Effects of dietary high dose DHA omega-3 supplement in dry eye with meibomian gland dysfunction
Yeon Ji Jo, Jong Soo Lee
Department of Ophthalmology, Pusan National University School of Medicine&Medical Research Institute of Pusan National University Hospital, Busan 49241, Republic of Korea
Abstract
INTRODUCTION
Dry eye disease (DED) is a multifactorial chronic inflammatory condition of the ocular surface that results in ocular discomfort and visual disturbance. The prevalence of DED is estimated at 10.4% of the Korean people[1]. DED is continually increasing due to various factors such as aging,intensive use of computer and smartphone, contact lenses wearing, and corneal refractive surgery[2-3]. The artificial tear is the first choice of treatment for DED, but the symptoms and signs of some DED are not alleviated completely by artificial tears. Thus, the various methods such as using steroid eye drops or autologous serum, punctal occlusion are used for chronic and severe DED. Regardless of the various treatment methods for dry eye existed, many DED patients suffering from chronic discomfort of dry eye.
The leading cause of DED is known due to obstructive meibomian gland dysfunction (MGD). MGD is caused by hyper-keratinization of the ductal epithelium and increased viscosity of meibum, resulting in lipid insufficiency and excessive evaporation and instability of the tear film[4].Actually, omega-3 fatty acids affect dry eye syndrome related with MGD. For example, omega-3 fatty acids induce the change of lipid profile in the meibum, secretion and quality of the meibomian gland, and tear film stability in MGD[5-7]. Omega-3 plays an important role in modulating the inflammatory and immune responses in DED[8]. For example, omega-3 fatty acids block the synthesis of interleukin-1 and tumor necrosis factoralpha associated with dry eye syndrome. However, omega-3 fatty acid is not enough supply by dietary food sources, and dietary supplement of omega-3 fatty acids can be supplied to improve DED symptoms.
While many previous studies reported controversial results as to whether dietary supplementation with omega-3 fatty acids can aid in the treatment of dry eye symptom[9-10]. The U.S Food and Drug Administration (FDA) has established anacceptable daily intake of omega-3 is 3 g (3000 mg) per day under physician’s supervision. Omega-3 fatty acids is mainly composed of two kinds of fatty acid such as eicosapentaenoic acid (EPA) or docosahexaenoic acid (DHA). EPA inhibits the production of prostaglandin, leukotriene, and thromboxane related to inflammatory reactions[11]. DHA which is the final metabolite of omega-3 organizes nerve tissue such as the brain and retina. Also, DHA acts as a storage molecule, so it can be shortened and re-saturated to produce EPA and the antiinflammatory prostaglandins[12]. But recommended dietary allowance dosage for EPA and DHA is still not established,especially in DED. Although DHA influences the nerve tissue especially retina of eye, few products on the market contain higher doses DHA rather than EPA.

Table 1 Korean Corneal Disease Study Group guideline for the diagnosis of dry eye disease[13]
The purpose of this study is to investigate the efficacy of dietary supplementation with high dose DHA omega-3 for treating DED patients in 8wk intervention period.
SUBJECTS AND METHODS
Ethical ApprovalA randomized, double-masked interventional study was performed at one referral eye center from December 2017 to September 2019. This trial was approved by the institutional review boards and the local ethics committee (IRB No.1711-002-060). Written informed consent was obtained from all the participating patients based on the Helsinki protocol. This study is registered with the Korean clinical research information service (KCT0005222).
PatientsOver 18 years old adults, symptoms of DED with MGD patients were included in this study. Patients were checked dietary habits by questionnaire sheet whether high omega-3 food intake regularly or not. The diagnosis of DED was made based on the guideline proposed by the Korean Corneal Disease Study Group (KCDSG; Table 1)[13].
And MGD was diagnosed by slit-lamp examination. The application of digital pressure to the 8 glands of the central third of the lower tarsus on a scale of 0 to 3: 0=clear, 1=cloudy,2=cloudy with debris, and 3=thick like toothpaste (total score range 0-24). In this criterion, moderate MGD patients (score range 8-12) were included. And lid vascularity, plugging of gland orifices, lid margin irregularity and thickening were also assessed to include this study[14].
