Neoadjuvant chemotherapy without radiation as a potential alternative treatment for locally advanced rectal cancer:A metaanalysis
Pei Wu,Hui-Mian Xu,Zhi Zhu
Pei Wu,Department of Gastrointestinal Surgery,Yongchuan Hospital of Chongqing Medical University,Chongqing 402160,China
Pei Wu,Hui-Mian Xu,Zhi Zhu,Department of Surgical Oncology,The First Hospital of China Medical University,Shenyang 110001,Liaoning Province,China
Abstract BACKGROUND Neoadjuvant chemoradiotherapy(Neo-CRT)is the current standard strategy for treating locally advanced rectal cancer.However,it delays the administration of optimal chemotherapy and increases toxicity.AIM To compare the feasibility and efficacy of neoadjuvant chemotherapy(Neo-CT)and Neo-CRT for patients with locally advanced rectal cancer.METHODS The Cochrane,EMBASE,and PubMed databases were searched for relevant articles using MESH terms and free words.The hazard ratio of overall survival and the risk ratio(RR)for the pathological complete response,the sphincter preservation rate,and treatment-related adverse events were analyzed.RESULTS A total of 19 studies of 60870 patients were included in the meta-analysis.There was no significant difference in overall survival[hazard ratio=1.09,95%confidence interval(CI)=0.93–1.24;P=0.19]or the pathological complete response(RR=0.79,95%CI=0.61–1.03;P=0.086)between the Neo-CT and Neo-CRT groups.As compared to the Neo-CRT group,the incidences of anastomotic fistula(RR=0.49,95%CI=0.35–0.68;P=0.000)and temporary colostomy(RR=0.69,95%CI=0.58–0.83;P=0.000)were significantly lower in the Neo-CT group,with a simultaneous increase in the sphincter preservation rate(RR=1.07,95%CI=1.01–1.13;P=0.029).However,there was no significant difference in the tumor downstaging rate,overall complications,and urinary complications.CONCLUSION Neo-CT administration can lower the incidences of anastomotic fistula and temporary colostomy and increase the sphincter preservation rate as to compared to Neo-CRT and could provide an alternative to chemoradiotherapy for locally advanced rectal cancer.
Key Words:Rectal cancer;Neoadjuvant chemotherapy;Chemoradiation;Prognosis
INTRODUCTION
Preoperative administration of fluorouracil-based chemoradiotherapy(CRT)followed by total mesorectal excision(TME)and postoperative systemic therapy has been the standard strategy for treatment of locally advanced rectal cancer(LARC)since a 2004 randomized controlled study reported a lower local recurrence rate as compared to postoperative chemoradiation[1].
In subsequent clinical trials,neoadjuvant CRT(Neo-CRT)achieved significantly lower recurrence rates,greater accuracy of degrading staging,and higher R0 resection rates.However,with increasing application,the deficiencies of such regimens have started to arouse attention,including the long treatment cycle,including 25 d of concurrent CRT,6–8 wk of recovery followed by TME,and 6 mo of perioperative treatment as well as the relatively high incidence(9%–20%)of anastomotic fistula formation in lower rectal cancer(RC)[2].In addition,a second surgery is required after 3 mo to address the stoma.Long-term toxicity and the incidence of side effects,such as rectovaginal fistula,vaginal wall perforation,intestinal obstruction,perineal incision healing delay,peritoneal fibrosis,urethral irritation,control dysfunction,and sexual dysfunction,increase over time.Further,most clinical trials found that Neo-CRT did not improve overall survival(OS)due to higher distant metastatic rates.Finally,the presence of peritoneal fibrosis may increase the difficulty of surgery.
Therefore,the clinical utility of Neo-CRT regimens should be re-evaluated to make the best of their advantages,while avoiding their various disadvantages.Also,it is unclear whether it safe to selectively omit chemoradiation for RC patients with clinical evidence of a response to neoadjuvant chemotherapy(Neo-CT).For these reasons,many clinical trials have been carried out to explore the optimization of neoadjuvant therapy without radiation[3-6].The FOWARC study(mFOLFOX6 with or without radiation in neoadjuvant treatment of LARC)claimed that perioperative mFOLFOX6 alone followed by TME,led to a similar downstaging rate as CRT but with less toxicity,fewer postoperative complications,and a lower pathological complete response(pCR)rate than CRT.Preoperative FOLFOX/bevacizumab is reportedly a safe and effective treatment option for patients with LARC,as this regimen achieved a better clinical response,pCR rate,and local recurrence rate than consistent use of CRT.
