Scrofuloderma:A Rare Case Report of Sequelae of Intestinal Tuberculosis
Subhayan Das Guptaand Rohon Das Roy∗
1Department of Microbiology,Malda Medical College and Hospital,Malda732101,West Bengal,India;2Department of Microbiology,Midnapore Medical College and Hospital,Paschim Mednipore721101,West Bengal,India.
Abstract
Keywords:Mycobacterium tuberculosis,scrofuloderma,cutaneous tuberculosis,case report
Introduction
Cutaneous tuberculosis(TB)is caused by Mycobacterium tuberculosis(M.tuberculosis)in a majority of cases and rarely by Mycobacterium bovis.It accounts for0.1%–0.9% of the skin conditions among all dermatology outpatients in India.Cutaneous TB is a significant medical problem despite the availability of highly effective chemotherapy.It accounts for approximately1.5% of all tuberculous manifestations.1
Scrofuloderma,also known as tuberculosis colliquativa cutis,is the most common form of cutaneous TB.It arises by direct extension of acid fast bacilli from an underlying tuberculous focus into the skin.Cervical lymph nodes are the most common foci;however,inguinal,axillary,submandibular,supraclavicular,and epitrochlear lymph nodes may also be involved.2-3Primary infection of the bone,intestinal Koch,and hepatic TB are sources of scrofuloderma in children.
Case report
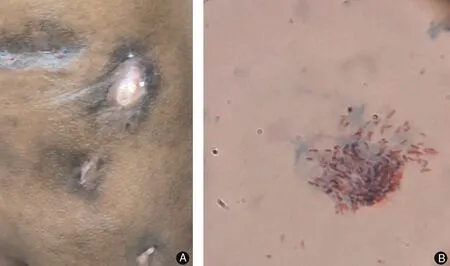
Figure1.Clinical features and laboratory test results of the patient with scrofuloderma.(A)Four ulcerative lesions were observed on the left side of abdomen,the largest measuring3cm×5cm.The ulcers were suppurative and well-demarcated,and they had elevated borders with undermined non-tender edges.The surrounding skin was edematous and pigmented.(B)Ziehl-Neelsen staining of impression smears from the ulcerative lesions showed the presence of acid-fast bacilli.
A28years old man presented with a5-month history of multiple non-healing and painless ulcerative lesions with purulent discharge on the left side of his abdomen.He had a low-grade fever and decreased appetite,and he had lost a significant amount of weight during the past year.He had been diagnosed with intestinal TB9months previously by fine-needle aspiration biopsy,which revealed multiple coalescent granulomas in the mucosa and submucosa.The patient was started on anti-tubercular drugs,but he discontinued treatment.He had no family history of TB.Physical examination revealed four ulcers of varying sizes on the left side of the abdomen,the largest measuring 3cm×5cm(Fig.1).The ulcers were suppurative and welldemarcated,and they had elevated borders with undermined non-tender edges.The surrounding skin was edematous and pigmented.There was no evidence of lymph node involvement.The patient had no history of trauma.His vitals were as follows:pulse rate of74beats/minutes,respiratory rate of22breaths/minutes,and blood pressure of130/80mm Hg.Systemic examination revealed no abnormalities.The results of a complete blood count,urinalysis,and biochemical analysis were normal.The patient’s erythrocyte sedimentation rate was40mm/h in the first hour.The result of an antibody test for human immunodeficiency virus was negative.The Mantoux test was positive(20mm/72h).Ziehl–Neelsen(ZN)staining of impression smears from the ulcerative lesions showed the presence of acid-fast bacilli(Fig.1).Chest X-ray examination revealed no abnormalities.Fungal and aerobic bacterial cultures were negative.Histological examination showed mature squamous cells forming epithelioid granulomas with multinucleated giant cells,caseous necrosis,and mixed inflammatory cells in the dermis.Cultures of the skin biopsy on Lowenstein–Jensen media showed growth of M.tuberculosis after8weeks.PCR for the detection of M.tuberculosis was conducted on a biopsy specimen,and the result was positive.
