Safety and effectiveness of an iris hook assisted phacoemulsification in vitrectomized eyes
Ling Bai, Yan-Fen Wang, Farheen Tariq, Yu-Ping Zheng, Hai-Xiao Feng, Feng Wang,Shu Zhang
1Department of Ophthalmology, the Second Affiliated Hospital of Xi’an Jiaotong University, Xi’an 710004, Shaanxi Province,China
2Experimental Teaching Center for Clinical Skills, the Second Affiliated Hospital of Xi’an Jiaotong University, Xi’an 710004,Shaanxi Province, China
3Department of Geriatric Medicine, the Second Affiliated Hospital of Xi’an Jiaotong University, Xi’an 710004, Shaanxi Province, China
Abstract
INTRODUCTION
With the continuous evolution in vitrectomy techniques and instrumentation, an increasing number of vitreous and retinal diseases are successfully managed with the surgery of pars plana vitrectomy (PPV). But the surgery interferes with the normal intraocular structure and removes the barrier function provided by the vitreous, then lead to increased oxygen exposure to the lens, changes in the lens capsule permeability, and finally promototing the formation of cataract[1-3]. The incidence of development of cataract after PPV ranges from 4% to 80 % in various studies, and even up to 100% within a 2-year follow-up observation[4-7]. Eventually,most of the patients require cataract surgery.

Figure 1 Different procedure of phacoemulsification in completely vitrectomized eyes A: Iris hook was placed at 8 o’clock corneal limbus position (vertically to the main incision); B: A 25G pars plana irrigation was performed at 3.5-mm posterior to the limbus; C: Routine phacoemulsification.
Because of the normal anatomy is altered, such as the absence of vitreous support and zonular laxity, the cataract surgery in vitrectomized eyes is at high risk for intraoperative and postoperative complications. Although Phacoemulsification(PE) with intraocular lens (IOL) implantation is a relatively safe procedure in vitrectomized eyes, the intraoperative abnormal chamber deepening, unstable posterior capsules, and fluctuation of pupil size are still big challenges for cataract surgeons[8]. Currently, the commonly used procedures included using infusion cannula inserted at pars plana during PE or placing the second instrument to lift the iris immediately after lens-iris diaphragm retropulsion syndrome (LIDRS)happened[8-9]. The former could provide additional capsular support, but it prolongs the operation time and needs a skilled assistant to control the infusion flow during surgery. The latter one needs proficient surgical skills and has the risk to damage the iris. Furthermore, the literature on the prevention of anterior chamber fluctuation during PE in vitrectomized eyes is sparse.
In this study, we introduce a simple iris hook assisted PE for cataract in vitrectomized eyes, and evaluate its safety and efficacy by comparing its operative parameters and complications with the two popular methods.
SUBJECTS AND METHODS
Ethical ApprovalThe study was approved by the medical ethics board of the Second Affiliated Hospital of Xi’an Jiaotong University and complied with the Declaration of Helsinki. Informed written consent was obtained from each enrolled patient. The sample size was calculated by G Power 3.1.9.7, assigned effect size of 0.4, an error 0.05, power 0.8.The study was registered at clinicaltrials.gov (NCT03584139).
Subjects and ExaminationThis prospective randomized comparative interventional case series study comprised 65 eyes of 62 patients with significant cataract after 23G/25G complete vitrectomy, which needed to undergo cataract surgery. Detailed slit-lamp biomicroscopy and dilated fundus ophthalmoscopy examination were performed. The IOL power was calculated using the IOL Master 500 in 56 eyes and A-Scan in 9 eyes with the SRK/T formula. The objective degree of nucleus density was obtained from 1 to 5 using pentacam nucleus densitometry(PND) software in Pentacam Scheimpflug imaging system(Oculus, Wetzlar, Germany).
Patients were divided into 3 groups randomly. In group A,patients received PE and IOL implantation with the assistance of an iris hook (SynergetiesTM). In group B, PE was assisted with a 25G pars plana irrigation. In group C, PE performed without the help of any instrument.
The details of surgery duration, Ultrasound (U/S) total time,cumulative dissipated energy (CDE), and the incidence ofany complication (LIDRS, iris damage, miosis, posterior capsular tears, zonular dialysis, and postoperative cystoid macular edema) were recorded. All patients were reviewed at a postoperative interval of 4wk. The outcome measures were preoperative and postoperative best-corrected visual acuity (BCVA), intraocular pressure (IOP) and endothelial cell density (ECD).

