A modified, simple technique for internal limiting membrane free flap transplantation in macular hole surgery: the Peel-PFCL-Peel technique
Hyun Goo Kang, Jae Yong Han, Jae Won Jun, Min Kim
Dear Editor,
We would like to introduce a simple but modified variant perfluorocarbon liquid (PFCL)-assisted technique, namely the “Peel-PFCL-Peel” technique, which overcomes these difficulties while improving manipulation and retention of the ILM free flaps during macular hole (MH)surgery.
Idiopathic full-thickness MH most commonly appears in patients in their 50s or 60s, more frequently in women, and causes either gradual or abrupt impairment of central vision with metamorphopsia[1]. Vitrectomy for MH closure was first described in 1991 by Kelly and Wendel[2], and is widely used with high success rates and significant functional improvement.However, even in the age of small gauge vitrectomy with internal limiting membrane (ILM) peeling techniques[3], MH can still recur or remain open after the initial surgery; a recent review found an MH recurrence rate of 3.3%, with 31% of these eyes requiring more than one additional operation for successful hole closure[4].
Various techniques have been introduced in recent years to improve surgical outcomes and prevent secondary MH recurrence in eyes with large (>400 µm), recurrent, or persistent MH[5-6]. These generally rely on using various materials such as autologous ILM flaps, amniotic membranes,lens capsule, and scleral or retinal flaps to fill the MH and act as scaffolds for promoting glial proliferation and tissue repair[7].
Among these techniques, variations of the inverted ILM flap or autologous ILM free flaps appear to be especially promising in terms of successful MH closure with significant visual acuity improvement[8]. A major advantage of autologous ILM free flaps is the relative ease with which it can be obtained, even in secondary operations with absent perifoveal ILM; however,the technique is surgically and technically challenging owing to the difficulty in stabilizing and manipulating the thin free flaps[9]. PFCL-assisted methods have been described previously, but the current technique may still be demanding for some surgeons. PFCL injected prior to ILM peeling results in difficulty in creating the flap itself, while PFCL injected after flap creation necessitates insertion of additional trocar/cannula and the use of the non-dominant hand for PFCL injection while holding the peeled flap. Thus, injecting PFCL after completion of the ILM flap tends to result in spontaneous flap loss, or the flap may refuse to enter the bubble and float on the surface[8].We can show this technique used successfully in a woman in her mid-60s presenting with worsening central visual blurring in her right eye. She had a surgical history of attempted MH repair combined with cataract surgery 2y previously at another center, with the immediate postoperative optical coherence tomography (OCT) images showing persistent MH. Her bestcorrected visual acuity (BCVA) was 20/100. Dilated fundus examination revealed a large, recurrent MH (Figure 1A),with elevated margins and cystoid spaces on OCT (Figure 1A, inlet). The MH diameter was approximately 1200 µm at the base and 780 µm at the narrowest distance between the hole edges. We performed vitrectomy with ILM free flap transposition using our modified “Peel-PFCL-Peel” technique.The use of patient’s imaging and surgery video data was approved by our Institutional Review Board, and the need for informed consent was waived (IRB No. 3-2020-0124).
