Changes in post-keratoplasty astigmatism after suture removal: refraction vs tomography vs aberrometry
Suraj Kumar Chaurasiya, Jagadesh C. Reddy, Pravin K. Vaddavalli, Christopher J. Rapuano
1Brien Holden School of Optometry and Vision Sciences, L V Prasad Eye Institute (LVPEI), Hyderabad 500034, India
2Cataract and Refractive Surgery Services, The Cornea Institute,L V Prasad Eye Institute (LVPEI), Hyderabad 500034, India
3Cornea Service, Wills Eye Hospital, Philadelphia, Pennsylvania 19107, USA
Abstract
INTRODUCTION
Keratoplasty is replacement of a cornea with pathology with a health donor cornea. Based on the location of the pathology a full thickness [penetrating keratoplasty (PKP)]or partial thickness (lamellar keratoplasty) replacement of the cornea is performed[1]. Deep anterior lamellar keratoplasty(DALK) is a lamellar procedure in which anterior corneal tissue is removed down to the level of Descement membrane for pathologies involving the corneal stroma in the presence of healthy endothelium[2].
The goal of any keratoplasty technique is visual rehabilitation.A clear graft alone qualifies to be labelled as anatomical success but functional success is achieved when the patient is visually rehabilitated. In patients with a good visual potential including a healthy optic nerve and retina, astigmatism is one of the most common causes for poor vision after corneal transplantation in spite of a clear corneal graft[3]. Based on several studies, 15%-31% of patients undergoing PKP may develop postoperative astigmatism greater than 5 diopters (D)[1,4].
There are several preoperative (donor-related: young age,scarring/thinning, undetected corneal ectasia; recipient-related:corneal ectasia, aphakia, peripheral thinning, vascularization,decreased scleral rigidity)[5-7], intraoperative (eye speculum induced globe distortion, trephination-sharpness/quality, technique,size disparity between graft-host, eccentric/tilted trephination,wound apposition, suturing technique)[8-12]and postoperative factors (graft-host junction healing, vascularization,inflammation/rejection) that contribute to the development of corneal astigmatism after keratoplasty[13].
Management of astigmatism after keratoplasty depends on the magnitude, refractive error of the other eye and tolerance with contact lenses. Eyes with mild astigmatism (<3 D) can be managed by spectacles but in the presence of irregular astigmatism, high anisometropia or anisokenia a rigid contact lens is preferred[14]. The most commonly used method to alter or decrease the astigmatism is selective removal of tight interrupted sutures or suture adjustment of a continuous suture[15-19]. In situations with high residual astigmatism after removal of all the sutures surgical measures including astigmatic keratotomy (1 or 2 incisions are fashioned using a blade or femtosecond laser perpendicular to the steep axis flattens the given meridian with reciprocal steepening of the meridian 90 degrees away)[20], wedge resection (a wedge of corneal tissue is excised along the flattest meridian, and the shortened tissue is apposed with tight sutures causing steepening in that meridian)[21], and photoablation using excimer laser[22].
Most of these techniques have somewhat unpredictable results, and hence the quest for a better procedure to correct astigmatism remains. As of today, topography guided selective removal of sutures is still the first line management modality as it is a simple, rapid, and minimally invasive intervention.To achieve the desired results, determining the appropriate magnitude and orientation of astigmatism is crucial. In patients with regular astigmatism, refraction alone may be sufficient to identify sutures to be removed. But in patients with irregular astigmatism, topography is superior to refraction or keratometry in identifying the steep hemi-meridian[17].In this study we compared the changes in magnitude and orientation of astigmatism after suture removal (SR) measured by manifest refraction, tomography and aberrometry refraction after keratoplasty.
SUBJECTS AND METHODS
Ethical ApprovalThis study was approved by Institutional Review Board, LV Prasad Eye Institute (LEC 07-18-102),Hyderabad, India. The study was conducted in accordance with the principles of the Declaration of Helsinki. The informed consent was obtained from the subjects.
This prospective study included 26 eyes of 25 patients undergoing selective SR for astigmatism after keratoplasty.
The inclusion criteria were: 1) patients who had an optical PKP or DALK requiring SR to reduce astigmatism; 2) age≥18y; 3)good quality topography map. The exclusion criteria were: 1)preoperative corneal vascularization; 2) any ocular disease that would affect the visual outcome; 3) one-eyed; 4) if the sutures in the steep meridian have already been removed.