All patients have no history of having dietary omega-3 supplements from 3 months ago[15]. During the trial period, all participants have prescribed 0.5% carboxymethyl cellulose eye drops (Refresh plus®, Allergan, Dublin, Ireland) four times a day. However, patients were instructed not to use tear supplements, at least 2h before the examination.
Patients were excluded from this study if they met one of the following criteria: a history of diagnosed level IV DED by KCDSG guideline; allergic conjunctivitis, severe ocular infection,and inflammation; ocular surgery in 3mo; systemic (anti-anxiety,anti-histamine, anti-depressant) or topical medications that could affect tear film or meibomian gland function; severe MGD having anatomical changes; allergy to fluorescein®; using contact lens; and current pregnancy or breast feeding.
Randomization, Masking, and Sample Size CalculationTo calculate sample size and compare the mean difference in dry eye symptoms between the omega-3 and placebo groups.Assuming 1:1 randomization, 80% power (alpha=0.05), and a precision error of 5%. The estimated sample size in each group was calculated to be 24 by the G power 3.1 programs. Figure 1 shows the patient flow-chart, randomization schedule, and follow-up protocol. Patients were randomly allocated to one of the two groups by a parallel assignment. High dose DHA omega-3 group received two capsules of Easyeye Dry®(Korea CNS pharm, Seoul, Korea), total containing 600 mg of EPA and 1640 mg of DHA, once a day for 8wk. The placebo group received 3000 mg of olive oil in two capsules, once a day for 8wk. The contents and types of capsules were masked for participant patients.
Outcome MeasuresAll participants were examined by slitlamp examination and dry eye testing at baseline, 4, and 8wk after omega-3 and placebo supplementation. At each visit,assessed MGD score, tear break-up time (TBUT), cornea staining (NEI score) of the ocular surface, tear secretion (SM Tube), and ocular symptoms evaluated by Ocular Surface Disease Index (OSDI).

Figure 1 Flow diagram of this study for the therapeutic effect of dietary omega-3 supplement.
The ocular surface was stained with 2 mL of 1% preservativefree fluorescein solution instilled into the conjunctival sac. The corneal staining was then assessed by fluorescein staining using the NEI score where the area of corneal staining was divided into five areas: superior, nasal, center, temporal, and inferior.The density of corneal staining was graded from 0, when no corneal staining was present, to 1 when corneal staining was sparse, 2 when it was moderately dense, and 3 when the corneal staining was high and the lesions overlapped[16].
TBUT was the interval between the last complete blink and the first disturbance of the stained corneal tear film. Three measurements per subject were made both right and left side,then the average of the three values was taken as the mean value.
Under non-anesthetic conditions, the tip of the strip meniscometry tube (SM tube, Echo Electricity Co., Ltd.,Fukushima, Japan) was immersed in the tear meniscus for 5s under a slit-lamp microscope. The examination was performed while taking care to avoid the test paper touching the ocular surface. The duration of measurement was strictly checked using a timer. The SM Tube value (in millimeters) was measured from the wet length of the test paper for 5s[17].
The OSDI is one of the most frequently used methods to assess DED. In this study, Korean version OSDI questionnaire was used. The translated in the Korean version of OSDI tool reliability was Crohnhach’s α=0.94[18]. This questionnaire comprises 12 questions and evaluates the frequency of symptoms over the preceding week. The questionnaire requires approximately 5min for the patient to complete, and the scores range from 0 to 100. Based on the score, the patient’s symptoms can be categorized as normal (0-12), mild dry eye(13-22), moderate dry eye (23-32), or severe dry eye (33-100)[19].
Statistical AnalysisStatistical analysis was performed using SPSS version 24.0 for Windows (SPSS statistics, IBM). At-test or one-way analysis of variance (ANOVA) test was applied.Thet-test was conducted to investigate the mean differences between the two groups. An ANOVA test was conducted to determine whether there were significant changes in mean test values over the course of the 8wk of intervention. TheP-value of less than 0.05 was considered statistically significant.
RESULTS
Of the 50 included patients, 24 patients were randomized to the high dose DHA omega-3 group and 26 patients to the placebo group. Two patients were lost during the follow-up period. There were 44 females and 6 males were included.Total patients mean age was 63.0±7.7y, the mean age in high dose DHA omega-3 group was 62.0±7.0y, and 63.8±8.4y in the placebo group. As for baseline indices, there was no significant differences in mean age, sex, best corrected distant visual acuity (BCDVA), intraocular pressure (IOP), MGD score, TBUT, NEI score, SM Tube, and OSDI score between two groups (allP>0.05; Table 2).