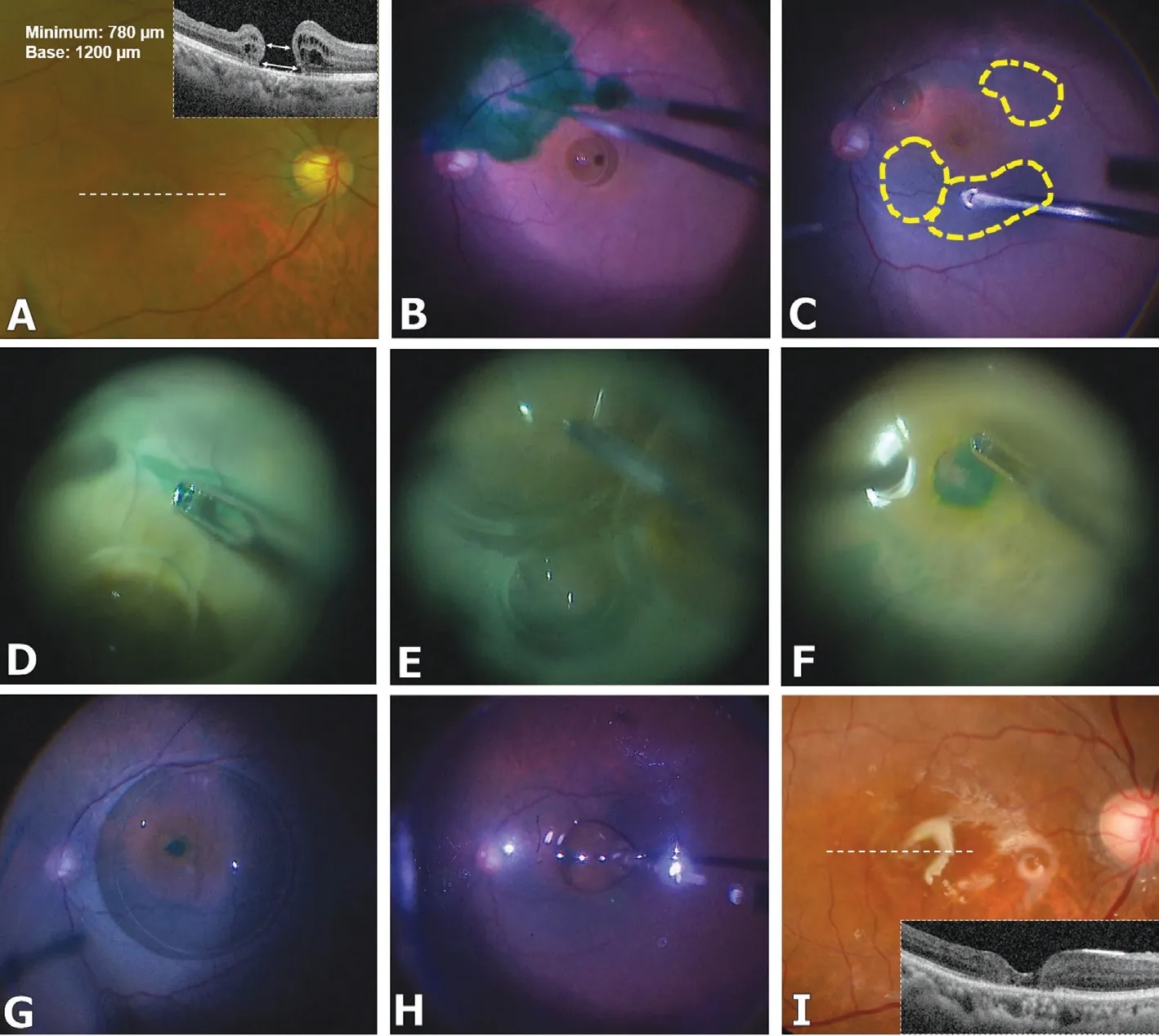
Figure 1 A simple modified PFCL-assisted technique for ILM free flap transplantation during MH surgery: the Peel-PFCL-Peel technique A large, persistent MH is noted on fundus photography (A) with elevated margins and cystoid spaces on OCT (MH size: 1200 µm base, 780 µm minimum) (A, inlet). A small PFCL bubble is injected to protect the exposed retinal pigment epithelium at the fovea (B), and the ILM is stained using indocyanine dye. Autologous ILM free flaps are planned with the remnant ILM (C). After partially peeling the pre-planned flaps to create edges that could be easily grasped (D), the posterior pole is filled judiciously with PFCL (E). The ILM is fully peeled and the flaps are transplanted within the MH (F). The PFCL bubble prevents the free flaps from floating away and flittering out of sight (G). After fluid-air exchange and rinsing to remove all PFCL, silicone oil is injected away from the fovea under direct visualization (H). At 1wk postoperatively, the fovea can be seen filled with the ILM material (I) and the foveal architecture appears well recovered on OCT (I, inlet).
A standard 3-port, 25-gauge vitrectomy (Constellation®Vision System; Alcon Laboratories, Fort Worth, TX, USA) was performed. After confirming that the vitreous had been fully removed, a small PFCL bubble was injected over the fovea to protect the exposed retinal pigment epithelium (RPE), and indocyanine green dye was used to stain the remaining ILM in the macular area (Figure 1B). On identifying the area of the remaining ILM, we could determine whether a fovea-adjacent hinged ILM flap could be created and transposed, or a fully free ILM flap would be needed to be transplanted within or outside the macular area (Figure 1C).