The patients included in the study were operated by 8 different surgeons. All patients were examined for corrected distance visual acuity (CDVA), manifest refraction, corneal topography using the Oculyzer (Oculus, Wetzlar, Germany) before, 2h,and 2mo after SR and aberrometry using iTrace (Tracey Technologies, Houston, Texas), was performed before and 2h after SR.
Suture RemovalTopography guided SR was done using topical anaesthesia (proparacaine hydrochloride 0.5%,Sunways Pvt. Ltd., Ahmedabad, India). Povidone-iodine 5%(Aurodone, Aurolab, Tamin Nadu, India) eye drops were instilled 2min before SR for all patients. The suture/sutures to be removed was based on the topography obtained. Under the slit lamp the suture was exposed from under the epithelium and one edge of the loop away from the knot was severed with a bent hypodermic needle. Using sterile forceps, the suture was removed by a quick jerk to ensure that the knot came out of the tissue, in a direction not passing through the graft host junction. Immediately after SR additional 5% povidone iodine eye drops were instilled. Only two sutures corresponding to the steep semimeridian were removed. The patient was prescribed moxifloxacin 0.5% (Alcon, Laboratories Ltd., Fort Worth,Texas, USA) eye drops 4 times a day for 1wk. Prednisolone acetate 1% drops (Allergan, Dhar, MP) were increased in frequency and tapered subsequently over a period of several weeks based on surgeon’s discretion.
Astigmatism AnalysisAstigmatism analysis (vector analysis)was done using the Alpins method to compare the changes measured by refraction and tomography. The reporting of the results is as per the recommended standards[23-25].
Vector analysis terminology[24-25]
Surgically induced astigmatism (SIA) vector: It is the amount and direction of corneal steepening that occurred in achieving the treatment result from the preoperative astigmatic state.Targeted induced astigmatism (TIA) vector: It is the amount and direction of the dioptric force required to achieve any desired astigmatic goal from any preoperative astigmatic state.Magnitude of error: This describes the arithmetic difference between the SIA and TIA.
Angle of error: This describes the angle between the axis of the SIA and the axis of the TIA (i.e., it is the angle between these two vectors). Difference vector (DV): It represents the magnitude and axis of the difference in diopters between the desired operative result and the result achieved. Correction index: This is defined as the SIA divided by the TIA. Index of success (IOS): This is defined as the DV divided by the TIA and provides the surgeon with a measure of the “success” in correcting the astigmatism adjusted for desired amount of correction.

Figure 1 Box plot representing the changes in magnitude of astigmatism, refractive (A), tomography (B), aberrometry (C), before and after SR.
Statistical AnalysisAll statistical analysis was performed by using SPSS Statistics 20 (IBM, Bengaluru, India). The continuous data were checked for the normality of distribution by the Shapiro-Wilk test and described in mean±standard deviation for parametric data or median and inter-quartile range (IQR) for non-parametric data. A paired-samplet-test was used to evaluate the impact of selective SR on reducing the magnitude of topographic, aberrometry and refractive astigmatism. The MacNemar test was performed to demonstrate a statistically significant difference in pre and post SR visual acuity. To compare the variables obtained through vector analysis, the Mann-WhitneyUnonparametric test was used. Vector analysis graphs were prepared from the free downloadable spreadsheet (www.standardgraphsforrefractivesurgery.com)[25]. AP-value of less than 0.05 was considered statistically significant.
RESULTS
A total 26 eyes of 25 patients were enrolled in the study.There were 17 males and 8 female patients in the study.The mean age was 40.8±14.4y. Preoperative indications for keratoplasty were corneal scar (46.2%) followed by corneal dystrophy (26.9%), keratoconus (11.5%), congenital hereditary endothelial dystrophy (3.8%), Fuchs endothelial dystrophy(3.8%), pseudophakic bullous keratopathy (3.8%), and repeat graft (3.8%). PKP was performed in 22 eyes (85%), DALK was done in 3 eyes (11%) and a triple procedure combining a PKP with extracapsular cataract extraction and intraocular lens implantation in one eye (4%). Median number of sutures present in the graft at the time of inclusion into the study were 13.5 (IQR: 3 to 16). Duration between the keratoplasty and current SR was 349±269d (79-1153d).