Meibomian Gland Dysfunction ScoreMGD score was only significantly reduced in omega-3 groups after treatment. In omega-3 group, the MGD score was 8.7±1.5 at the baseline,and 7.2±1.8 (P<0.001) at 8wk after treatment. Regarding to placebo group, the MGD score was 8.6±1.4 at the baseline,and 8.1±2.6 (P=0.162) after 8wk. There were no significant differences in MGD score between the two groups at baseline(P=0.783). But after 8wk of treatment, the omega-3 group MGD score showed more significant improvement than the placebo group (P=0.033; Figure 2).
Tear Break-up TimeMean baseline TBUT in both omega-3 and placebo groups improved significantly after treatment. In omega-3 group, the value of baseline TBUT was 4.13±0.85s.After 4 and 8wk, the value of TBUT were 5.58±1.21 (P<0.001)and 6.00±1.62s (P<0.001). In the placebo group, the value of baseline TBUT was 3.75±0.79s. The value of TBUT were 5.25±1.29s (P<0.001) at 4wk and 5.08±1.28s (P<0.001) at 8wk after treatment. However, the value of TBUT at 8wk wasimproved significantly higher in the omega-3 group, compared to the placebo group (P=0.034; Figure 3).
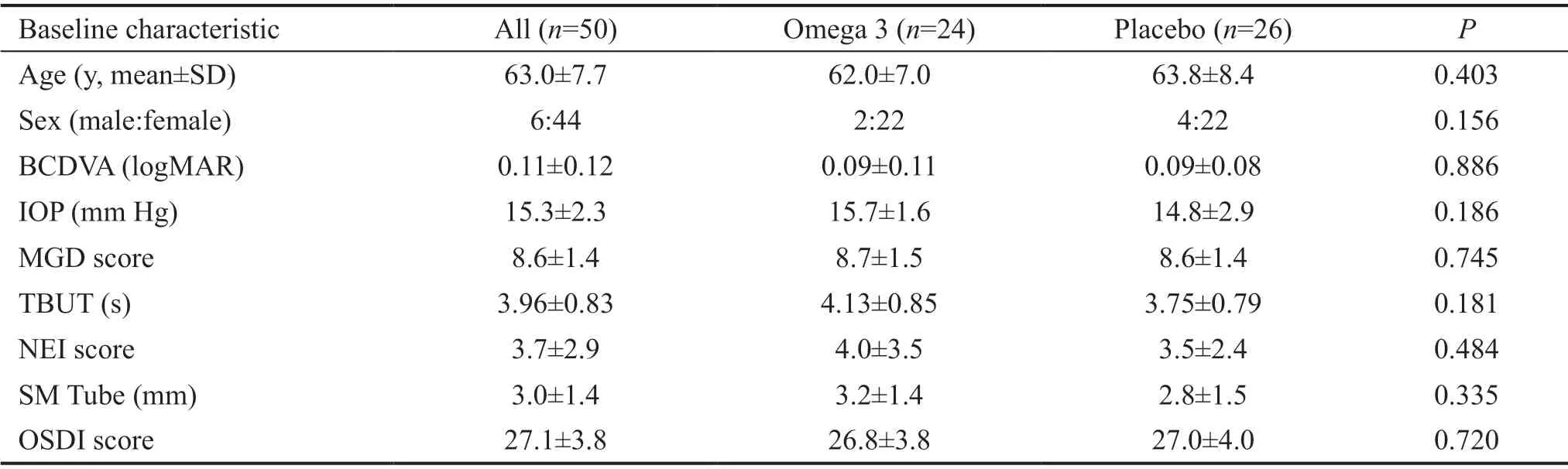
Table 2 Characteristics of patients with dry eye
Cornea StainingNEI score was significantly reduced in both groups after treatment. In omega-3 group, the average NEI score was 4.0±3.5 at baseline, 2.5±2.1 (P=0.013) at 4wk,and 1.4±1.4 (P<0.001) at 8wk. As for the placebo group,the average NEI score was 3.5±2.4 at the baseline, 3.0±2.4(P=0.030) at 4wk, and 1.9±1.5 (P<0.001) at 8wk. However,there were no significant differences in vital staining between two groups at 4 and 8wk after treatment (Figure 4).