The patient was diagnosed with scrofuloderma based on his clinical examination findings,the presence of acid-fast bacilli on ZN staining,positive culture,and positive PCR.He began treatment with an anti-tubercular regimen that included isoniazid,rifampicin,ethambutol,and pyrazinamide.The follow-up showed that the cutaneous lesions regressed and the ulcer healed after18months.The authors confirmed that the patient agrees to publish the case.
Discussion
Globally,an estimated10million people fell ill with TB in 2019.4Cutaneous TB remains a rare infection,with an incidence of3.5%reported among patients with organ TB.Scrofuloderma is the commonest form of cutaneous TB,5and starts as a painless subcutaneous nodule that ruptures,giving rise to shallow ulcers with undermined edges and granulation tissue at the base.The disease has a chronic,insidious course,leading to formation of intermittently discharging sinus tracts that heal with characteristic puckered scarring and producing irregular adherent masses that are densely fibrous in places.6
Diagnosis of scrofuloderma is always challenging because the clinical appearance of the lesions is not always characteristic and a positive culture is not always obtained.Biopsy from the periphery of the lesion may show granulomas with caseous necrosis,the center of which is dominated by necrotic and abscess material with inflammatory infiltrates.In the epidermis,scarring and atrophic changes often predominate.M.tuberculosis bacilli are easy to identify in the purulent discharge or biopsy tissue.The tuberculin test is usually positive.7
Scrofuloderma may be a manifestation of systemic TB or result from direct extension or hematogeneous spread of the infection.The incidence of systemic involvement is reportedly35% in adults with scrofuloderma.PCR has increased the sensitivity of the overall detection of cutaneous TB with the possibility of earlier initiation of treatment.8
There are several other differential diagnoses for discharging sinuses,such as atypical mycobacterial infection,sporotrichosis,botryomycosis,actinomycosis,and nocardiosis.2PCR and histopathology can easily distinguish between atypical mycobacterial infection from M.tuberculosis.Actinomycosis presents with multiple discharging sinuses with typical sulfur granules.Nocardia spp.appear as branching filamentous bacilli at right angles.The absence of fungal hyphae on histopathology leads to exclusion of sporotrichosis.Botryomycosis is diagnosed by the presence of bacteria in pus;it is mainly found in immunocompromised patients,and the lesions usually appear on the extremities.
Cutaneous TB is treated according to the recommendations for extrapulmonary TB.Recommended treatment includes a2-month four-drug regimen(isoniazid,rifampicin,pyrazinamide,and ethambutol)followed by a4-month two-drug regimen(isoniazid and rifampicin).Fixed-dose combinations should preferably be used.The World Health Organization recommends that daily dosing throughout the duration of the above-mentioned therapy is optimal for all patients who have been newly diagnosed with TB.9
The response to anti-tubercular treatment alone as a primary therapy is usually good.However,surgery,such as electrosurgery,cryosurgery,and curettage with electrodessication of affected nodes,can also be considered as an adjunctive measure.
We have herein presented a case involving a patient with a chronic,non-healing ulcers,which is a common presentation of scrofuloderma.Diagnosis of scrofuloderma may pose a challenge.However,a proper history and thorough examination with relevant investigations,such as ZN stain of the tissue sample and PCR,can facilitate rapid diagnosis of the infection and early initiation of treatment.
- 国际皮肤性病学杂志的其它文章
- Capsaicin Regulates Mitochondrial Fission to Promote Melanoma Cell Apoptosis
- Oxyresveratrol-induced Activation of Nrf2/HO-1 Signaling Pathway Enhances Ability ofResveratrol to Inhibit UVB-induced Melanin
- Linking Cellular Metabolism to Epigenetics in Melanoma
- mTOR-Dependent Autophagy Machinery Is Inhibited in Fibroblasts of Keloid
- Ablative Carbon Dioxide Laser Treatment for Papular Scars of Nose and Chin Due to Acne:A Case Series
- Treatment of Nevoid Basal Cell Carcinoma Syndrome by Surgery Combined With ALA-PDT:A Case Report