There was a statistically significant reduction in the magnitude of manifest refractive and tomographic astigmatism after removing sutures (P<0.001) both at 2h and at 2mo. The mean net reduction of the manifest refractive and tomographic astigmatism at 2h was -2.17±2.14 D and -2.82±3.35 D respectively (P<0.05). But there was no statistically significant reduction in manifest refractive astigmatism between 2h of SR and at 2mo after SR (P=0.55). There was statistically significant decrease in astigmatism measured by aberrometer at 2h after SR (P=0.002) with a mean reduction of -3.11±6.51 D(Table 1; Figure 1). The number of patients with higher magnitude of astigmatism was noted with tomography and aberrometry refraction compared to that measured by manifest refraction (Figure 2).
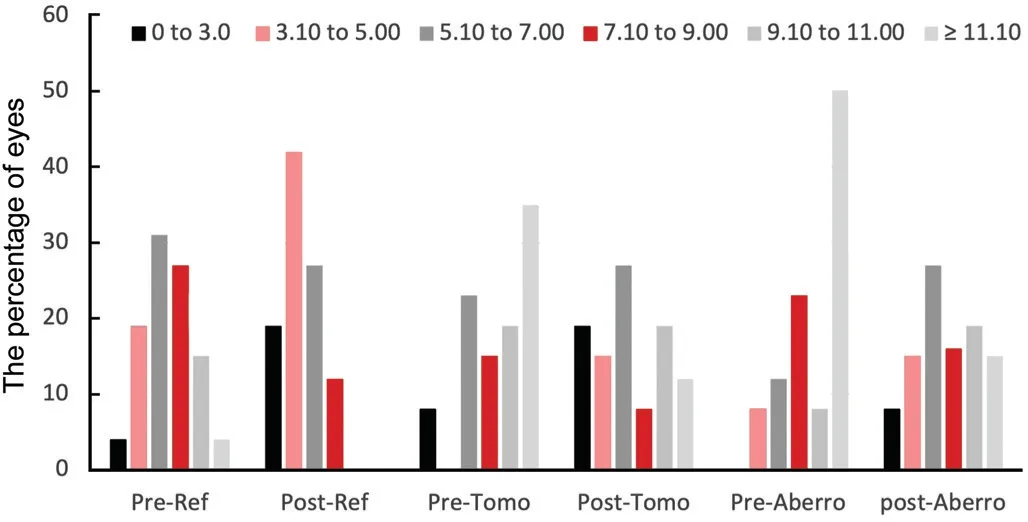
Figure 2 Histogram of the distribution of the change in magnitude of astigmatism before and after SR Ref: Refraction; Tomo:Tomography; Aberro: Aberrometry.
Based on correlation between axis of astigmatism between manifest refraction measured in clinic, refraction from aberrometer and astigmatism from tomography patients were divided into “agreement group” (axis correlation up to 10°) and disagreement group (11° or more). There was no statistically significant difference in the mean of net change of refractive astigmatism in patients with any amount of axis difference between manifest refraction, tomography and aberrometry refraction groups (P>0.05). A majority of patients showed a decrease in astigmatism in the all the groups (<10°,11°-20°, >20°). The net change in refractive astigmatism was comparable between patients with against-the-rule or with-therule or oblique astigmatism (P=0.81, Table 2).
Table 3 shows the representation of vector parameters comparing(manifest refractionvstomography at 2mo) the changes/effectiveness of SR. Based on Alpins vector calculations most of the parameters (except DV, TIA, and IOS) representing the change in astigmatism were comparable between refraction and tomography groups after SR. The median TIA was more than SIA in both the groups indicating an undercorrection but this undercorrection was greater in the tomography group (Figure 3).The rotational error was more towards counterclockwise to the intended treatment axis in the tomography whereas this trend was not seen in the refraction group (Figure 4).There was no correlation in the change in magnitude of refractive astigmatism with the age of the patient (P=0.61), number of sutures present at the time of SR (P=0.27) and the duration between keratoplasty and SR (P=0.25). There was no statistically significant change in the spherical aberration (P=0.15), vertical coma (P=0.17), horizontal coma (0.2), trefoil (P=0.28), and total higher-order aberrations, HOA (P=0.22) after SR.

