Treatment of Nevoid Basal Cell Carcinoma Syndrome by Surgery Combined With ALA-PDT:A Case Report
Chun Pan,Qian Zhang,Wen-Bo Bu,Hao Chen,Yan Wang,∗,Fang Fang,∗
1Department of Dermatologic Surgery,2Department of Dermatologic Histopathology,Hospital for Skin Diseases(Institute of Dermatology),Chinese Academy of Medical Sciences and Peking Union Medical College,Nanjing,Jiangsu210042,China.
Abstract
Keywords:nevoid basal cell carcinoma syndrome,basal cell carcinoma,eyelid tumor,photodynamic therapy
Introduction
Nevoid basal cell carcinoma syndrome(NBCCS),also known as Gorlin–Goltz syndrome,is a rare multisystem disease caused by a mutation in the patched gene.1It is inherited in a dominant autosomal manner with complete penetrance and variable expressivity.This syndrome is characterized by multisystem abnormalities,especially the early appearance of multiple basal cell carcinomas.2We herein present a case of NBCCS that manifested as multiple BCCs and palmar pits and was treated by surgery combined with5-aminolevulinic acid-mediated photodynamic therapy(ALA-PDT).
Case report
A60-year-old man presented with a>30-year history of systemic plaques and nodules.He had been employed in an alkylbenzene factory for more than20years(since the age of20years).Disease onset occurred after10years of working in the factory.Infiltrative red plaques and black papules of unknown cause were scattered over the trunk and limbs,and they gradually increased in severity.Neoplasms appeared on the surface of the papules,which gradually affected the face and developed bright surfaces that appeared likely to rupture(Fig.1A).No skeletal deformity or obvious abnormality was found in oral and cranial radiographic examinations.None of the patient’s family members had similar diseases.
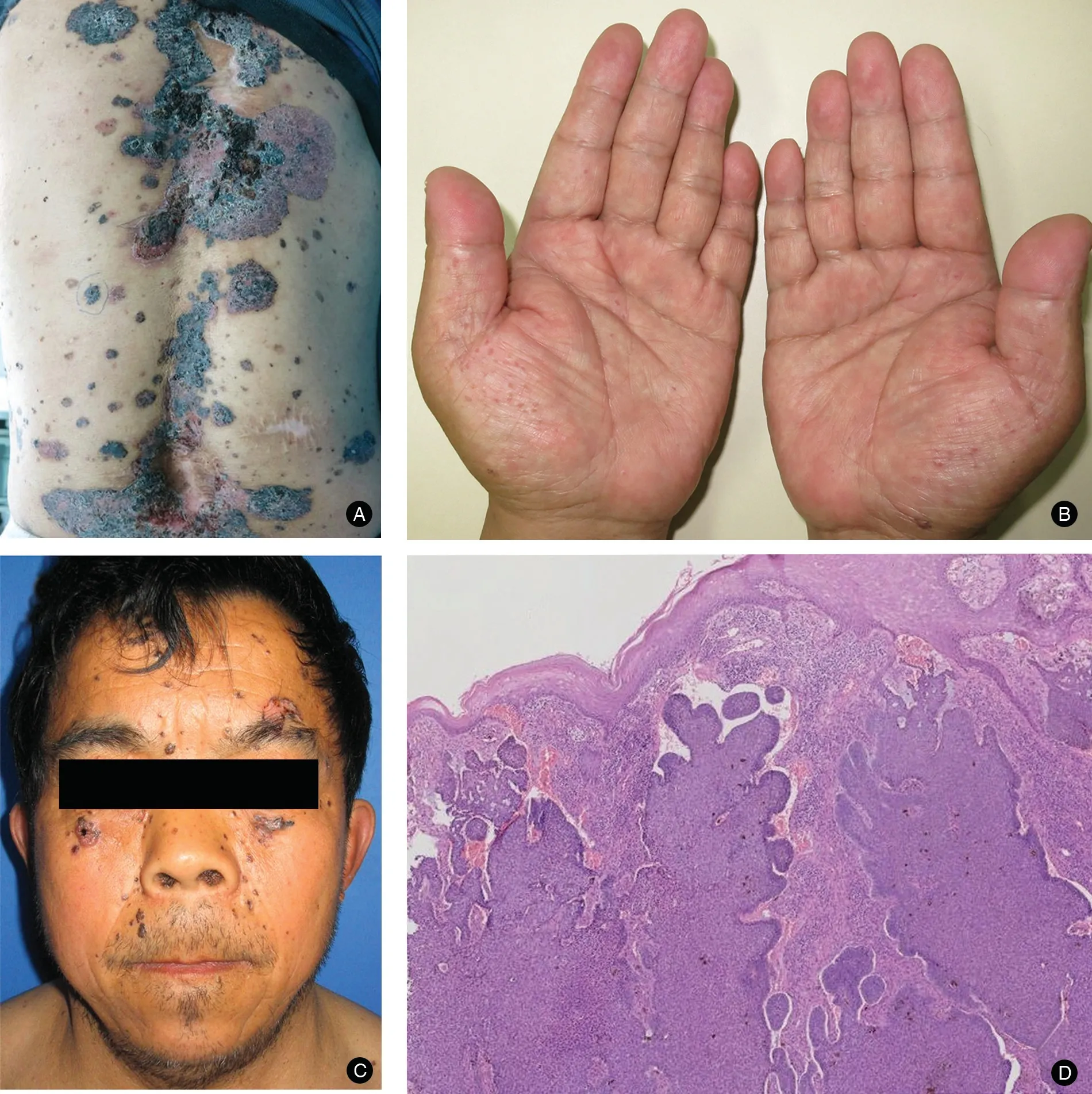
Figure1.The cutaneous and histopathological examination findings of the patient with NBCCS.(A)Invasive erythema was scattered on the back with a region of black pearl-like bulges.Neoplasms were seen in the central area of erythema and appeared likely to rupture.(B)Examination of the hands revealed palmar pits.(C)Lesions clinically compatible with NBCCS were seen on the face.(D)Histopathological examination showed well-defined collections of basophilic basaloid cells exhibiting typical peripheral“palisades”and adjacent stromal retraction with gap formations.(Hematoxylin and eosin stain;×25).NBCCS:nevoid basal cell carcinoma syndrome.
