lndividuals with and without normal tension glaucoma exhibit comparable performance on tests of cognitive function
Qi N. Cui, David Green, Mohit Jethi, Todd Driver, Travis C. Porco,2, Jane Kuo,Shan C. Lin,5, Robert L. Stamper, Ying Han, Cynthia S. Chiu, Saras Ramanathan,Michael E. Ward, Katherine Possin, Yvonne Ou
1Department of Ophthalmology, University of California San Francisco, San Francisco, California 94143, USA
2Francis I. Proctor Foundation, University of California San Francisco, San Francisco, California 94143, USA
3Department of Neurology, University of California San Francisco, San Francisco, California 94143, USA
4University of Pennsylvania, Philadelphia, Pennsylvania 19104, USA
5Glaucoma Center of San Francisco, San Francisco, California 94105, USA
6Neurogenetics Branch, National Institute of Neurological Disorders and Stroke, National Institutes of Health, Bethesda,MD 20892, USA
Abstract
INTRODUCTION
Glaucoma is the leading cause of irreversible blindness in the United States with an estimated treatment cost in excess of $7.7 billion in 2020[1-2]. Even more substantial is the monetary cost of dementia, which was in the range of $305 billion in 2020[3]. Both diseases increase in prevalence with age; glaucoma increases from 3 to 16-fold between 40 and 80 years of age, and dementia increases 25-fold between ages 65 and 85[4-7]. Globally, as the number of older adults increases in an aging population, the number of patients with both conditions are sure to follow.
In a prospective population-based cohort study, Helmeret al[8]found a four-fold increase in the incidence of Alzheimer’s disease (AD) among subject with open angle glaucoma(OAG) over a three year period. Interestingly, none of the subjects who later developed AD were documented as having intraocular pressures (IOP) >21 mm Hg, suggestive of an underlying diagnosis of normal tension glaucoma (NTG). This association between normal IOP and dementia in subjects with glaucoma is supported by the findings of two additional cross-sectional studies[9-10]. If present, a link between NTG and dementia is intriguing as it suggests an IOP-independent susceptibility to neurodegeneration that manifests in both the eye and the brain. Pathologic features associated with AD,including increased tau and decreased amyloid-beta 1-42 proteins, have been demonstrated in patients with glaucoma,while increased concentrations of apoproteins have been found in the aqueous humor of eyes with primary OAG[11-14].Structural evidence of a connection between glaucoma and neurodegenerative conditions also exists in the form of several studies demonstrating an association between decreased retinal nerve fiber layer (RNFL) and ganglion cell-inner plexiform layer thickness and cognitive decline/dementia on optical coherence tomography (OCT)[15-18].
Alternatively, it is possible that those diagnosed with both NTG and dementia, while exhibiting RNFL thinning and optic disc cupping that appear glaucomatous, were in fact manifesting ocular signs of a global neurodegenerative process[19-24].Indeed, although a series of retrospective studies showed an increased risk for dementia in those with OAG, several other registry-based studies found no correlation between glaucoma and dementia[25-31]. More recently, a prospective study found higher incident dementia in Chinese patients with self-reported glaucoma[32]. In contrast, 2 retrospective studies both found decreased odds for an AD diagnosis in patients with OAG[33-34]. Still other studies attempted to answer this question by utilizing neuropsychological assessments to screen for cognitive impairments in subjects with glaucoma, yielding conflicting results[35-37]. For example, whereas Harrabiet al[35]associated a diagnosis of glaucoma with impaired performance on the Mini-Mental Status Examination blind version (MMSEblind), Jefferiset al[36]demonstrated comparable performance between glaucoma subjects and controls using the same test.
To clarify whether a connection exists between NTG and neurodegenerative processes, this study administered a battery of cognitive tests to NTG and control subjects. Tests examined executive function, learning, and memory, which are often impaired in the “mild cognitive impairment (MCI)”stage of AD and other dementing disorders[38]. Specifically,the Executive Abilities: Measures and Instruments for Neurobehavioral Evaluation and Research (EXAMINER) is a computer-based battery designed to provide a comprehensive evaluation of executive function[39]. The battery was constructed and scaled using neurological conditions such as AD, and validatedviameasurements of real-world executive function and correlation with dorsolateral prefrontal brain volumes[40]. In addition, the full-length California Verbal Learning Test-Second Edition (CVLT-II) is a widelyvalidated and sensitive assessment of learning and memory in various forms of dementia[41-43]. NTG and control subjects demonstrated similar performance on both sets of tests. As such, the results of this study did not support the hypothesis that individuals with NTG have a higher risk for cognitive dysfunction and dementia.
