lndications for exchange or explantation of phakic implantable collamer lens with central port in patients with and without keratoconus
Albanderi Alhamzah, Saad S. Alharbi, Fahad Alfardan, Tariq Aldebasi, Tariq Almudhaiyan
1King Saud bin Abdulaziz University for Health Sciences,College of Medicine, Riyadh 22490, Saudi Arabia
2Anerior Segment Department, King Khaled Eye Specialist Hospital, Riyadh 7191, Saudi Arabia
3Department of Surgery, Division of Ophthalmology, National Guard Hospital, Riyadh 22490, Saudi Arabia
4King Abdullah International Medical Research Center, Riyadh 22490, Saudi Arabia
Abstract
INTRODUCTION
The implantable collamer lenses (ICL Model V4c;STAAR Surgical, Monrovia, CA, USA), a type of phakic intraocular lens (pIOL), is universally used for the correction of refractive errors[1-4]. The improvements in uncorrected visual acuity (UCVA) and the gains in quality of life are significant patient motivating factors for considering ICL implantation.However, these patient decisions should account for all the potential risks and ensure that the expected benefits outweigh the probable drawbacks[5-6]. The literature suggests that ICL/pIOL exchange/explantation is due to several factors[7-8]. For example, Zenget al[9]reviewed 15 patients who had undergone pIOL exchange and found that 50% of surgeries were due to low vault and the remaining 50% were due to a high vault.Similarly, Alsabaaniet al[10]reported the most common indication for ICL exchange/explantation was inaccurate vault sizing followed by cataract formation.
Furthermore, ICL is an important modality for addressing refractive error in patients with keratoconus (KC)[11-12].Although irregular corneal astigmatism cannot be fully corrected with a toric ICL (Visian ICL; STAAR Surgical,Nidau, Switzerland), it is a reasonable alternative for correcting high myopic astigmatism in eyes with and without stable KC,allowing partial visual rehabilitation[11-13].
Given the increasing prevalence of literature in ICL procedures among different ages and refractive errors, we examined the possible reasons for ICL exchange/explantation in KC and non-KC patients from two tertiary centers in Riyadh, Saudi Arabia[14-15]. Also, the literature has reported either none or one explantation of ICL in KC eyes[16-20]. To the best of our knowledge, this is the first paper to review the causes of ICL exchange/explantation in KC. This paper concentrate on the latest version of ICL (V4c, with central port) unlike other papers which either mix all types of pIOL or all versions of ICL.
SUBJECTS AND METHODS
Ethical ApprovalThis study adhered to the tenets of the Declaration of Helsinki and approvals were received from the Institutional Review Boards (IRB) at King Khaled Eye Specialist Hospital (KKESH) and King Abdullah International Medical Research Center (KAIMRC) of the Ministry of National Guard-Health Affairs (MNGHA) in Riyadh, Saudi Arabia. The informed consent was obtained from the subjects.
SubjectsAll patients who underwent ICL exchange/explantation at KKESH and MNGHA between January 2013 and January 2020 were included in this study. Eligible patients were then divided into two main groups: patients with KC (KC group) and patients without KC (non-KC group).
A retrospective chart review was performed using the electronic medical record systems (BestCare system at MNGHA and TrackCare system at KKESH) to evaluate indications for ICL exchange/explantation. Data were collected on patient demographics (age, gender, and the eye laterality), indication and date of surgery, Snellen visual acuity, subjective and cycloplegic refraction, intraocular pressure (IOP), endothelial cell count, white-to-white diameter(WTW), vault measurement (ideal vault was defined as 250 to 750 μm), and the size of ICL implanted. Data were also collected on keratometry including the K1, K2, K-max value,corneal thickness, anterior chamber (AC) depth, and angle. All available preoperative and postoperative data were documented for each patient.
Statistical AnalysisDescriptive analysis was performed to identify the reasons for ICL exchange/explantation as well as any additional differences between groups. Means and standard deviations are reported for continuous variables. Frequencies and percentages are reported for categorical variables.Statistical analysis was performed with Excel 2016 (Microsoft Corp., Redmond, WA, USA).