A cutaneous examination revealed invasive erythema with slight tenderness scattered on the back and welldefined black pearl-like bulges.Neoplasms were seen in the central area of erythema,and the lesions appeared likely to rupture and bleed(Fig.1B).Most areas of both palms showed flesh-colored,needle-sized pits(Fig.1C).The pigmented papules on the back were histopathologically examined,revealing tumor nests consisting of basaloid cells in the papillary and reticular dermis accompanied by slit-like retraction.The surrounding stroma showed myxoid change.Melanin pigmentation of the tumor cells was also seen(Fig.1D).Histopathological examination of the palmar pits showed focal diminution of the keratin and granular layers.The findings were consistent with NBCCS.
The patient was admitted to local hospital in December 1987and underwent surgical excision of the chest lesions.However,2months after surgery,the black papules recurred and expanded to plaques.No special treatment was administered;as a result,the multiple lesions caused severe pain,spread throughout the whole body,and gradually expanded.From2006to2014,the patient was admitted to the hospital four times because of ulceration and exudation of the lesions,and he finally underwent extended excision of the BCCs on the chest(Supplementary Fig.1,http://links.lww.com/JD9/A7),with arm,back,abdomen,bilateral axillae,and left frontal region combined with full-thickness skin grafting.Skin biopsies were obtained from the concave part of the fingers.Although the lesions were cured in the surgically treated areas,new lesions occurred on the surrounding skin.

Figure2.The patient underwent left frontal tumor excision and full-thickness skin grafting in2014.No new lesions were found in the treated areas during3years of follow-up.(A)Before ALA-PDT,the tumors on the bilateral lower eyelid enlarged,and the right lower eyelid appeared to be at risk of perforation.The black papule on the edge of the right lower eyelid was curetted.(B)The ulcer on the right lower eyelid gradually healed after six treatments with ALA-PDT,and the black papule on the edge of the right lower eyelid did not recur.(C)The ulcerated surface of the right temporal lesion suddenly profusely bled two times before ALA-PDF.(D)After five additional treatments with ALA-PDT,the recurring hemorrhage of the right temporal lesion resolved and the ulcer healed completely.ALA-PDT:5-aminolevulinic acid-mediated photodynamic therapy.
