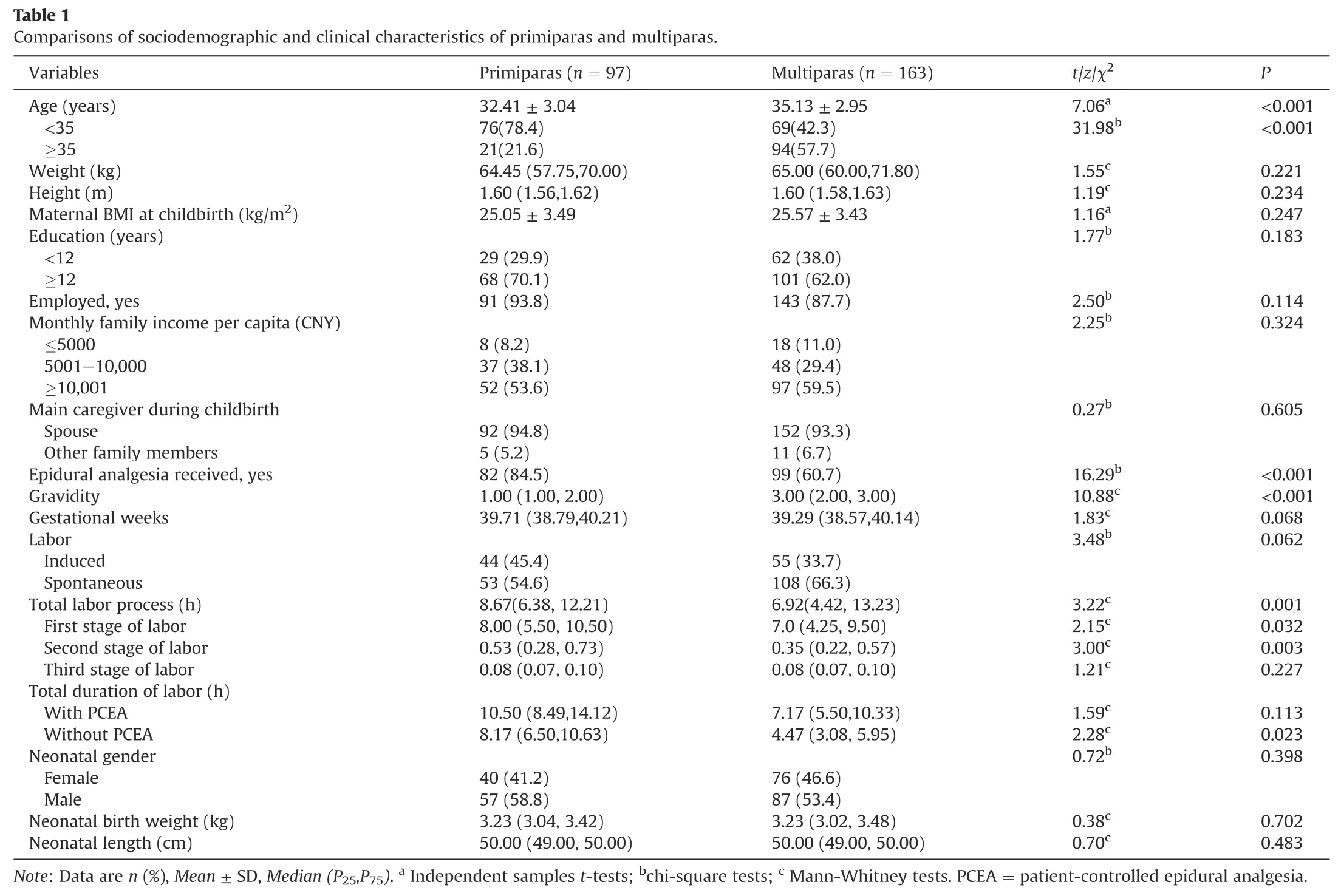
A total of 260 women,including 97 primiparas and 163 multiparas,were included in the final data analyses.A total of 44.2%(115/260)of the women were ≥35 years of age;of the women ≥35 years of age,more were multiparas than primiparas (57.7% vs.21.6%,P<0.001).The weight at childbirth was 64.45(57.75,70.00)kg for primiparas and 65.00 (60.00,71.80) kg for multiparas (P=0.221).The gravidity range was 1-6 for all participants,and the gravidity was 1.00 (1.00,2.00) for primiparas and 3.00 (2.00,3.00) for multiparas (P <0.001).Eighty-two (84.5%) primiparas and 99 (60.7%)multiparas received the PCEA (P <0.001) (Table 1).