SUBJECTS AND METHODS
Ethical ApprovalThis study was conducted in accordance with the Declaration of Helsinki and the regulations of the Health Insurance Portability and Accountability Act (HIPAA).Informed consent was obtained. Institutional Review Board(IRB) at the University of California, San Francisco (UCSF)approved this study.
The electronic medical records from the UCSF Department of Ophthalmology were queried on June 12, 2014 to identify patients who had at least one ophthalmology visit since January 1, 2013 and carried a diagnosis of either “low-tension open angle glaucoma” (ICD9 code 365.12) for the NTG group, or“cataracts” (ICD 9 codes 366.00-366.9) for the control group.The EMR of these patients were then reviewed for inclusion in the study.
Inclusion criteria were as follows: 1) age ≥50y; 2) mentally capable of giving consent for participation; 3) English fluency;4) maximum IOP (Tmax) ≤21 mm Hg and/or an existing diagnosis of NTG as determined by glaucoma specialists for the NTG group. Exclusion criteria were as follows: 1)best corrected visual acuity (BCVA) <20/50 in either eye;2) glaucoma diagnoses other than NTG; 3) diagnoses of glaucoma, glaucoma suspect, or ocular hypertension for control subjects; 4) an ocular history that includes exudative age-related macular degeneration, proliferative diabetic retinopathy, central retinal artery occlusion, central retinal vein occlusion, or non-glaucomatous optic neuropathy secondary to ischemic, compressive, or infiltrative causes (e.g.,anterior ischemic optic neuropathy, pituitary adenoma, or intracranial hypertension).
Qualifying subjects were contacted by telephone regarding voluntary participation. A total of 396 NTG patients were identified, of which 222 patients qualified for the study and were contacted for participation. In comparison, 715 control patients were identified, of which 541 patients qualified for the study and were contacted for participation. The first 50 people from each group who agreed to participate and completedall testing were included in the study (Table 1). For the NTG group, glaucoma severity was determined based on the most recent Humphrey visual field (HVF) of the worse eye, and subjects were classified as mild, moderate, or severe based upon established ICD-9 staging criteria[44]. The number of antiocular hypertensive medications, vertical cup-to-disc ratio(CDR), as well as the most recent HVF mean deviation (MD)and the mean RNFL thickness measured by OCT were also collected for the NTG group.
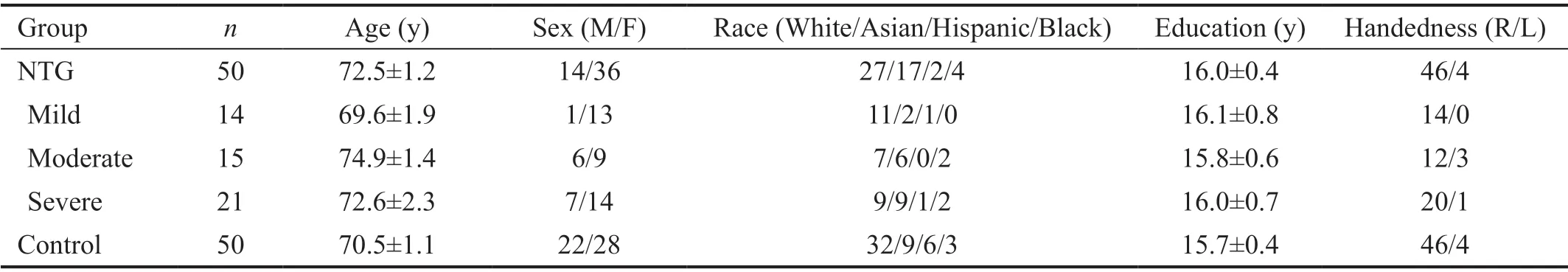
Table 1 Demographic characteristics of the study population mean±standard error
In-person testing was conducted in the UCSF Ophthalmology Clinic between August 2014 and March 2015 by trained examiners. Testing required 45-60min to complete. At the time of testing, subjects were also queried regarding selfreported race, education, and handedness. Testing consisted of sequential administrations of: 1) the EXAMINER battery to assess executive function; 2) the CVLT-II to assess learning and memory.