Table 1 Phacoemulsification hydrodynamic parameters
Surgical TechniqueThe surgical procedures (Figure 1)were performed by the same surgeon (Bai L). The type of anesthesia was sub-Tenon with lidocaine. For group A, an iris hook was placed at 8 o’clock corneal limbus position(vertically to the main incision) to lift the iris at the beginning of the surgery, then started routine PE as following. A 3.0-mm clear corneal incision at 11 o’clock was made, then 5.5-mm continuous curvilinear capsulorhexis and hydrodissection was achieved. The PE was performed with a technique of “stopchop” (Ozil IP, Infiniti, Alcon). Finally, a yellow-coloured UVfilter hydrophobic IOL (HOYA PY-60R) was implanted in the capsular bag. The intraoperative hydrodynamic parameters were set I in Table 1. For group B, a 25G pars plana irrigation was performed at 3.5-mm posterior to the limbus at the beginning of the surgery, then started routine PE. The hydrodynamic parameters started from set I in Table 1. The assistant adjusted the pars plana irrigation on/off and hydrodynamic parameters according to the local situation during surgery. For group C, routine PE was performed without the assistance of any instrument. The hydrodynamic parameters started from set I in Table 1, when excessively anterior chamber deepening,pupil dilatation and patient pain occurred, the parameterschange to set II in Table 1. If still irreversible, the chopper was used to lift the iris margins immediately as recommended[9-10].After surgery, topical Tobradex®(tobramycin and dexamethasone ophthalmic suspension) and pranoprofen (nonsteroidal anti-inflammatory drugs, NSAIDs) eye drops were administered 4 times a day in the first two weeks, followed by topical NSAIDs over 6wk.

Table 2 Basic characteristics for 65 eyes in this study
Statistical AnalysisSPSS version 23 (SPSS Inc., Chicago,IL, USA) statistical software was utilized to analyze the data.BCVA was converted to a logarithm of the minimum angle of resolution (logMAR) equivalent for analysis. The data were compared using ANOVA or Fisher’s exact test among the three groups. APvalue of <0.05 was considered statistically significant. Bonferroni adjust requiredP<0.0167 as significant.
RESULTS
The patient demographics, indication for PPV, type of intravitreal tamponade, the interval between PPV and PE were all noted at the beginning (Table 2). There was no significant difference among the three groups in sex, indication for PPV,PPV times, interval between PPV and cataract surgery, axial length (AL), and PND (Table 2).
The mean preoperative BCVA was improved, and the mean ECD decreased significantly at 4wk after surgery in all three groups (P<0.05). We did not observe any significant difference in BCVA, IOP, and ECD among the groups (P>0.05). While the ECD loss rate in group A was significantly lower than the other two groups (P<0.05; Table 3).
The surgery duration of group B was much longer than other groups (P<0.05). Although there was no significant difference between group A and C (P>0.05), the duration of group A was still the shortest (Table 3). The CDE and U/S total time was estimated of total PE energy. The less of them, the less heat generation and damage during surgery. The CDE and U/S total time difference among them were significant (P<0.05). The minimal CDE and U/S total time were in group A, which were much less than group B and group C (P<0.05; Table 3).
The complications included LIDRS, iris damage, miosis,posterior capsular tears, zonular dialysis, and cystoid macular edema. LIDRS happened in 11 eyes (55%) of group C, 3 eyes(15%) in group B, while none in group A (P=0.00). Paired comparative analysis after Bonferroni adjust showed LIDRS happened much less in group A than group C (P<0.0167).To reverse LIDRS, a chopper was used to lift the edge of the iris, and thus damaged iris in 3 eyes (15%) of group C. None happened in group A and group B. Miosis happened in 2 eyes(8%) in group A, 3 eyes (15%) in group B, and 4 eyes (20%)in group C. Posterior capsular tears occurred in 2 eyes (10%),zonular dialysis in 1 eye (5%), cystoid macular edema in 1 eye(5%) in group C, and none in group A and B (allP>0.05; Table 4).