Once the surgical plan was established, the planned ILM flaps were partially peeled to create edges that could be easily regrasped even if they were to be flattened under PFCL (Figure 1D). Then, additional PFCL was injected so that the entire posterior pole and the entirety of all planned ILM flaps were covered (Figure 1E). Finally, the previously peeled ILM flap edges could be easily visualized and grasped under the PFCL,completing the free flaps and placing them within the MH(Figure 1F). As these maneuvers were performed within the PFCL bubble, the high density and high interfacial tension of PFCL enabled to stabilize the free ILM flap once released, and to re-grasp the flaps for proper placement within the MH if necessary, without fear of them floating away and flittering out of the view (Figure 1G).
After gentle massaging of the MH margins, fluid-air was first exchanged, followed by careful and deliberate PFCLair exchange. The posterior hole was carefully rinsed with balanced salt solution (BSS) to ensure that the PFCL was fully removed; then, silicone oil was injected gently under direct visualization (Figure 1H). In all instances when BSS or silicone oil was injected, we ensured that the point of contact or impact was away from the macular area, so as to prevent dislodging of the ILM flaps. Finally, we removed all instruments from the eye. The total surgical time was less than 45min.
At postoperative week 1, the patient’s uncorrected visual acuity was 20/100 and she experienced subjective improvement in her presenting symptoms (central visual blurring) with no signs of complications. Evaluation with dilated funduscopy revealed well-placed translucent, greyish ILM material within the MH(Figure 1I), and OCT showed a closed MH with a seemingly recovered foveal contour (Figure 1I, inlet). By the end of her 6mo post-operative follow-up, she experiences significant improvement in her symptoms with a BCVA of 20/25.
This Peel-PFCL-Peel technique is a simple, variant sequence that efficiently stabilizes and immobilizes the ILM free flap, thus improving surgical control and enabling ILM transplantation within the MH. Our modified technique can be utilized in both autologous flap transplantation (free flap) and the inverted ILM flap technique (hinged flap).
The ILM free flap transplantation technique for MH requires expertise, and may be very difficult to perform especially in high myopes and in case of unstable fluidics in vitrectomized eyes. PFCL has a high density and interfacial tension and was originally used intraoperatively during surgery for proliferative vitreoretinopathy and highly bullous rhegmatogenous retinal detachment, as the so-called “heavy liquid” can hold down and stabilize the retina during various surgical maneuvers.Although the use of PFCL in ILM peeling was reported in as early as 2002[10], our variant sequence allows for a simple systematic method for ILM flap transplantation: creating the ILM edge (first “peel”), then filling with PFCL, and finally peeling the rest of the planned ILM flap for MH closure.Furthermore, under the PFCL, a single-layer ILM flap can be easily created, thus forming a niche environment where mesenchymal factors in the microenvironment between the ILM and RPE may facilitate glial proliferation and migration[8].In conclusion, our simple, modified technique efficiently improves the creation and transplantation of ILM free flaps in persistent or recurrent MH under challenging surgical conditions.
ACKNOWLEDGEMENTS
Authors’ contributions:Conception or design of the work:Kang HG, Han JY, Jun JW and Kim M; Data collection: Kang HG, Han JY and Kim M; Data analysis and interpretation:Kang HG, Han JY and Kim M; Drafting the article: Kang HG and Kim M; Critical revision of the article: Kang HG, Han JY and Kim M.
Foundations:Supported by a National Research Foundation of Korea (NRF) grant funded by the Korean government(MSIT) (No.NRF-2019R1G1A1008122), and by the Korean Association of Retinal Degeneration.
Conflicts of Interest:Kang HG, None; Han JY, None; Jun JW, None; Kim M, None.
 International Journal of Ophthalmology2021年10期
International Journal of Ophthalmology2021年10期
- International Journal of Ophthalmology的其它文章
- lmpact of intraocular pressure fluctuations on progression of normal tension glaucoma
- Effective treatment for secondary angle-closure glaucoma caused by traumatic lens subluxation:phacoemulsification with capsular-tension-ring implantation combined with ophthalmic endoscopecontrolled goniosynechialysis
- Efficacy and safety of newly developed preservativefree latanoprost 0.005% eye drops versus preserved latanoprost 0.005% in open angle glaucoma and ocular hypertension: 12-week results of a randomized,multicenter, controlled phase III trial
- Progressive restrictive strabismus in an infant
- Association of peripheral anterior synechia, intraocular pressure, and glaucomatous optic neuropathy in primary angle-closure diseases
- Protective effect of LIF-huMSCs on the retina of diabetic model rats
