Progressive restrictive strabismus in an infant
Hong-Gai Yan, Ning-Dong Li
Department of Ophthalmology, Beijing Children’s Hospital,Capital Medical University, National Center for Children’s Health, Beijing 100045, China
Dear Editor,
In this work, we evaluated a special case. Acquired progressive restrictive strabismus is very rare in the infants. We have been accessed to literatures and found only 5 infants had been reported. So, we report a case of progressive restrictive strabismus in a 4-month-old infant and using an anterior orbitotomy approach for the strabismus surgery.
Restrictive strabismus is characterized as limitation of ocular motility at any one or multiple fixating directions caused by intrinsic or extrinsic mechanical forces, such as fibrosis of the ocular muscles. It can be divided into congenital and acquired restrictive strabismus according to the age of onset as well as the underlying pathogenesis. Congenital restrictive strabismus is not rare in the infants and is documented as congenital fibrosis of the extraocular muscles (CFEOM), Duane’s restriction syndrome (DRS), Mobius syndrome, Brown syndrome, as well as congenital orbital fibrosis[1]. Patients with congenital restrictive strabismus have a history of limitation of ocular movements since birth. However, acquired progressive restrictive strabismus is very rare in the infants but more common in the adults, usually caused by trauma[2], tumors[3],infiltrated inflammation of the ocular muscles such as thyroid disease[2]. Here, we report a case of progressive restrictive strabismus in a 4-month-old infant.
A 4-month-old female infant was brought by her parents to our department because that her “black eye” was gradually gone to her left orbit. She was a full-term infant and delivered normally without family or medical history. She had a normal eye position and ocular motility since birth (Figure 1A). However,her left eye started to deviate downward and medially without any reasons at the age of 2mo. Subsequently, downward deviation was aggravating progressively. Finally, her left eye turned in the extremely infradducted and esotropic position at the age of 4mo. Ocular examination showed that her cornea was invisible and buried completely behind her inferior eyelid(Figure 1B). A congestive conjunctiva was showed in her left eye. Forced duction test showed her left eye was hardly elevated and “fixed” at the downgaze position with relative restriction on abduction.
Computed tomography (CT) scan showed that her left inferior rectus muscle was thickened and fuzzy, which was interpreted by the radiologist as typical of myositis (Figure 1D, 1F).However, inflammatory factors were not increased, so did the levels of thyrotropin, thyroxine, and the thyroid-stimulating immunoglobulin, according to the laboratory tests.
Surgical treatment was performed for her invisible “black eye” under general anesthesia at the age of 4mo. Forced duction test was performed preoperatively, intraoperatively and postoperatively. An anterior orbitotomy approach was employed to explore her left inferior rectus muscle because it was too tight to be hooked from conjunctiva incision. When the orbital septum was exposed, we found that orbital adipose tissue was partially replaced by the scar tissue, which further supported that inflammation had occurred in her left orbit. An extremely tight inferior muscle was finally hooked along the inferior wall of the eyeball without under direct visualization.When we were trying to dissect the scar tissue around the inferior rectus, her inferior rectus muscle was fractured suddenly from 7 mm behind its attachment, so that her left eye was elevated, and cornea was completely visible. Upward limitation was completely released, which was confirmed by the forced duction test intraoperatively. The stump of inferior rectus muscle was taken off and sent to biopsy with its around tissues. Biopsy showed that her inferior rectus muscle was fibrotic and infiltrated with the inflammatory cells (Figure 1F).Her primary eye position had been improved significantly with a 10° residual hypodeviation in 1wk after surgery (Figure 1C).As we mentioned above, acquired and progressive restrictive strabismus in infancy is very rare. Up to date, only a few cases have been reported (Table 1)[4-6]. The minimum age of onset is 2mo according to the reports. Monocular disorder is more common. Inferior rectus is frequently involved, followed by medial and superior rectus muscles, lateral and oblique muscles were rare. Subacute myositis has been suggested tobe the cause of this disorder. However, its definite etiology is still unknown. Early steroid treatment could be helpful for releasing the symptoms and averting a large angle strabismus.However, most patients finally undergo surgery in prevention of amblyopia in the affected eye.