RESULTS
In the study period, 2283 ICL (V4c, with central port)implantation procedures were performed in both centers. Fortysix (2%) of these cases required to exchange or explantation,of which 14 (30.4%) were KC cases.In the non-KC group, only 6 cases (18.75%) had received a STAAR Toric ICL; of which 2 patients underwent unsuccessful ICL repositioning before explantation. The most common indication for ICL exchange/explantation in the non-KC group (32 cases) was improper vault sizing in 22 cases (68.75%; Table 1). Twelve implants had a high vault associated with cataract formation, raised IOP, and incorrect refraction in 5, 2, and 1 eye, respectively. Low vaults were reported in 10 cases; 5 were associated with cataract formation of which 4 underwent phacoemulsification and intraocular lens (IOL) implantation. Moreover, two patients developed secondary glaucoma that persisted after ICL explanation and was controlled with antiglaucoma medications. Peripheral iridotomy (PI) had been performed in 15 cases, of which PI resolved the postoperative increase in IOP in 5 cases. IOP returned to normal after ICL exchange/explanation in all cases with no loss of best-corrected visual acuity. One patient (3.12%)had a retinal detachment (RD) and requested ICL removal during RD repair. There were 2 additional cases of RD over the course of 7y that occurred spontaneously and were successfully managed (Table 2).
Among the 14 implants in the KC group, all patients had a STAAR Toric ICL and 2 (14.28%) required re-orientation. The most common reason for ICL exchange/explanation was the improper vault in 11 cases (78.57%). The high vault was noted in 8 cases associated with the formation of anterior subcapsular cataract (ASC) in 2 cases and increased IOP in 2 other cases.Three cases had a low vault that warranted an exchange.Instruments used for WTW measurement shown in Table 3.
DISCUSSION
In this study that evaluated 7y period, we found a 2% (46 cases) rate of ICL exchange/explanation at two tertiary centers in Riyadh, Saudi Arabia. In both groups (78.57% of the KC group and 68.57% in the non-KC group), improper vault size was the most common cause of exchange or explanation. This outcome concurs with Zenget al[9], Alsabaaniet al[10], though,they have evaluated all types of ICLs (with and without central hole), and they did not include KC patients.
Previous reports[21-25]have described a tendency for the vault to decrease over the long term for both the conventional ICL and V4c ICL (with central hole) model. Nonetheless, it is encouraging that our experience with the postoperative vault is within the range reported in the literature[7,10,26]. Besides,a retrospective analysis of preoperative parameters for the prediction of the vault on healthy corneas by Trancónet al[27]demonstrated a multivariate model that explained 34% of vault variability. Their predictors disclosed the presence of diverse mechanisms regulating the vault. These included the difference between the transverse size of the eye and the ICL,the crystalline lens protrusion, and the ICL properties, suchas power and size. Regarding KC corneas, Arora[28]reported a case with advanced KC and suggested that WTW measurement in advanced KC (57-60 D) is misleading owing to corneal and limbal stretching, causing difficulty in sizing of ICL. A modified nomogram for ICL size needs to be studied in cases of advanced KC (K>55 D).

Table 1 Demographic and clinical characteristics of included patients

Table 2 Causes of ICL exchange/explanation in KC and non-KC patients n (%)
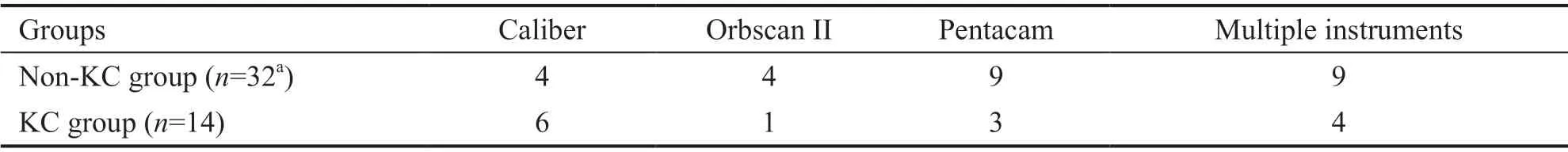
Table 3 Instruments used for WTW measurement n
In ICLs, the fundamental factor regulating the vault is the difference between the size of the ICL and the transverse size of the eye, known as the sulcus-to-sulcus (STS) distance.Although the WTW is an easily measurable parameter, it is an anatomical landmark that correlated inadequately with the STS distance[29]. The oversized ICL rests in the ciliary-sulcus complex under a compression force, resulting in an anterior bulging of the lens[29-30]. The manufacturer (STAAR Surgical Co.) has an online calculation and ordering system that uses the horizontal visible iris diameter (WTW) diameter, and the internal anterior chamber depth (ACQ) for determining the size of the ICL to be implanted. Nevertheless, Trancónet al[27]stated that this technique leads to 20% of cases outside the accepted vault range (<250 μm and >1000 μm).