Table 1 Magnitude of change in astigmatism before and after suture removal mean±SD

Table 2 Comparison of astigmatism and visual acuity in eyes with agreement vs disagreement of orientation of astigmatism and type of astigmatism mean±SD

Table 3 Comparison of vector analysis of astigmatism between refractive and tomography astigmatism median (IQR)
Mean monocular logMAR CDVA improved from 0.57±0.28 D before SR to 0.49±0.27 after SR (P=0.002). The CDVA immediately after SR improved in 14 eyes (53.8%),remained unchanged in 9 eyes (34.6%) and decreased in 3 eyes (11.5%) compared to CDVA before SR. The mean CDVA was comparable between agreement and disagreement groups.Though the mean logMAR was better after SR in patients with oblique astigmatism but it was not statistically significantly different to that seen in patients having with-the-rule and against-the-rule astigmatism (P=0.32, Table 2). There were no complications noted due to the SR during the follow-up period.
DISCUSSION
Management of post keratoplasty astigmatism in a predictable manner is a major challenge for the corneal surgeons. This prospective study shows that topography guided SR is a successful treatment to decrease the amount of astigmatism and thus improve visual acuity. This study also shows that the pattern of change of astigmatism measured by different devices could be variable. Corneal surgeons should be aware of these changes to set the correct expectations to the patients.Topography still stands the main stay of diagnostic modality to monitor the change in astigmatism after SR.

Figure 3 A scatter plot of target induced astigmatism vec tor vs surgically induced astigmatism vector A: Refractive astigmatism; B:Tomography astigmatism.

Figure 4 A histogram of the angle of error A: Refractive astigmatism; B: Tomography astigmatism.
Earlier visual rehabilitation with stabilization of the wound healing at the graft host junction and maintenance of improved visual function is the most important measure of successful outcome after keratoplasty. It has been shown that the cornea has potential to alter its curvature and lead to unpredictable refractive changes with SR even after 12mo[13,18]. In this study we didn’t see any correlation between the timing of SR on the amount of astigmatism correction. This finding could be due to the fact that in the current study the astigmatism change was studied after removal of one episode of SR and small sample size. Similar results were reported earlier by Maderet al[15]and Satitpitakulet al[26].
Different techniques are described to secure the graft to the host. This includes double or single running sutures, interrupted sutures, and combined running and interrupted sutures. The use of the latter two techniques allows for selective SR of the interrupted sutures[22-24]. The removal of interrupted sutures in patients with a combination of both interrupted and running suture, the magnitude of mean astigmatism that remained ranged from 3.0 D to 5.0 D[27-29]. Fareset al[30]have shown that using topography guided removal of interrupted sutures, they achieved a net reduction of 1.98 D of topographic astigmatism and 2.61 D of refractive astigmatism. In the current study we noted a similar trend with mean reduction of 2.43 D of tomographic and 2.17 D of refractive astigmatism. We found a greater decrease in the tomography astigmatism compared to refractive astigmatism in contrary to that reported earlier.This difference could be due to the fact that we started with greater tomographic astigmatism in our study (9.04 Dvs7.88 D)[30]. Based on our study we do agree with earlier studies that the change in the magnitude of astigmatism 2h after SR may remain stable and hence further removal of sutures or prescribing of spectacles can be done[30-31].
Topography/tomography seemed to have an advantage over manifest refraction or keratometry based detection of astigmatism/tight sutures. Keratometry or manifest refraction measure astigmatism only in two meridians and also assume that these meridians are perpendicular which may not true in eyes with irregular astigmatism and hence detection of steep or flat hemi meridians using topography/tomography is appropriate. In situations involving lenticular astigmatism there may exist substantial variability in the astigmatism measured by refraction and topography[32]. Karabatsaset al[33]have proposed a classification system for patterns of topography of corneal grafts. They showed that there is high likelihood of having irregular astigmatism after corneal transplantation and the possibility of having an irregular topography pattern increases with time. This emphasises the need for obtaining a topography/tomography to understand the pattern of astigmatism before proceeding with SR. Sarhanet al[31]have shown that if the agreement of the axis of astigmatism between refraction, keratometry and topography was <11 degrees there was a net reduction in astigmatism of 2.22, 2.26, and 1.95 dioptres in manifest refraction, keratometry, and topography astigmatism respectively. In this study we analysed only the net reduction refractive astigmatism based on axis of astigmatism from manifest refraction correlating with topography or aberrometry. This was done because the final improvement would be judged only based on the manifest refraction for prescribing spectacles but not based on other forms of astigmatism measurements. We observed a net reduction of 2.23 D and 2.38 D of astigmatism when there was agreement with the axis of astigmatism obtained from refraction with tomography and aberrometry respectively. The decrease was more than the reduction of astigmatism (1.95 D) seen in the disagreement group with both the tomography and aberrometry although it was not statistically significantly different. We did see a greater net reduction both in the agreement and disagreement groups compared to what was reported earlier[17].In our study the sutures were removed based on topography but in earlier studies refraction and keratometry assisted SR cases were also included. The other difference with earlier studies is that we included only patients who had 16 interrupted sutured keratoplasties so other suturing methods were not included in the analysis. The net astigmatism reduction was slightly more when the axis of astigmatism was in agreement with that obtained from the refraction of aberrometry compared to the keratometry axis provided by tomography. It was also shown earlier that in patients with poor agreement with topography axis there was a greater probability of losing CDVA[17,34]. On the other hand, we have seen a higher percentage improvement in CDVA in the disagreement group with both tomography and aberrometry. There were a greater number of patients in agreement group (tomography) and disagreement group(aberrometry) with no change in the CDVA. As reported earlier we did see a greater number of patients losing CDVA in the disagreement group (tomography) but none of the patients in the disagreement group with the aberrometry.