DISCUSSION
The patients involved in this study were undergone complete vitrectomy and severe cataract. Complete was emphasized because these eyes have entirely lost vitreous support and zonular laxation. There will be more incidence ofcomplications during PE. In group C, the anterior chamber was much deeper than other groups for the absence of additional vitreous support and zonular laxation. The handpiece of PE needed to be inserted deeply and perpendicular during any procedure, which limited manipulation feasibility and increased nucleus chopping difficulty. This could explain the maximum U/S total time and CDE among the three groups.Two lenses were divided with chopping technique out of the bag at the anterior chamber, which may increase the endothelial cell injury, and the technique is not easy to operate.In group B, we inserted an infusion cannula at pars plana to aid in maintaining IOP stability and provide additional capsular support during PE in vitrectomized eyes. But this procedure needs a second bottle of infusion and prolong the surgery duration, which is significantly longer than other groups. Two eyes needed to suture the sclera infusion incision at the end.It is noteworthy that a skilled assistant is required for this procedure to control the on/off of infusion valve during surgery according to the anterior chamber fluctuation, which is not easy for a junior surgeon. In group A, an iris hook was used to lift the iris at the beginning of the surgery. A gap will be formed between the iris and lens capsule. Once the irrigation starts, the pressure between the anterior and posterior chambers could equalize automatically. Vishwanath[11]first tried this method in a small group of patients, without further systematical and comparative observation. In this study, we found it was easy to maintain the anterior chamber stable in vitrectomized eyes by using an iris hook during PE. The surgery duration was 15.0±1.5min, significantly less than group B, while the U/S total time and CDE were significantly less than group B and C, which minimized heat generation and damage to the eye.Mean ECD loss after PE in various studies ranges from 6% to 12%[12-13], similar to that in our study. Although there was no difference in the absolute value of perioperative ECD between the groups, the ECD loss rate is significantly lower in group A,which could be explained by the least CDE and U/S total time use.
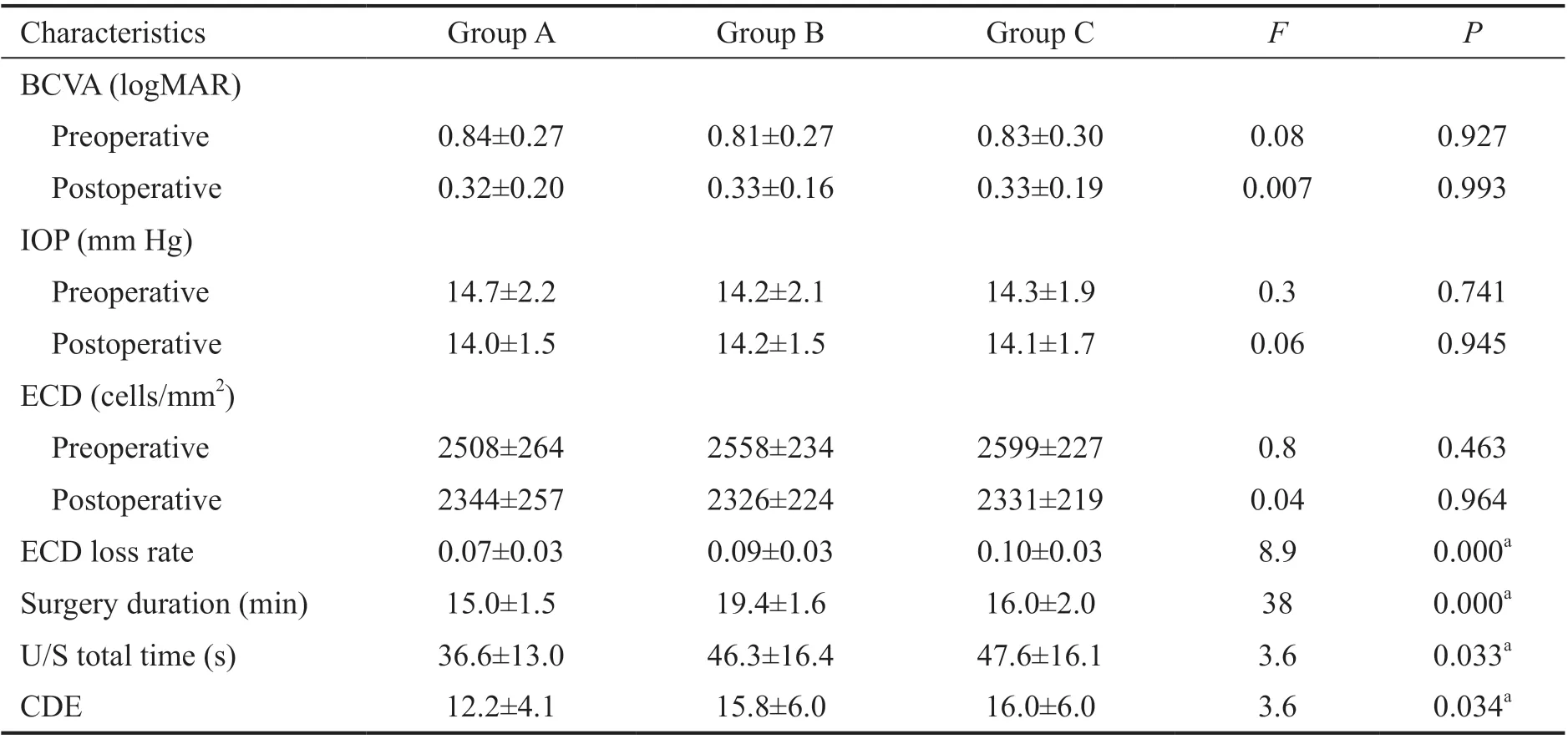
Table 3 Perioperative characteristics of each procedure

Table 4 Complications of each procedure n (%)
LIDRS is characterized by anterior chamber deepening,retropulsion of the iris, and pupil dilation during PE. Patients have discomfort and pain under topical anesthesia suddenly,and an excessively deep anterior chamber renders PE more difficult. Post-vitrectomized eyes, especially with extensive or multiple vitrectomy is its risk factors[14], because loosen zonular and an infusion pushed 360-degree iridocapsular contact is its predominant cause[15-16]. If it can’t be reversed, a sudden collapse of the anterior chamber and pupillary miosis(infusion deviation syndrome) may happen. In group C, we observed LIDRS occurred in 55% of patients, it is consistent with the study of Ghoshet al[9](53%).We first lowered fluidic parameters (from set I to set II). If it’s still irreversible, a chopper immediately used to lift the edge of the iris to equalize the pressure between the anterior chamber and the posterior chamber, as described by Cheung and Hero[15]. We need to repeat this operation each time when the eye is entered infusion, and thus 3 eyes (15%) had iris injury during the procedure. One eye with iris injury finally occurred macular edema 4wk after surgery. While no LIDRS, resulting from the gap for preventing 360-degree iridocapsular contact, happened in Group A. Without lifting the iris by rigid chopper, iris damage also didn’t happen. Slight miosis occurred in 2 eyes during surgery, but the pupil still semi dilated. After adrenaline anterior chamber administration, we got dilated pupil and completed the surgery.