EXAMINERSubject were administered four tests from the EXAMINER battery: Flanker, Dot counting, N-back, and Animal fluency. A standard 15.4” Apple MacBook Pro laptop was used to administer the computerized portions of the battery, as well as to record subject response, accuracy, and reaction times. Domain scores inCognitive Control(Flanker),Working Memory(Dot Counting and N-Back), andFluency(Animal fluency), and an overallExecutive Compositescore derived from performance on all four tests, were generated for each subject using item response theory as previously described[45]. These scores have been shown to have good psychometric properties including no ceiling or floor effects.
The specifics of the testing paradigm are described elsewhere and are available at http://examiner.ucsf.edu[45]. Briefly, Flanker required subjects to observe a row of arrows pointing either to the right or to the left of the screen and to indicate the direction of the central arrow by pressing the corresponding key. In order to respond accurately to this test of cognitive control,subjects needed to suppress all reactions to the directions of the surrounding arrows. Dot counting assessed verbal working memory and required subjects to tally, one screen at a time, the total number of dots of a specific color shown on a consecutive series of up to 7 computer screens. Subjects were then asked to recall the total number of dots from each screen in the same order in which they were presented. Similarly, N-back assessed spatial working memory by asking subjects to determine whether the location of a white square on the computer screen was the same as that of a square presented either immediately before (1-back) or two before (2-back) the current square.Finally, animal fluency assessed verbal fluency by asking subjects to name as many animals as possible in a 60s period.
California Verbal Learning Test-Second EditionThe specifics of the testing paradigm are described elsewhere[43].Briefly, the test was administered on an individual basis using standardized paper forms and began with five learning trials where a list of 16 words were read to the subject. After each trial, the subject verbally recalled as many words from the list as possible, and accurate responses were summed across these 5 trials (Immediate Recall). The subject was then read and asked to recall an interference list of 16 words. The subject then recalled the words from the first list after a short delay (Short-Delay Free Recall) and then after a 20-minutes long delay (Long-Delay Free Recall). Finally, Long-Delay Recognition required the subject to identify words from the first list from a list containing 32 distractor words.
Charlson Comorbidity IndexThe Charlson Comorbidity Index contains 19 medical conditions that are weighted based on the adjusted risk of mortality at one, five, and ten years for each condition[46]. As a substitute for a measure of general health, an age-adjusted Charlson score representing 10-year mortality was calculated for each subject based upon ICD-9-CM and procedure codes. A higher score on the index reflects more severe comorbidity.
Data AnalysisMultivariate linear regression models were used to compare NTG to controls with respect to group performance on the CVLT-II and the EXAMINER battery,while controlling for age, sex, and education. AP-value<0.05 was considered significant. Age, years of education,BCVA (converted to logMAR), Tmax, CDR, HVF and OCT parameters, as well as the Charlson score, were compared between NTG subgroups (i.e.mild, moderate, and severe) and between NTG and controls using ANOVA with post-hoc Tukey HSD. Sex, race, and handedness were compared using Fisher’s exact test. All computations were done using R version 2.10 (R Foundation, Vienna Austria, http://www.r-project.org).
RESULTS
The NTG and control groups were comparable with respect to age, sex, race, education, and handedness (P>0.07; Table 1).The Charlson score was also comparable between NTG and controls (4.44±0.44vs3.66±0.22, respectively;P=0.12).BCVA was comparable between all NTG subgroups as well as between NTG and controls (P>0.51; Table 2). While Tmax was comparable between NTG subgroups (P>0.12), other glaucoma-related ocular characteristics of CDR, HVF MD,and RNFL thickness were significantly different between the three NTG subgroups (P=0.01, 0.01, and 0.04, respectively;Table 2).