SM Tube TestThe mean value of the baseline SM tube in omega-3 group was 3.2±1.1 mm, which changed insignificantly reduced after treatment. The value of SM tube was 2.8±1.1 mm(P=0.071) at 4wk and 2.9±1.5 mm in 8wk (P=0.518). The mean value of the baseline SM tube in the placebo group was 2.8±1.5 mm, which changed insignificantly improved after treatment. The value of SM tube was 2.9±0.5 mm (P=0.811)in 4wk and 3.1±1.1 mm in 8wk (P=0.319). There were no differences in the SM tube between the omega-3 and placebo groups at 4 and 8wk (Figure 5).
OSDI ScoreOSDI score was also significantly reduced in both groups after treatment. In omega-3 group, the value of OSDI score was 26.8±3.8 at the baseline, 24.2±4.2 (P<0.001)at 4wk, and 24.3±4.2 (P<0.001) at 8wk after treatment.Regarding to Placebo group, the value of OSDI score was 27.0±4.0 at the baseline, 25.5±4.1 (P<0.001) at 4wk, and 25.0±4.0 (P<0.001) after 8wk. There were no significant differences in OSDI score between the two groups at 4 and 8wk after treatment (Figure 6).
DISCUSSION
It is known that DED can be aggravated by MGD. This study was conducted to evaluate the treatment effect of high dose omega-3 dietary supplementation in DED patients with MGD. Recently, the composition of omega-3/omega-6 ratio in serum is increased due to changing a dietary habit in Korea.High serum omega-6 level triggers the pro-inflammatory status which could worsen symptoms in DED and MGD.Although oral supplementation of omega-3 could benefit to reduce inflammatory reaction, the direct mechanism of dietary omega-3 supplementation in DED treatment is not fully understood. Although there was controversy in the therapeutic effect by omega-3 supplement, but many previous studies report dietary omega-3 supplement is effective in DED[10-11,20-21].

Figure 2 The outcomes of MGD score after omega-3 and placebo supplementation The MGD score of omega-3 group significantly improved at 8wk after treatment (aP=0.033).

Figure 3 The outcomes of TBUT after omega-3 and placebo supplementation The value of TBUT of omega-3 group significantly improved at 4 and 8wk after treatment, compared to that of control group at baseline of pre-treatment on both groups (compared t-test bP<0.001 in all groups). Especially, the value of TBUT in omega-3 group was significantly more improved than that of control group at 8wk (one-way analysis of variance, aP=0.034).
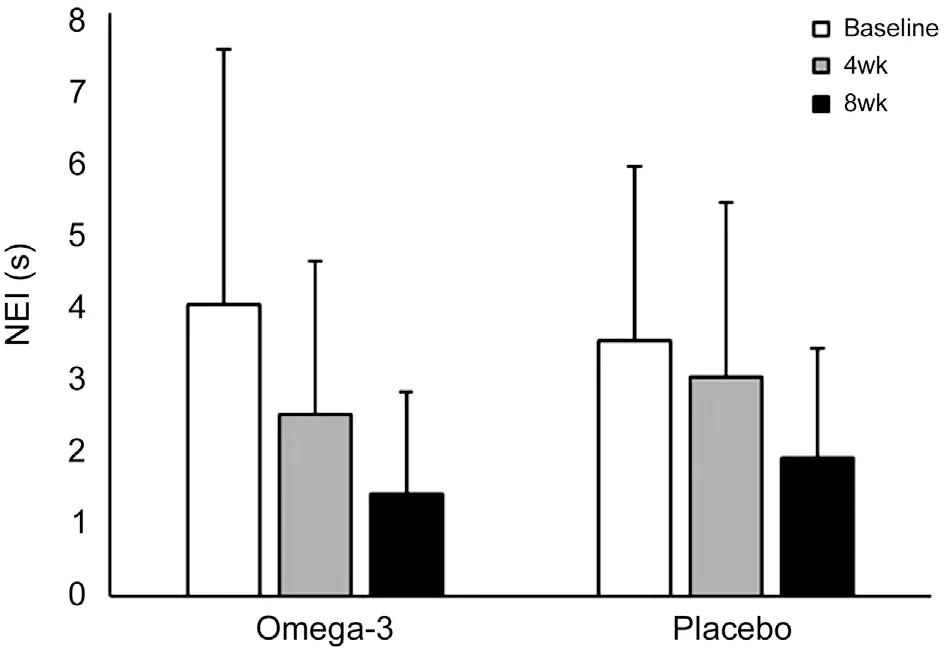
Figure 4 The outcomes of NEI score after omega-3 and placebo supplementation The values of NEI score of omega-3 group and control significantly improved at 4 and 8wk, compared to that of baseline between pre-and post-treatment (compared t-test P=0.013,P<0.001, P=0.030, P<0.001 respectively). The value of NEI score in omega-3 group was not significantly more improved than that of control group at baseline, at 4 and 8wk (one-way analysis of variance,P=0.034).