3.2.Fear of childbirth and in-labor pain
The average FOC was 36.46 ± 10.93 for primiparas and
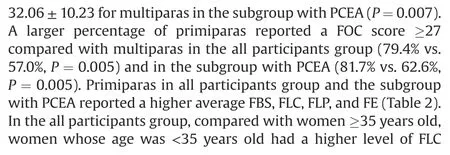
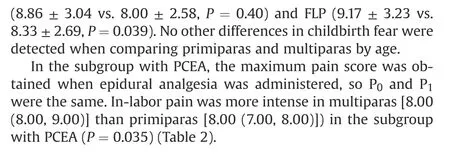
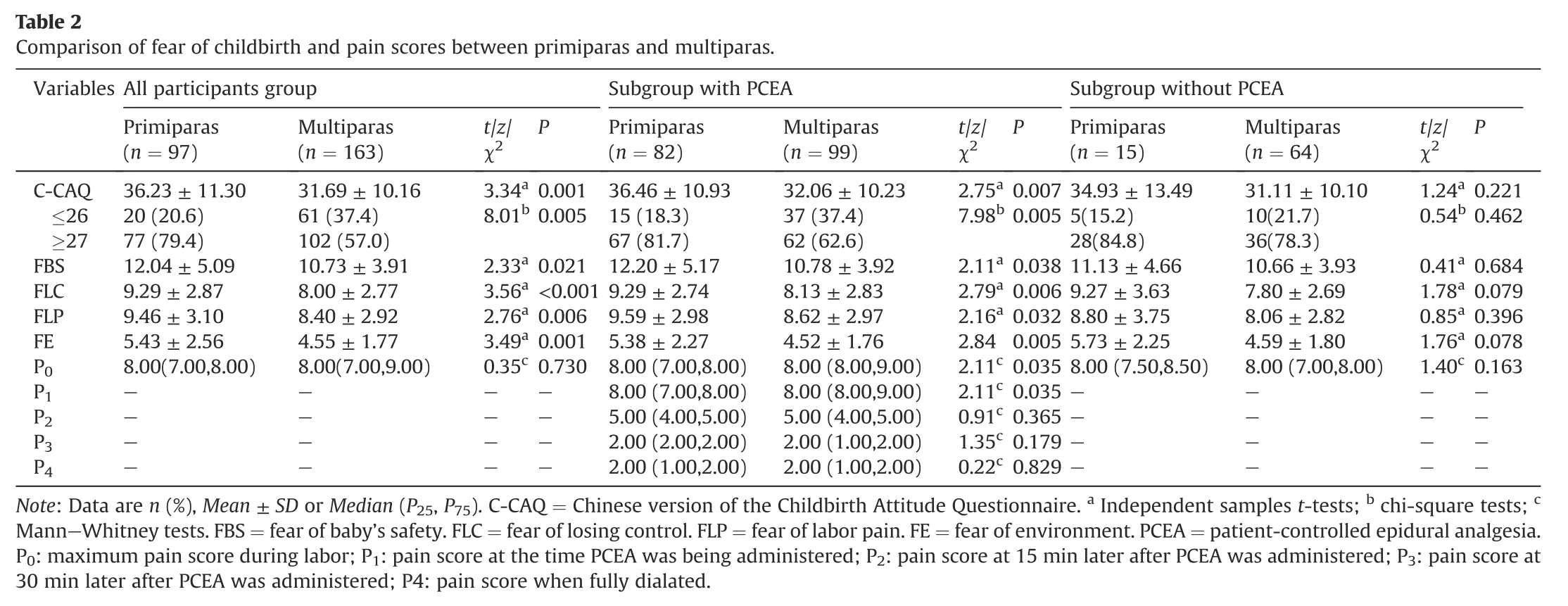
3.3.Pain relief and its association with fear of childbirth and inlabor pain
The duration of epidural analgesia was 8.00 (4.50,10.77) h for primiparas and 3.25 (1.93,6.23) h for multiparas (P <0.001).A similar percentage of primiparas and multiparas had manual boluses as rescue analgesia (91.5% vs.94.9%,P=0.348).Multiparas had 2.68 (1.65,3.85) successful manual boluses per hour,and primiparas had 1.77 (0.90,2.47) PCEA successful manual boluses per hour(P<0.001).To exclude the effects of weight and the duration of anesthesia,the average analgesic consumption was compared.The hourly analgesic consumption was 23.00(16.00,28.25)mL for multiparas and 17.24 (11.52,21.36) mL for primiparas (P <0.001).The average analgesic consumption was 0.35(0.24,0.45)mL/(h·kg)for multiparas and 0.26 (0.19,0.35) mL/(h·kg) for primiparas(P <0.001) (Table 3).Spearman’s correlation analysis showed an extremely weak positive correlation between the maximum inlabor pain score and the FOC score (r=0.09,P <0.05),hourly analgesic consumption (r=0.16,P <0.01) and average analgesic consumption(r=0.17,P<0.05)(Table 4).No statistically significant correlation was found between analgesic consumption and FOC.