EXAMINER Executive Composite and domain scores were comparable between NTG subgroups (P>0.47; Figure 1 and Table 3). The Executive Composite and the domain scores of Fluency and Working Memory were comparable between NTG and controls (P≥0.06). In comparison, the domain score of Cognitive Control differed between NTG and controls with the control group performing significantly worse compared to the NTG group (P=0.01). Sub-analyses comparing the NTG subgroups to controls revealed significance only between the moderate NTG group and controls with respect to the domain score of Cognitive Control (P<0.03).
All CVLT-II scores were comparable between NTG subgroups as well as between NTG and controls (P≥0.24 for all; Figure 2 and Table 3). A power calculation was also conducted for the EXAMINER Executive Composite and CVLT-II LD Recognition scores. For both measures, 50 cases and 50 controls provided 80% power to detect a moderate effect size of 0.57.
DISCUSSION
This is one of the first prospective studies in which the cognitive function of subjects with NTG were evaluated using a comprehensive electronically-administered battery of neurocognitive tests designed to assess executive function,memory, and learning. The NTG and control groups were well-matched with respect to age, sex, race, education, and handedness as well as the Charlson score, which served as a surrogate measure of general health. The EXAMINER Executive Composite score was similar between groups, as were performances on tests designed to target verbal fluency and working memory. Similarly, no difference was observed between NTG and controls with respect to memory and learning as assessedviathe CVLT-II. Testing also did not demonstrate any correlation between glaucoma severity and cognitive function, which is consistent with at least one prior report[47].
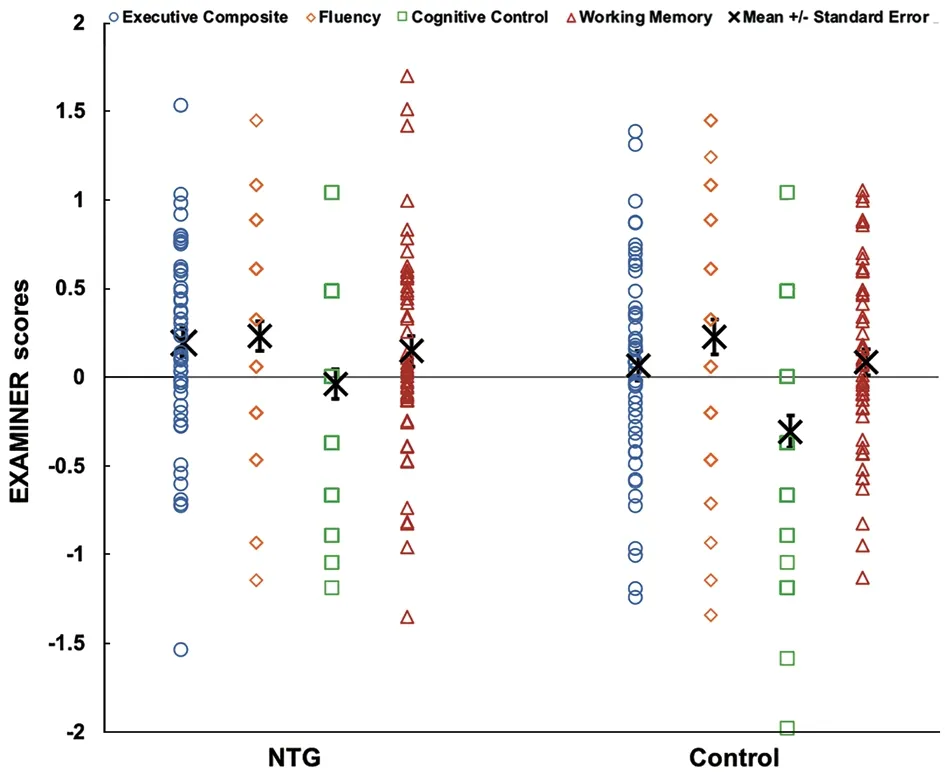
Figure 1 EXAMINER executive composite and domain scores(e.g. fluency, cognitive control, and working memory) for normal tension glaucoma and control subjects Error bars indicate standard error. NTG: Normal tension glaucoma.

Figure 2 CVLT-II scores for normal tension glaucoma and control subjects Error bars indicate Standard Error. NTG: Normal tension glaucoma; SD: Short-delay; LD: Long-delay.