Although Neo-CT alone has shown promising results,many studies failed to compare Neo-CT with Neo-CRT,and the data tended to be limited or were collected from relatively small studies.In the present study,a meta-analysis of related clinical studies was performed to evaluate the pCR rate,sphincter preservation rate,incidences of anastomotic fistula and temporary colostomy,tumor downstaging rate,overall complications,urinary complications,and OS of RC patients receiving Neo-CT with or without radiotherapy.Ultimately,the aim of this meta-analysis was to provide a summary and reference for future research and treatment.
MATERIALS AND METHODS
Search strategy and inclusion/exclusion criteria
The meta-analysis was conducted in accordance with the preferred Reporting Items for Systematic Review and Meta-analysis guidelines.The Cochrane,EMBASE,and PubMed databases were systematically searched for relevant articles published from 1964 to 2020 using the following search terms “rectal neoplasm,” “chemotherapy,” and“radiotherapy.” Wu P and Zhu Z conducted the searches independently.
The diagnoses of all patients were pathologically confirmed as primary RC with or without metastasis.For all patients,if Neo-CT was deemed unnecessary,then neoadjuvant radiotherapy was selected.All studies included related data of endpoints,such as OS,pCR,sphincter preservation rate,or tumor downstaging rate.If related data could not be extracted,the study was excluded from analysis.The quality of all studies was deemed as medium or high.The study design(e.g.,randomized control trial or cohort study)was not considered in the selection process.The sample size of all studies was greater than 20 patients.
Quality of studies and end points
The quality of the randomized control trials,including randomization,concealment of allocation,double-blinding,withdrawals,and dropouts,was evaluated using the Modified Jadad Score.Meanwhile,the Newcastle Ottawa Scale was applied to assess the quality of the cohort studies based on three items:Selectivity,comparability,and outcome.The primary endpoint was OS,the secondary endpoints were the pCR rate,
sphincter preservation rate,incidences of anastomotic fistula and temporary colostomy,tumor downstaging rate,overall complications,and urinary complications.
Data extraction and statistical analysis
The hazard ratio(HR)was used to estimate OS,while the risk ratio(RR)was applied to evaluate pCR,sphincter preservation rate,incidences of anastomotic fistula and temporary colostomy,tumor downstaging rate,overall complications,and urinary complications.The HRs were extracted directly from the studies or from a Kaplan–Meier curve generated with the Engauge Digitizer(http://digitizer.sourceforge.net/).Moreover,a credibility interval was calculated based on the HR and probability(P)value,as described by Tierneyet al[7],and an I statistic(I2)>50% andP<0.05 were considered to indicate significant heterogeneity.In this case,a random effects model was used for analysis.Sensitivity analysis was conducted to explore the source of heterogeneity in all studies.Subgroups were created to lower heterogeneity and identify factors influencing the final results.Furthermore,possible publication bias was assessed using the Egger’s and Begg’s tests,whereP<0.1 was regarded as confirmation of significant publication bias.
Images were processed with the Engauge Digitizer and Adobe Photoshop CC 2018(Adobe Inc.,San Jose,CA,United States).Furthermore,all data analyses were conducted using STATA 14.0 software(Stata LLC,College Station,TX,United States).APvalue <0.05 was considered statistically significant.
RESULTS
Study characteristics and quality
A total of 22087 potentially relevant articles were retrieved from the PubMed,Cochrane,and EMBASE databases.After exclusion of duplicate articles,case reports,meta-analyses,and reviews,the titles,abstracts,and full texts of the articles were screened.Finally,19 articles(6 randomized control trials[8-14]and 13 cohort studies[15-27],Figure 1)with 60870 patients met the eligibility criteria and were included in the meta-analysis.In total,2908 and 57962 patients had been treated with Neo-CT alone and Neo-CRT,respectively.The characteristics of the included studies(i.e.,first author,year of publication,sample size,tumor stages,surgery regimens,chemotherapy regimens,and radiotherapy regimens)are shown in Table 1.The corresponding study was represented using the last name of the first author plus the year of publication.The quality of all studies was deemed medium or high(Figure 2).