4.Discussion
This cross-sectional study examined the differences in primiparous and multiparous childbirth fear,in-labor pain,and the amount of pain relief.The first hypothesis was proved that primiparas had a higher level of childbirth fear.However,a statistically significant difference in FOC between primiparas and multiparas was only discovered in the subgroup with PCEA but not among women without PCEA.Meanwhile,primiparas with PCEA failed to report higher self-rated maximum pain scores than multiparas.Likewise,they consumed less average analgesic consumption and had fewer PCEA successful manual boluses per hour than multiparas,which did not verify our second hypothesis.Last but not least,we failed to find evidence to prove the positive association of FOC with pain relief.
Regarding the relationship between childbirth fear and parity,our finding agrees with many previous studies [19,34-36] discussing childbirth fear and parity that showed primiparas reported higher FOC than multiparas.However,another published study revealed inconsistent findings regarding the differences between primiparas and multiparas[24].It is thought that since multiparas have experienced childbirth,they may be better prepared for subsequent childbirths.Thus,multiparas may have a lower risk of developing childbirth fear than primiparas.In contrast,previous delivery experiences,especially negative birth experiences,such as cesarean sections,episiotomies,and assisted deliveries,may equally increase the risk of multiparas developing birth fear of multiparas [24].Consequently,multiparas with previous bad childbirth experiences may as well have higher levels of fear than some primiparas in light of the effects of fear after birth.Resultedly,when we speak of childbirth fear,it is infelicitous to assume that primiparas will have higher levels of FOC than multiparas.Health care providers should remember that there are differences in these women that make them fearful.Additionally,younger age is still associated with childbirth fear,similar to the previous findings[23].
A greater FOC failed to predict more pain relief consumption in our study,which contrasts with the study that showed that fear of delivery during the early stage of labor predicted the amount of pain relief during the remaining phase of labor [19].Conversely,multiparas with a lower FOC consumed significantly more analgesics per hour and had more successful manual boluses per hour.This is not the first study to discover that fear failed to predict differences in the use of pain relief.One recently published study reported that women who feared childbirth during pregnancy requested pain relief more frequently than women without FOC during pregnancy,but the difference was not statistically significant [11].The reasons for this outcome are unknown.
Many studies have been published that fearful women request pain relief more frequently [11,42,43],whereas few have followed or observed real pain relief consumption in actual situations.Previous studies focusing on the relationship between childbirth fear and labor pain measured fear before or after childbirth and then dissected how the severity of fear was associated with maternal requests for the exact purpose of pain relief.Fear is a stable psychological variable in a short period,which is the theoretical basis for many previous studies that predicted maternal needs during labor but not pain relief behaviors.Fear may have the potential to predict maternal needs and behavior during labor;nevertheless,this hypothesis is in lacks of support from psychophysiological and psychological-behavioral mechanisms.Some researchers believe that fear increases catecholamine concentrations in the plasma[37],and further studies are needed to show how hormonal changes can impact maternal needs and reactions.
Furthermore,labor is perhaps the most stressful,tense,and potentially tragic experience for a woman,and as a result,many stress reactions may be instantly induced during labor.Hence,it is challenging to interpret real maternal needs and responses based on previous psychological expectations before labor happens in the real world.Additionally,FOC consists of four components.Our study reported that fear of baby safety dominated other fearful feelings,including fear of pain.This may be attributed to women concentrating on the baby's safety more than labor pain;thereby,women with greater FOC did not consume more analgesics.
Moreover,it was reported that most childbearing women lacked knowledge about epidural anesthesia [42],and there were many misconceptions and fears associated with epidural analgesia use[43].Primiparas with stronger fears may have more significant concerns about risks to their baby.Thus they may attempt psychologically to balance their pain tolerance and manual bolus requirements to minimize the potential adverse effects that may be caused to their baby.Another speculation is that primiparous labor pain decreased sharply once epidural anesthesia was administered,as did their childbirth fear.Meanwhile,multiparas suffered stronger uterine contraction and were impacted by the memory offormer labor pain [40].Multiparous reactions to painful stimuli might be more sensitive.That's why primiparas consumed fewer analgesics than multiparas,which requires more evidence from empirical studies.