Table 1 The cases have been reported
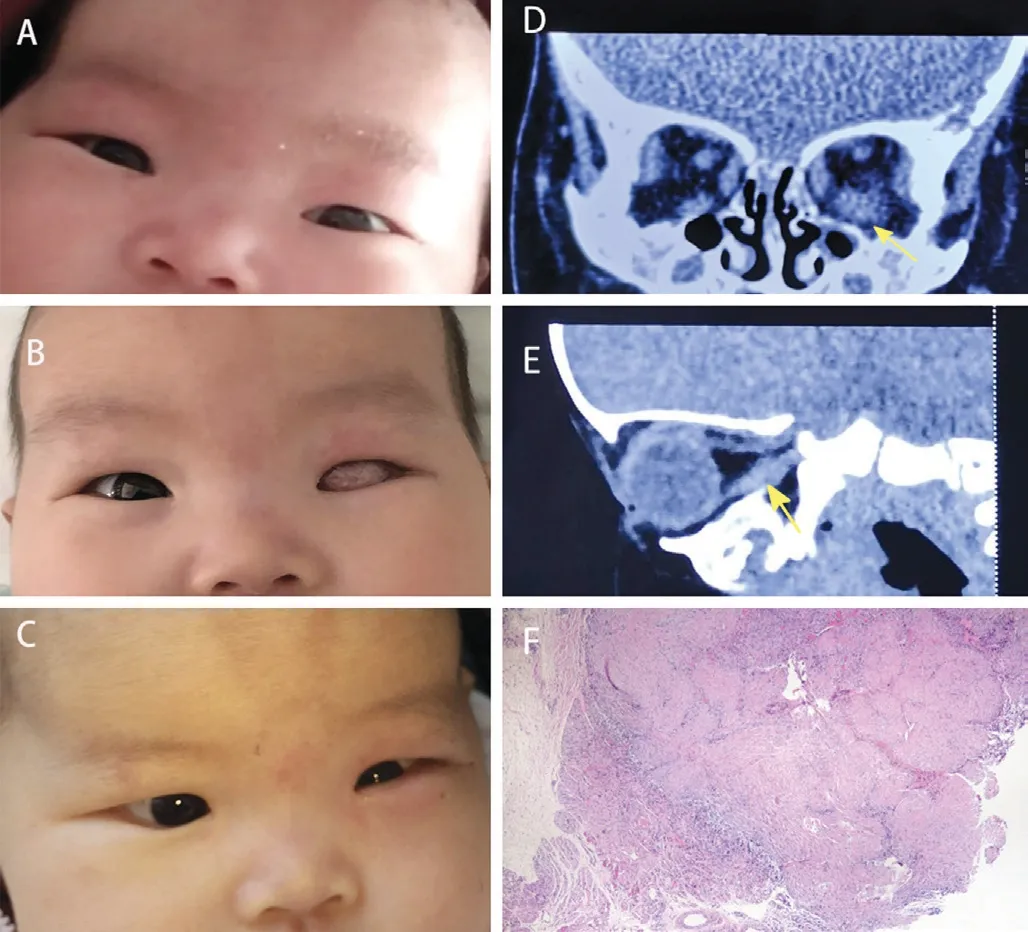
Figure 1 Left eye position in three different stages, enlarged inferior rectus in the images of the CT scan and biopsy of the inferior rectus muscle A: A normal eye position was showed in a female infant at the first month since birth; B: An extremely infraducted and eso-shift position with an invisible cornea at 4mo and the conjunctiva was congestive in her left eye; C: A slight eso- and hypo- shift of her left eye was showed in 1wk after operation; D and E: An enlarged inferior rectus muscle(the yellow arrow) was seen in the sagittal and the coronal positions of the CT scan; F: Histopathologic evaluation of the inferior rectus muscle showed that sheet fibrous tissue could be seen in skeletal muscle tissue, and degenerated skeletal muscle fibers were still visible(Hematoxylin & Eosin, ×40).
In this case, progressive restrictive strabismus occurred in a 2-month-old female infant. All factors, such as congestive conjunctiva, enlarged inferior rectus in CT scan, surgical findings, as well as biopsy, supported that her strabismus was secondary from orbital inflammation which resulted in a large angle hypodeviation of her left eye. Forced duction test showed that her left eye was completely fixated at the downward position and hardly to be elevated. We suppose that her inferior rectus could be adhered tightly to its around tissues and steroid treatment could be ineffective at that time, so we performed surgery for her. The fact that her inferior rectus was broken during the operation demonstrates that her inferior rectus had been fragile and taut due to inflammatory involvement.
Previous studies showed that surgical management for an acquired restrictive strabismus was challenging because the patients had an extremely abnormal eye position, and the postoperative outcome was very poor with exotropia and limited infraduction. In our experience, preoperative evaluations for the patients are very important, including systemic and ophthalmic examinations, radiological images as well as forced duction test. An anterior orbitotomy approach could be more convenient for this kind of complicated strabismus surgery. Although the infant still has a residual hypodeviation, she has already acquired an improved cosmetic change. In addition, her cornea has been visible, which would be benefit for amblyopia treatment in the future.
In conclusion, acquired and progressively restrictive strabismus is very rare in infancy. We propose earlier surgery once we have made a correct diagnosis and excluded those factors caused by acute infection, bleeding, or tumor infiltration, in order to avoid amblyopia and improve the infant’s cosmetic appearance.
ACKNOWLEDGEMENTS
Conflicts of Interest:Yan HG, None; Li ND, None.
 International Journal of Ophthalmology2021年10期
International Journal of Ophthalmology2021年10期
- International Journal of Ophthalmology的其它文章
- lmpact of intraocular pressure fluctuations on progression of normal tension glaucoma
- Effective treatment for secondary angle-closure glaucoma caused by traumatic lens subluxation:phacoemulsification with capsular-tension-ring implantation combined with ophthalmic endoscopecontrolled goniosynechialysis
- Efficacy and safety of newly developed preservativefree latanoprost 0.005% eye drops versus preserved latanoprost 0.005% in open angle glaucoma and ocular hypertension: 12-week results of a randomized,multicenter, controlled phase III trial
- Association of peripheral anterior synechia, intraocular pressure, and glaucomatous optic neuropathy in primary angle-closure diseases
- Protective effect of LIF-huMSCs on the retina of diabetic model rats
- Therapeutic effect of a traditional Chinese medicine formulation on experimental choroidal neovascularization in mouse