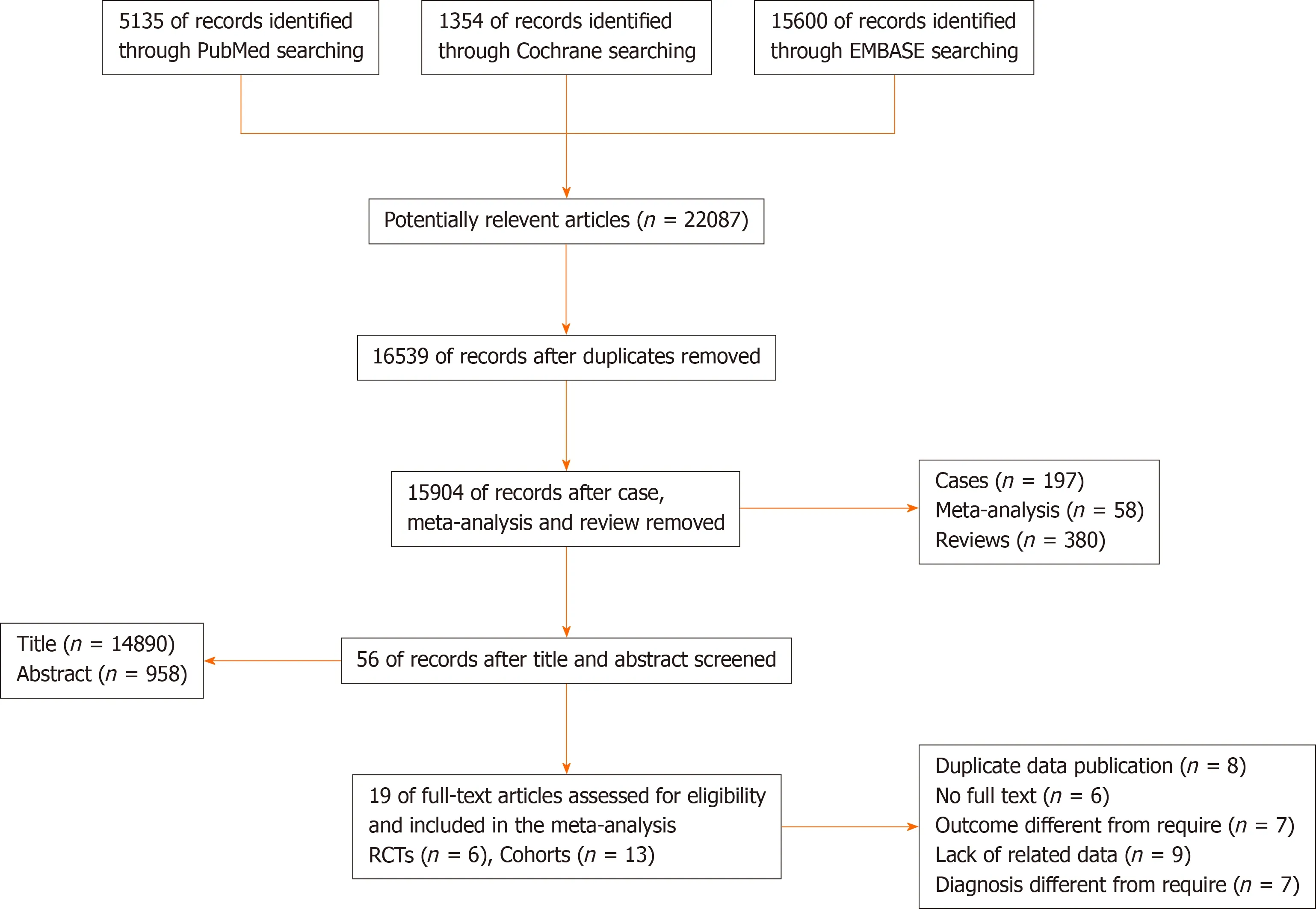
Figure 1 Flow diagram.RCT:Randomized controlled trial.