In2016,tumors on the bilateral lower eyelid enlarged(diameter of2.3cm),and the right lower eyelid was almost perforated(Fig.2A).Because surgical excision was impossible in this area,ALA-PDT was selected as an adjuvant treatment after thorough communication with the patient.The black papule on the edge of the right lower eyelid was curetted before the first application of PDT.ALA(20%;Shanghai Fudan-Zhangjiang Bio-Pharmaceutical Co.,Ltd.,Shanghai,China)was applied in the region of the right eyelid lesions and surrounding2-cm area while shielding these regions from light for4hours,and a635-nm light-emitting diode(Wuhan Yage Photoelectric Medical Devices Co.,Ltd.,Wuhan,China)was used to irradiate the lesions at80mw/cm2for20minutes once a week.After six treatments with ALA-PDT,the right eyelid lesions were controlled,and the black papule on the edge of the right lower eyelid did not recur during follow-up(Fig.2B).However,the ulcerated surface of the right temporal lesions(diameter of2cm)then bled profusely two times(about200mL each time).The bleeding was temporarily stopped by suture ligation and bipolar coagulation(Fig.2C).After five additional treatments with ALA-PDT,the recurring hemorrhage of the right temporal lesions ceased and the ulcer healed completely(Fig.2D).The patient developed no recurrence for almost 1year of follow-up,and gave his agreement for the case publication.
Discussion
Managing multiple tumors in patients with NBCCS is extremely difficult,especially when the lesions occur on the face.No consensus has been reached regarding the optimal strategy.Surgical excision is the standard treatment method but may result in significant disfigurement and difficulty in wound recovery.2Drug therapy is feasible for refractory BCCs;5-fluorouracil,imiquimod,and vismodegib have been approved by the USA Food and Drug Administration for use in superficial BCC,and many other drugs have been used under experimental settings.Vismodegib,a small molecular drug,is believed to be effective for invasive and metastatic BCCs,but its adverse effects should be further studied.3Topical PDT is now recognized in some countries as an adjuvant therapy after surgery for superficial BCCs.4In the present study,the patient underwent three surgeries.No new lesions were found in the treated areas throughout3years of follow-up.This outcome indicates that the tumor was partially benign and could be cured by extended excision.However,the new lesions that continuously occurred over the whole body illustrated the invasive biological characteristics of NBCCS.The disadvantages of surgical excision include tissue trauma and an obvious postoperative scar.In addition,surgery cannot be performed in certain sites,such as the right eyelid area in the present(Fig.2).Because of the difficulty of surgical excision,PDT was chosen to treat the right lower eyelid tumors and bleeding of the right temporal lesion.After application of ALA-PDT,the tumor growth and neovascularization were inhibited;as a result,wound healing was accelerated.As an adjuvant therapeutic approach to skin tumor resection,PDT can reduce the excision range of the tumor with good cosmetic results and can play a significant role in combination therapy for tumors that are extremely difficult to remove completely by surgical excision.5-6However,PDT also has limitations particularly on penetration depth,so it could not comparable with surgery.
In conclusion,particular attention should be paid to early identification and treatment of NBCCS.Surgical excision is the first-choice treatment.However,when complete removal of lesions becomes difficult,ALA-PDT could be considered.The combination of these two therapies can play a complementary role in the treatment of NBCCS.
Source of funding
This work was supported by the National Natural Science Fund of China(No.81872216)and PUMC Postgraduate Education and Teaching Reform Project in2018(No.10023201801701).
- 国际皮肤性病学杂志的其它文章
- Capsaicin Regulates Mitochondrial Fission to Promote Melanoma Cell Apoptosis
- Oxyresveratrol-induced Activation of Nrf2/HO-1 Signaling Pathway Enhances Ability ofResveratrol to Inhibit UVB-induced Melanin
- Linking Cellular Metabolism to Epigenetics in Melanoma
- mTOR-Dependent Autophagy Machinery Is Inhibited in Fibroblasts of Keloid
- Ablative Carbon Dioxide Laser Treatment for Papular Scars of Nose and Chin Due to Acne:A Case Series
- Scrofuloderma:A Rare Case Report of Sequelae of Intestinal Tuberculosis