Interestingly, the control group performed significantly worse than the NTG group with respect to one executive function domain, Cognitive Control. This domain was measured by the Flanker test, which is arguably the least challenging test in the EXAMINER battery employed for this study, as it only requires correctly indicating the direction of a single arrow. It is therefore somewhat surprising that the controls did worse on this test compared to the NTGs while performance on all other tests were comparable between groups. One possible explanation may be a difference in the level of motivation.While many subjects in the NTG group were aware of the connection between glaucoma and dementia, the same cannot be said of the control group. This difference in emotional investment and interest may have resulted in a difference in attention and performance between groups, which was most noticeable during Flanker testing.
Despite the outcomes of the Flanker test, taken as a whole,we found no evidence an association exists between NTG and deficits in executive function, learning, or memory.Importantly, this study was sufficiently powered to detectmoderate effect sizes in our primary outcomes. The results of this study are supported by a recent publication showing similar neurocognitive function as measured by the Montreal Cognitive Assessment in OAG patients compared to controls[48].Results do not support the hypothesis that glaucoma patients have worse cognitive function, which are typically evident in MCI or dementia, and thus increased risks for dementia. Our results are also in line with findings from multiple registrybased studies, and a recent retrospective study demonstrating lower AD and dementia risks in patients with OAG[28-31,33].Another database study paradoxically demonstrated lower AD risk but higher MCI risk in OAG patients, which is difficult to interpret without additional context as to the criteria upon which these diagnoses were made[34].
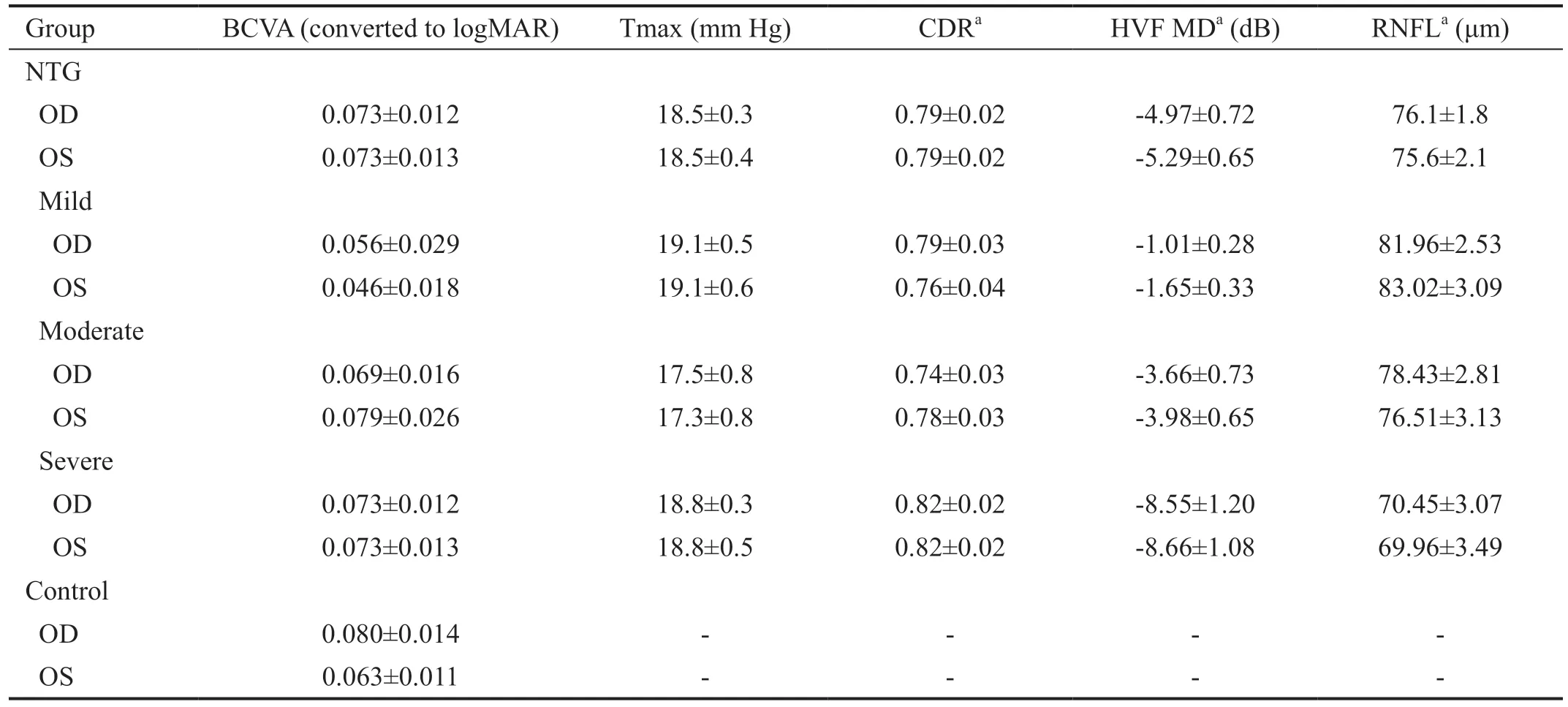
Table 2 Ocular characteristics of the study population mean±standard error
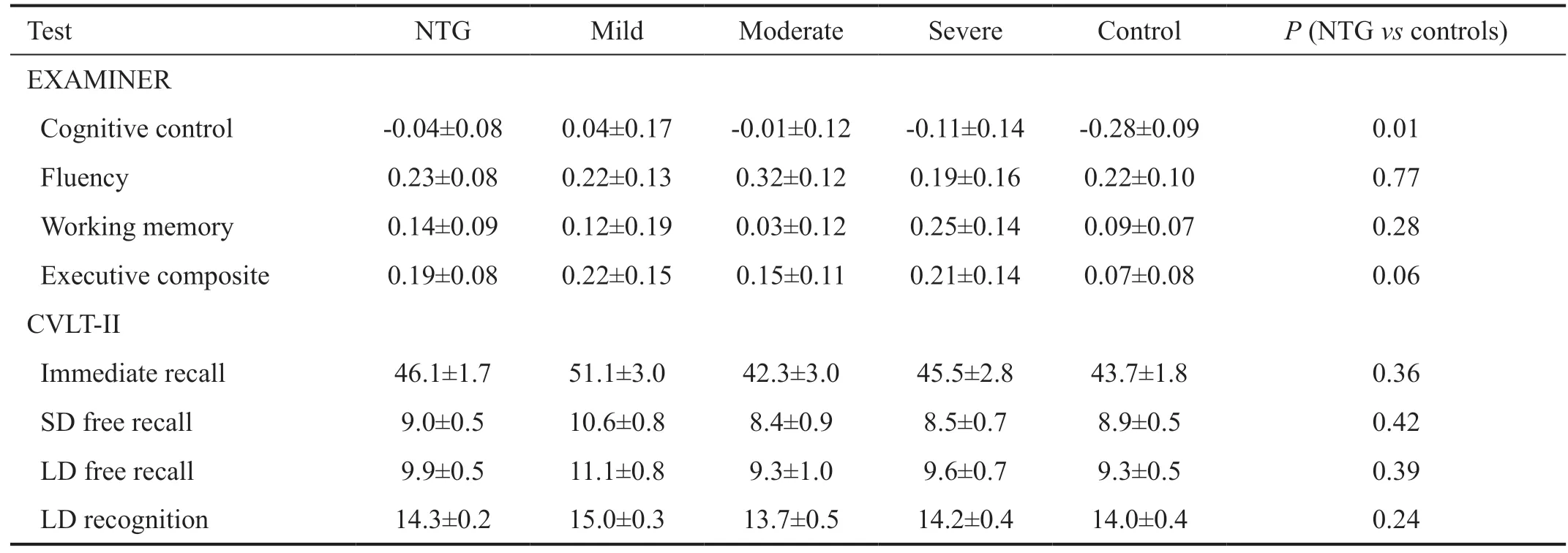
Table 3 EXAMINER and CVLT-II scores for normal tension glaucoma sub-groups as well as controls mean±standard error
Controversy exists as to whether low vision directly impacts cognitive function. Jefferiset al[36]associated glaucoma with poor performance on the MMSE but not on the less visually-demanding MMSE-blind. In contrast, Harrabiet al[35]demonstrated lower performance on the MMSE-blind in those with vision loss due to age-related macular degeneration,Fuchs’ corneal dystrophy, and glaucoma compared to sighted individuals. To preclude potential confounding effects of visual impairment, all participants in this study had BCVA ≥20/50 in both eyes.