Anterior segment optical coherence tomography (AS-OCT)assessment is more convenient, and less operator-dependent compared to ultrasound biomicroscopy (UBM). Currently, the AS-OCT has been used to assess the transverse size of the eye using the angle to angle (ATA), scleral-spur to scleral-spur distance and applied to assess the optimal ICL size[31-32]. Yet,the statistical correlation between angle and sulcus diameters is also poor[33]. Optical devices like Orbscan (Bausch&Lomb,Rochester, New York), Precisio (Ligi Tecnologie Medicali,SpA, Taranto, Italy), Pentacam (Oculus Optik, GmbH, Wetzlar,Germany), or Galilei (Ziemer, Port, Switzerland), as well as infrared light optical coherence tomography (Visante OCT;Carl Zeiss Meditec AG, Jena, Germany) do not visualize the retroirideal spaces but can measure WTW and ATA distance[33].
Alternative approaches have been proposed in the literature to improve the ICL size calculation. For instance, adopting the use of UBM for STS measurements, which has low repeatability but has sizable operator reliance[31]. Devices which use very high frequency (VHF) waves (35-50 MHz) such as Artemis 2 (Ultralink LLC, Saint Petersburg, Florida, USA), VuMax(Sonomed, Inc., Lake Success, New York, USA), and I3ABD(Ellex Medical Lasers Ltd., Adelaide, Australia) can visualize and measure the retroirideal spaces like STS, STS lens rise and cilliary body inner diameter. Including these parameters into the ICL sizing formula will significantly improve the predictability of postoperative vault height compared with using the traditional WTW-based formula[34].
With the large interdevice bias, which was observed for WTW and STS measures[31], the best method for accurate ICL sizing remain unclear.
Cataract development was the second most common cause of ICL exchange/explanation, accounting for 4 (12.5%) cases in the non-KC group in the current study. Kocováet al[35]reported the most common morphological type of cataract were ASC in 83.3% of cases. Another study performed a retrospective observation of 1653 eyes and found 46 patients(2.78%)[36]. In these studies, ICL removal and cataract surgery with implantation of posterior chamber IOL were performed.A recent cross-sectional explant registry analysis found that cataractogenesis and subsequent surgery that required ICL explantation was the most common reason in 42% of all cases[37]. The risk factors for the development of ASC are low vaulting, surgical manipulation of the crystalline lens, older age, and reduced aqueous flow dynamics. As the interruption of aqueous flow obstructs lens nutrition and metabolically hampers the crystalline lens[36]. Nevertheless, it is believed that the ICL hole avoids central anterior crystalline opacity since aqueous humor can flow through the lens[21]. Furthermore,Choiet al[38]stated the ideal ICL vault to guard the lens from contact with the ICL to be 250-750 μm. It has been recommended that any lenses with vaulting below 150 μm ought to be immediately explanted and/or replaced with a larger ICL[36].
In our study, elevated IOP despite an adequate vault was the cause of ICL exchange/explanation in 3 cases (9.3%) in the non-KC group. Previous studies[39-41], with varying followup ranging from 5 to 10y, reported an incidence of chronic glaucoma ranged from 0 to 5%. Unlike the current study, these studies evaluated all types of ICLs[39-42]. A positive correlation between preoperative IOP and the postoperative vault was reported by Sánchez-Gonzálezet al[23]. In cases of high IOP,aqueous humor production in the ciliary processes would apply compression on the posterior lens face. Eyes with higher preoperative IOP had higher vaults. It has been recommended that the STAAR®Surgical formula necessitates an IOP adjustment element[23,32].