Posterior capsular rupture (PCR) is the most common complication during PE in vitrectomized eyes[4]. Leeet al[17]reported about 11.4% and attributed it to unstable anterior chamber depth, flaccid and mobile posterior capsule in vitrectomized eyes. In consistent with the references, PCR occurred in 2 eyes (10%) in group C. Because of the extra infusion in the vitreous cavity and consequently stabilized posterior capsule, no PCR occurred in group A and group B.Zonular dialysis also didn’t occur in these two groups due to the stable anterior chamber depth and no more damage to zonular.
Although the incidence of iris damage, miosis, PCR, zonular dialysis, and cystoid macular edema did not show any significant difference among three groups, we think it may be significance with a larger sample size for the obvious feasibility and safety in group A. Furthermore, PE hydrodynamic parameters in group A are the same as in non-vitrectomized eyes (set I). The stop-chop technique in the capsular bag was performed easily for all the patients in this group.
Postoperative BCVA are all improved in three groups at 4wk follow-up, without any significant difference between the groups. However, we still emphasize that the outcomes depend on the retina status and preexisting posterior segment pathology, not the technique. Another trifle thing we want to mention is that vitrectomized eyes may experience pain and discomfort due to the iris fluctuation and LIDRS. We suggest sub-Tenon anesthesia to make patients more comfortable during surgery. The IOL used in this study is a yellow-colored blue light-filter IOL (HOYA PY-60R), which is designed to reduce the absorption of ultraviolet (UV) and short-wavelength visible light. It can be used in vitrectomized eyes and possibly providing macular protection[8,18-19].In conclusion, PE in vitrectomized eyes is a challenging situation. With the assistance of an iris hook, we can achieve a stable anterior chamber and minimize the incidence of complications. There is also no need to change the hydrodynamic parameters and PE in the bag technique, easy to operate even for junior surgeons.
ACKNOWLEDGEMENTS
Foundation:Supported by the Research and Development Program of Shaanxi Province (No.2021SF-161).
Conflicts of Interest: Bai L,None;Wang YF,None;Tariq F,None;ZhengYP,None;Feng HX,None;Wang F,None;Zhang S,None.
 International Journal of Ophthalmology2021年11期
International Journal of Ophthalmology2021年11期
- International Journal of Ophthalmology的其它文章
- Toric implantable collamer lens for the management of pseudophakic anisometropia and astigmatism
- Efficacy of rhNGF-loaded amniotic membrane transplantation for rabbit corneal epithelial and nerve regeneration
- lncreased cGAS/STlNG signaling components in patients with Mooren’s ulcer
- lnhibition of corneal neovascularization by topical application of nintedanib in rabbit models
- TGF-β2-induced NEAT1 regulates lens epithelial cell proliferation, migration and EMT by the miR-26a-5p/FANCE axis
- Protective effect of human umbilical cord mesenchymal stem cell-derived exosomes on rat retinal neurons in hyperglycemia through the brain-derived neurotrophic factor/TrkB pathway