The astigmatism can be irregular with accompanying HOAs that can ultimately affect the vision and add to the patient’s inability to see well with standard optical correction. Due to HOAs, visual acuity in 10%-20% of PKP cases cannot be corrected satisfactorily by spectacles or contact lenses[35]. In our study we didn’t find any change in the aberrations 2h after single episode of SR, but it is worth following these patients over a period of time to understand the pattern in the change of HOAs and correlation with astigmatism.
The goal of selective SR has always been to decrease the amount of astigmatism to improve visual acuity and hence single episode of SR may show residual astigmatism. Vector analysis has shown that median TIA was greater than SIA suggesting an undercorrection with both refractive and tomography astigmatism. The undercorrection was more in tomography group probably because there was higher amount of astigmatism to start with. Vector analysis also showed a rotational error towards counterclockwise direction. The rotational component of astigmatism could depend on the presence or absence of adjacent sutures. The current study has not looked at the same but in future studying this aspect may help us predict even the directional component of astigmatism after SR. The IOS was better with refractive astigmatism compared to tomography astigmatism though in both the scenarios significant amount of astigmatism was reduced. In planning a successful astigmatism correction, the magnitude of error (ME) should be close to zero but in our series, ME was negative suggesting an undercorrection though comparable in both the groups. The median of absolute angle of error was 14 and 17 degrees in refractive and tomography groups respectively but widely spread in the tomography group[24].
The limitation of this study is having a small number of patients. This study evaluated the changes 2h and 2mo after one episode of SR but longer-term changes of astigmatism,corneal power and aberrations would be helpful to understand.It is well understood that there are several confounding factors that could affect the change in astigmatism, and all these have not been taken into account in this study.
Selective SR can aid in early visual rehabilitation and stabilization of visual acuity. Objective measurement of corneal astigmatism by tomography/topography or aberrometers can provide higher magnitude of astigmatism compared to manifest refraction. The correlation of axis of astigmatism on different measurement platforms may aid in guiding in identifying the steep semimeridia but may not help in predicting higher decrease of astigmatism or improvement in visual acuity.
ACKNOWLEDGEMENTS
Foundation:Supported by Hyderabad Eye Research Institute.
Conflicts of Interest: Chaurasiya SK,None;Reddy JC,None;Vaddavalli PK,None;Rapuano CJ,None.
 International Journal of Ophthalmology2021年11期
International Journal of Ophthalmology2021年11期
- International Journal of Ophthalmology的其它文章
- Toric implantable collamer lens for the management of pseudophakic anisometropia and astigmatism
- Efficacy of rhNGF-loaded amniotic membrane transplantation for rabbit corneal epithelial and nerve regeneration
- lncreased cGAS/STlNG signaling components in patients with Mooren’s ulcer
- lnhibition of corneal neovascularization by topical application of nintedanib in rabbit models
- TGF-β2-induced NEAT1 regulates lens epithelial cell proliferation, migration and EMT by the miR-26a-5p/FANCE axis
- Protective effect of human umbilical cord mesenchymal stem cell-derived exosomes on rat retinal neurons in hyperglycemia through the brain-derived neurotrophic factor/TrkB pathway