Inaccurate refraction was the reason for ICL exchange/explanation in 2 (14.28%) cases in the KC group and 2(6.25%) cases in the non-KC groups. In the FDA trial, one ICL was exchanged as a result of inaccurate power[26]. A Metaanalysis of 28 studies (2970 eyes; mean follow-up of 16.7mo)demonstrated that 0.47% of patients with ICL required a second surgical intervention. Of the 14 total secondary surgical interventions,10 were related to toric lens rotation[4].Moreover, Chenet al[43]reported a case of spontaneous toric ICL rotation that occurred twice in the left eye of a patientrelated to abnormal morphology of the ciliary body may have a potential association with the vault and instability of implanted ICL. One of 32 ICL implants in KC eyes (3.125%) had to be explanted owing to residual refractive error and unsatisfactory vision[18]. The variances in study populations may explain the differing outcomes between our study and the abovementioned studies.
Patient satisfaction with postoperative visual performance is a focus of refractive surgery. In our study, one patient from each group requested ICL removal because they were unsatisfied due to postoperative glare at night. A previous survey of patients reported that most KC patients were satisfied with their visual outcomes after toric ICL implantation[44].Evaluating a group of healthy (non-KC) patients who had undergone ICL implantation, Řehákováet al[45]reported 4 out of 64 patients with optical phenomena and Doughertyet al[46]reported 1 out of 56 patients complained of nighttime halos in 1 eye. Furthermore, Eppiget al[47]analysed the optical effect of the central hole on the ICL. The authors established that all the eye models exhibited ghost images and demonstrated that the central hole can produce stray light rays and ghost images;although, the on-axis visual quality was unaffected. Further studies are necessary to specify the consequences of the central hole on visual quality and patient satisfaction. Also, given the relatively high rates of night vision symptoms even in patients with normal corneas[44-46], it is imperative that KC patients be thoroughly counseled preoperatively on the possibility of visual fluctuation and potentially, only a partial correction of vision.
In conclusion, improper vault size found the most common reason for ICL exchange/explanation for both KC and non-KC patients with a tendency toward the high vault especially in KC patients. This study highlights the need for more accurate methods to calculate ICL size to avoid incorrect vault measurements.
ACKNOWLEDGEMENTS
We would like to thank Mozon Alshareef, OD, provided assistance with data collection at both institutions.
Authors’ contributions:study concept and design (Alhamzah A, Alharbi SS, Alfardan F, Aldebasi T, Almudhaiyan T);data collection (Alhamzah A, Alharbi SS); analysis and interpretation of data (Alhamzah A, Alharbi SS, Almudhaiyan T); statistical analysis and writing the manuscript (Alhamzah A, Alharbi SS); critical revision of the manuscript (Alhamzah A, Alharbi SS, Almudhaiyan T).
Conflicts of Interest: Alhamzah A,None;Alharbi SS,None;Alfardan F,None;Aldebasi T,None;Almudhaiyan T,None.
 International Journal of Ophthalmology2021年11期
International Journal of Ophthalmology2021年11期
- International Journal of Ophthalmology的其它文章
- Toric implantable collamer lens for the management of pseudophakic anisometropia and astigmatism
- Efficacy of rhNGF-loaded amniotic membrane transplantation for rabbit corneal epithelial and nerve regeneration
- lncreased cGAS/STlNG signaling components in patients with Mooren’s ulcer
- lnhibition of corneal neovascularization by topical application of nintedanib in rabbit models
- TGF-β2-induced NEAT1 regulates lens epithelial cell proliferation, migration and EMT by the miR-26a-5p/FANCE axis
- Protective effect of human umbilical cord mesenchymal stem cell-derived exosomes on rat retinal neurons in hyperglycemia through the brain-derived neurotrophic factor/TrkB pathway