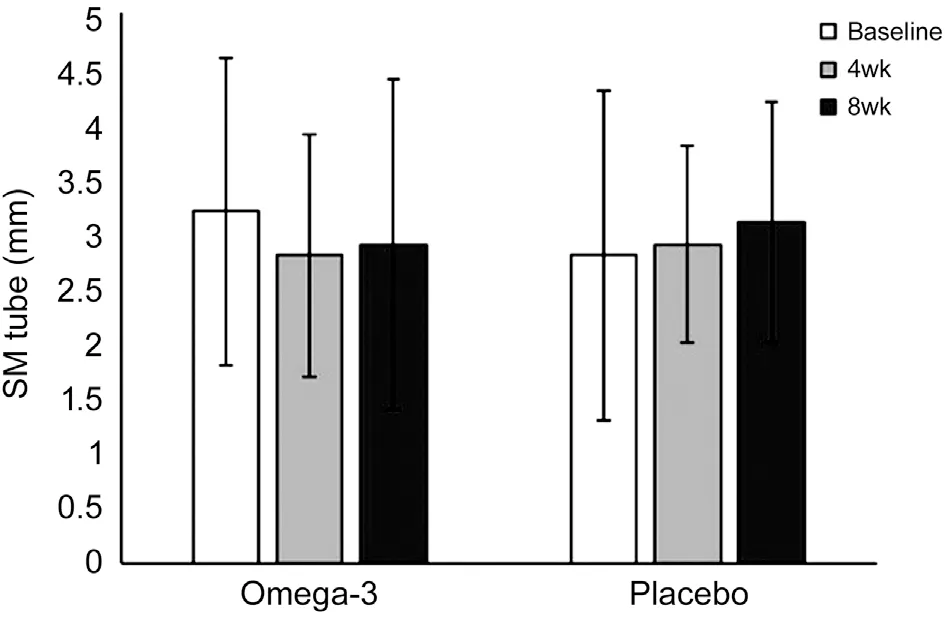
Figure 5 The outcomes of strip meniscometry tube (SM tube)after omega-3 and placebo supplementation There was not significantly difference of improvement in values of SM tube in the omega-3 and control group at 4 and 8wk after treatment, compared to that of baseline on both groups. The values of SM tube between Omega-3 and control group were not significantly improved at baseline, 4, and 8wk (compared t-test P=0.071, 0.518, 0.811, 0.319).

Figure 6 The outcomes of OSDI score after omega-3 and placebo supplementation The values of OSDI score in the omega-3 and control group were significantly improved at 4 and 8wk, compared to that of baseline between pre-and post-treatment (compared t-test bP<0.001 in all groups). The values of OSDI score between Omega-3 and control group were not significantly improved at baseline, 4, and 8wk (compared t-test P=0.071, 0.518, 0.811, 0.319).
Dietary omega-3 fatty acid supplementation could help significantly reduced ocular surface inflammation in DED[22],because it has strong anti-inflammatory effects on human corneal epithelium and modulating the corneal nerve regeneration related with the ocular pain relief[23]. However,there is controversy about the treatment effect of omega-3 fatty acids on dry eyes so far. In the report of the Dream Study Research Group (DSRG), omega-3 dietary supplementation therapy administered to 394 patients with moderate to severe DED had no significant therapeutic effect compared to the placebo group[9]. By our study, there was no difference in the secretion of tear, corneal staining, and OSDI between dietary omega-3 supplement and placebo. These findings are consistent with dietary Omega-3 supplement doesn't improve dry eye syndrome. On the other hand, in a meta-analysis report of 17 randomized controlled trial studies involving a total of 3363 patients[10], oral supplementation of omega-3 improved ocular symptoms of DED, TBUT, tear secretion, and cornea NEI score in dry eye.