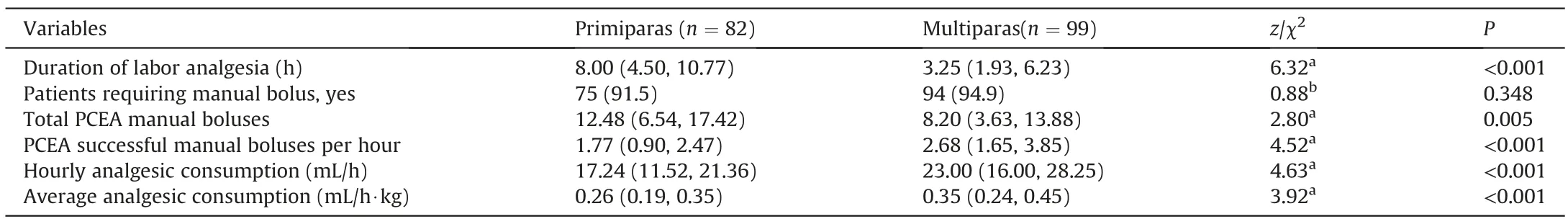
Table 3 Comparison of the amount of pain relief between primiparas and multiparas.
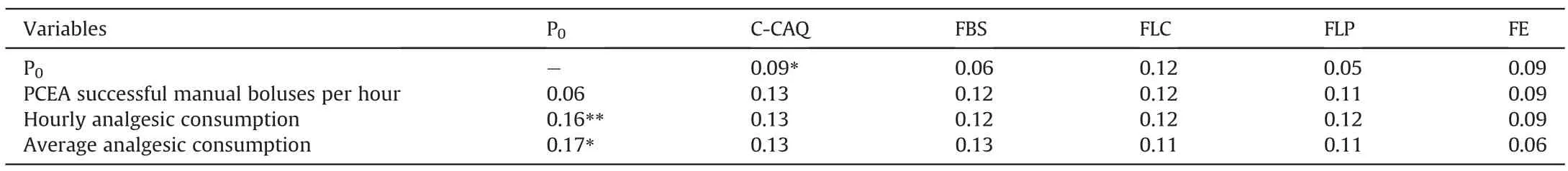
Table 4 Association of pain relief,fear of childbirth scores and maximum in-labor pain in all participants (r).
On the other hand,we failed to prove our second hypothesis that primiparous women will require increased analgesic consumption and request more manual boluses for rescue analgesia,which was a surprising result.We initially proposed our hypothesis based on the results of previous studies on the associations between FOC and pain,with the aim to find some evidence to support our reasoning.The failure to prove that our hypothesis confirmed that childbirth fear was not associated with analgesic consumption.Labor pain and childbirth fears are mutual causes and effects.Therefore,it is challenging to distinguish the dominant factor for laboring women requesting pain relief,while pain is much easier to assess,intervene,and control in practice than childbirth fear in practice.As pain is recognized as the fifth vital sign,medical staff naturally choose pain as the crucial factor to determine whether and when to implement pain relief and how much the women may need.That is,women who have stronger labor pain will need more analgesics.Contrary to our initial reasoning,our findings showed multiparas reported higher maximum labor pain than primiparas and consumed more analgesics.
Our findings partly contradict previous studies on primiparous and multiparous labor pain disparity in that we found that multiparas who received epidural analgesia had stronger maximum labor pain.No more differences were found at other time points.Generally,the discrepancy in pain perceptions between primiparas and multiparas remains controversial [15-18].Some researchers[15,38,39] revealed that multiparas experienced less pain because multiparas were older,did not worry about childbirth,and had less painful sensations and feelings than primiparas.Even for the same group of women who had two consecutive vaginal childbirths,their average maximum labor pain during the latent phase of their first childbirth was slightly higher than that during their second childbirth[40].Ranta P et al.[41]discovered different that pain intensity in grand multiparous women was significantly higher than that in primiparas at the end of the first stage (median scores 7 to 6) and during the second stage of labor(median scores 8 to 6),and women with two to five previous deliveries experienced more pain than primiparas.In a prospective Jordanian study,no significant difference in labor pain was found between primiparas and multiparas[20].Another randomized controlled trial also reported that multiparous women had more intense afterpains than primiparas[18].It is,therefore,safe to conclude that labor pain is changeable as labor progresses;this is one crucial reason why previous studies conducted at different stages of labor failed to come to the same conclusions about the role of parity in labor pain.Another reason is that labor pain is a unique individual feeling.It is difficult to compare the baseline maternal pain perceptions between groups of laboring women with an array of parties.