The Helmeret al[8]study, which found a four-fold increase in the incidence of AD among OAG subjects, may have been affected by methodological issues in subject identification. The OAG cohort was identified based upon non-mydriatic, nonstereo color disc photos. While the diagnosis was confirmed through an ophthalmology exam, the contribution of optic nerve head imaging, and to a lesser extent, visual field testing, in establishing the OAG diagnosis was unclear. Due to this categorization ambiguity, the possibility that those OAG patients who went on to an AD diagnosis actually had dementia-associated RNFL thinning and/or optic nerve atrophy cannot be excluded. RNFL thinning and optic nerve atrophy have been demonstrated in the eyes of those with AD and MCI, and given that RNFL thinning in AD and MCI are often most prominent in the superior quadrant, may well mimic glaucomatous optic neuropathy in appearance[19-24]. Similar subject identification issues exist in the series of populationbased studies out of Taiwan, which in combination suggested a higher risk for AD in those with OAG[25-27]. In those studies,the glaucoma cohort was identified based on ICD-9-CM codes and glaucoma treatments without the benefit of additional chart review or ophthalmic examination. The criteria by which these subjects received the OAG diagnosis were not reported. The same diagnostic ambiguity also exists in a 2020 prospective study of Chinese patients in Shanghai, where OAG diagnoses were self-reported[32].
Strengths of our study include the robustness of the cognitive tests employed. The EXAMINER battery is a comprehensive and well-validated assessment of executive function. Likewise,the CVLT-II is a well-validated and widely-utilized test for learning and memory. Used in combination, these two tests provided coverage for multiple elements of cognition known to be affected in MCI and early dementia. Furthermore,unlike other studies which are based on registry information alone, all subjects in this study were: 1) directly evaluated by ophthalmologists in a glaucoma specialty ophthalmology clinic; 2) underwent chart review by glaucoma specialists prior to enrollment to ensure correct diagnoses of NTG for the glaucoma group or lack thereof for the control group.A possible limitation of this study is the fact that examiners were not blinded to NTG or control status, which could have introduced bias in testing administration.
In summary, this study evaluated cognitive impairment in a population of NTG subjects utilizing a battery of tests designed to assess executive function and memory. Results do not support an increased risk for cognitive dysfunction in subjects with NTG compared to controls without glaucoma.Future studies with a larger cohort and prospective followup involving repeat testing are needed to elucidate the relationship between glaucoma and cognitive dysfunction before determinations about the presence or absence of a true connection can be made.
ACKNOWLEDGEMENTS
The authors would like to acknowledge Dr. Ari Green for assisting with project conception.
Foundation:Supported by the Core Grant for Vision Research and the Research to Prevent Blindness Unrestricted Grant to the UCSF Department of Ophthalmology (No.NIH-NEI EY002162).
Conflicts of Interest: Cui QN,None;Green D,None;Jethi M,None;Driver T,None;Porco TC,None;Kuo J,None;Lin SC,None;Stamper RL,None;Han Y,None;Chiu CS,None;Ramanathan S,None;Ward ME,None;Possin K,None;Ou Y,None.
 International Journal of Ophthalmology2021年11期
International Journal of Ophthalmology2021年11期
- International Journal of Ophthalmology的其它文章
- Toric implantable collamer lens for the management of pseudophakic anisometropia and astigmatism
- Efficacy of rhNGF-loaded amniotic membrane transplantation for rabbit corneal epithelial and nerve regeneration
- lncreased cGAS/STlNG signaling components in patients with Mooren’s ulcer
- lnhibition of corneal neovascularization by topical application of nintedanib in rabbit models
- TGF-β2-induced NEAT1 regulates lens epithelial cell proliferation, migration and EMT by the miR-26a-5p/FANCE axis
- Protective effect of human umbilical cord mesenchymal stem cell-derived exosomes on rat retinal neurons in hyperglycemia through the brain-derived neurotrophic factor/TrkB pathway