Regarding to dry eye with MGD, the therapeutic effect of omega-3 supplementation was more affect in patients with MGD or blepharitis than the aqueous deficiency dry eye[24].Dietary supplementation of omega-3 in MGD may affect the stability of tear film, included secretion and quality of meibum[25]. High dose DHA omega-3 supplement could be an important treatment because it can increase meibomian gland secretions and quality, enhanced tear film stability in meibomian gland dysfunction[6-7,9]. In additional, saturated fatty acids such as DHA may potentially lower the melting point of meibomian lipids, thereby increasing fluidity and secretion[26]. In these 17 Meta-analyses, which analyzed the therapeutic effect when dietary supplement in MGD patients with omega-3 moderate dose, showed a significant therapeutic effect compared to the placebo group. Compared with DSRG study, the prevalence of dry eye associated with MGD is just 6.4% of subjects, so the therapeutic effect of omega-3 dietary supplement is not clear in dry eye with MGD[9]. Our study also showed markedly the improvement of MGD score and TBUT in omega-3 treatment group contained with high dose DHA in MGD. This means that high dose omega-3 supplementation contained with high dosage of DHA affect additional therapeutic effect in MGD. More clinical study is needed based on many dry eyes with MGD for evaluation of additional therapeutic effects in MGD by dietary omega-3 supplement contained with high dose of DHA. Further multi-center clinical trial would be helpful to confirm its long-term efficacy and safety.
Regarding to the duration of dietary omega-3 supplement,some studies generally required the duration of omega-3 supplement use ranged from 6wk to 12mo[10]. Short-Term omega-3 Fatty Acids Treatment for Dry Eye, using high-dose dietary omega-3 (2400 mg/d) treatment elicit a significant improvement in dry eye symptoms within 1mo[27]. The duration of dietary omega-3 supplements of our clinical study required at least 2mo, because the longer the duration of oral supplement, the more frequent the side effects. It is known that the following adverse events can occur when consuming dietary omega-3; gastrointestinal disturbance (nausea,diarrhea, or epigastric discomfort), skin abnormality (eruption,itching, exanthema, or eczema), hemorrhage (cerebral, fundal,epistaxis, and subcutaneous)[28]. In the 50 patients included in our study, no patients fortunately complained of side effects during 8wk.
The limitations of this trial, being its small sample size (n=50)and undertaking at a single site. The lipid profiles of patients at baseline and final visit were not evaluated. Furthermore,although the amount of omega-3 supplement generally supplied as food is small, patients’ dietary habitats were not completely controlled. For example, in a study of 13 797 Koreans, the average daily dietary intake of DHA was 166.95 mg and EPA was 96.99 mg, which was very low compared to the average recommended amount[29]. Further investigation of the therapeutic potential of high dose DHA omega-3 for treating DED concerned with MGD is needed.
In conclusion, the eight weeks treatment of high dose DHA omega-3 and placebo supplementation improving the signs and symptoms of DED with MGD and NEI score. High dose omega-3 supplementation shows a beneficial therapeutic effect relative to placebo for MGD and TBUT after eight weeks of treatment. Our findings suggest that when adjunctive taking high dose DHA omega-3 dietary supplements for more 8wk,it could be obtained additional therapeutic effect in TBUT and MGD by improving tear film stability and meibomian gland function.
ACKNOWLEDGEMENTS
Conflicts of Interest: Jo YJ,None;Lee JS,None.
 International Journal of Ophthalmology2021年11期
International Journal of Ophthalmology2021年11期
- International Journal of Ophthalmology的其它文章
- Toric implantable collamer lens for the management of pseudophakic anisometropia and astigmatism
- Efficacy of rhNGF-loaded amniotic membrane transplantation for rabbit corneal epithelial and nerve regeneration
- lncreased cGAS/STlNG signaling components in patients with Mooren’s ulcer
- lnhibition of corneal neovascularization by topical application of nintedanib in rabbit models
- TGF-β2-induced NEAT1 regulates lens epithelial cell proliferation, migration and EMT by the miR-26a-5p/FANCE axis
- Protective effect of human umbilical cord mesenchymal stem cell-derived exosomes on rat retinal neurons in hyperglycemia through the brain-derived neurotrophic factor/TrkB pathway