5.Implications for clinical practice
With the implementation of a new birth policy in China,women with previous childbirth experience continue to increase,and intrapartum pain management is sometimes challenging.Our research adds further evidence to the knowledge about primiparous and multiparous childbirth fear,labor pain,and actual analgesic consumption.When assessed using psychological tools,multiparous labor pain and their need for analgesia may have been underestimated,even though they may not be as fearful as primiparas.It is thereby assumed that this may result from stronger uterine contractions in shorter labor processes among multiparas,but no positive evidence supports this hypothesis.To provide better intrapartum pain management,it is,first of all,recommended that health care providers dynamically and timely assess pain relief requirements in laboring women of the various party.Providing timely and practical support to relieve pain,as demonstrated by maternal feedback,is essential for improving the maternal birth experience.Additionally,obstetricians,midwives,and anesthetists should know that labor pain and childbirth fear are mutual causes and effects.When multiparas report their FOC,labor pain should be the top priority to assess,intervene,and control,regardless of parity.
6.Strengths and limitations of this study
The main strength of our research is that we connected the subjective psychological variable of FOC and the real-world variable by introducing objective indicators for actual maternal consumption of pain relief during.Undoubtedly,this cross-sectional study has limitations.Akin to most previous studies,our study recruited only a small population of women in one hospital.Owing to China’s“general two-child policy”and the convenience sampling we used,multiparas were becoming the mainstream participants in this study,which may produce a population bias.Additionally,we did not collect the total manual boluses the women had attempted including the unsuccessful manual boluses because the pump could not store those data.Even though all participants were taught how to use the epidural analgesia pump to ensure that they could request the manual boluses freely and correctly,we did not evaluate the maternal perspectives and knowledge on PCEA.Accordingly,misunderstandings about the effects of anesthetic on their baby and maternal health may lead to primiparas and multiparas having different behaviors when using the pump.Last,although the scale we adopted to assess the FOC has been validated among Chinese pregnant women and showed good psychological properties,it has not been thoroughly validated in laboring women worldwide.Likewise,our study was limited by the inability to perform subgroup analyses for average FOC and the correlation between maximum in-labor pain and FOC.Thus,it is recommended that the conclusions to other cultural backgrounds or clinical situations should be applied with caution.
7.Conclusions
To bookend the article,FOC was not a strong predictor of pain.Navigating the new terrain of addressing women’s psychological pain of childbirth,this study has not found a correlation between analgesic consumption and the FOC.Further study is needed to explore the role and value of childbirth fear in pain management during childbirth.Parity was not a protective factor for multiparas in our research;nor is it a determinant of pain relief use and should not be a preconceived preference of obstetric care team members to determine the allocation of epidural analgesia,especially when analgesia resources are insufficient.We assert that health care providers assess pain relief requirements in laboring women of various parities dynamically and timely.It is our accountability and adherence to public health that implementation of nonpharmacological and pharmacological pain relief interventions for laboring women is the priority to improve their birth experience.
Funding
This study was funded by Guangzhou Municipal Science and Technology General Guide Project (20201A011028) and Nursing Research Fund of Guangzhou Women and Children’s Medical Center(HLB-2020-13).
Credit authorship contribution statement
Yongfang Deng:Conceptualization,Methodology,Writing -original draft,Writing-reviewing and editing,Writing -review &editing,Project administration,Fund acquisition.Yan Lin:Conceptualization,Supervision,Project administration,Resources,Writing-review&editing.Liyuan Yang:Resources,Methodology.Qiuxia Liang:Conceptualization,Funding acquisition,Methodology.Bailing Fu:Resources,Project administration.Huixian Li:Writing -review &editing,Formal analysis,Data curation,Visualization.Huizhu Zhang:Resources,Project administration.Yan Liu:Methodology,Project administration.
Declaration of competing interest
The authors have declared no conflict of interest.
Acknowledgments
The authors are grateful to all the participants,the nurses and midwives who supported and encouraged us.
Data availability statement
The dataset used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Appendix A.Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijnss.2021.09.003.
 International Journal of Nursing Sciences2021年4期
International Journal of Nursing Sciences2021年4期
- International Journal of Nursing Sciences的其它文章
- Second-order problem solving:Nurses’ perspectives on learning from near misses
- Exploring the employment readiness and return to work status of breast cancer patients and related factors
- Resilience of nurses at the epicenter of the COVID-19 pandemic in Lebanon
- A study of the relationship between nurses’ experience,structural empowerment,and attitudes toward computer use
- Mobile health applications for the care of patients with breast cancer:A scoping review
- Nursing students’ attitudes toward mobile learning:An integrative review