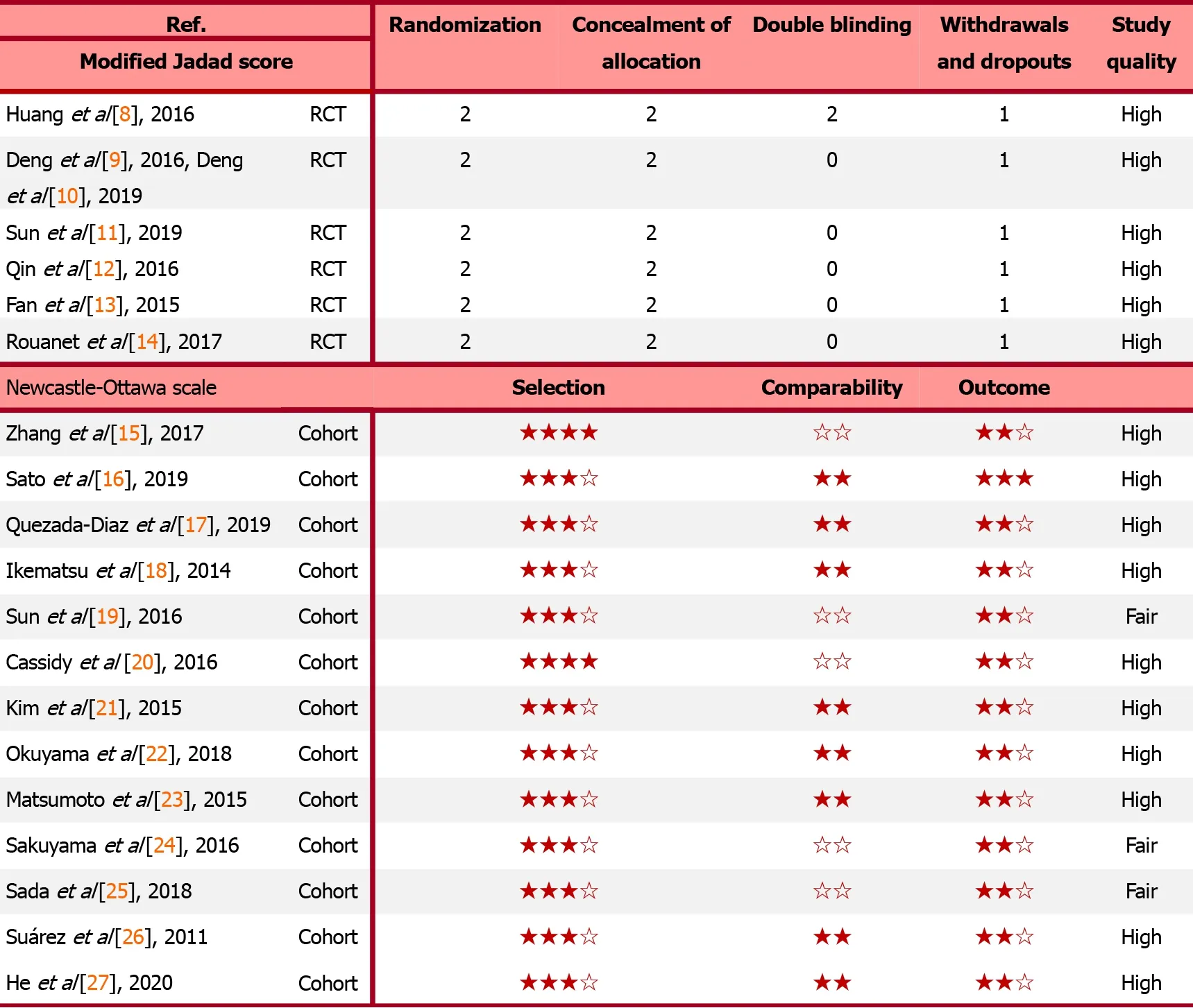
Figure 2 Quality of randomized controlled trials and cohorts.RCT:Randomized controlled trial.
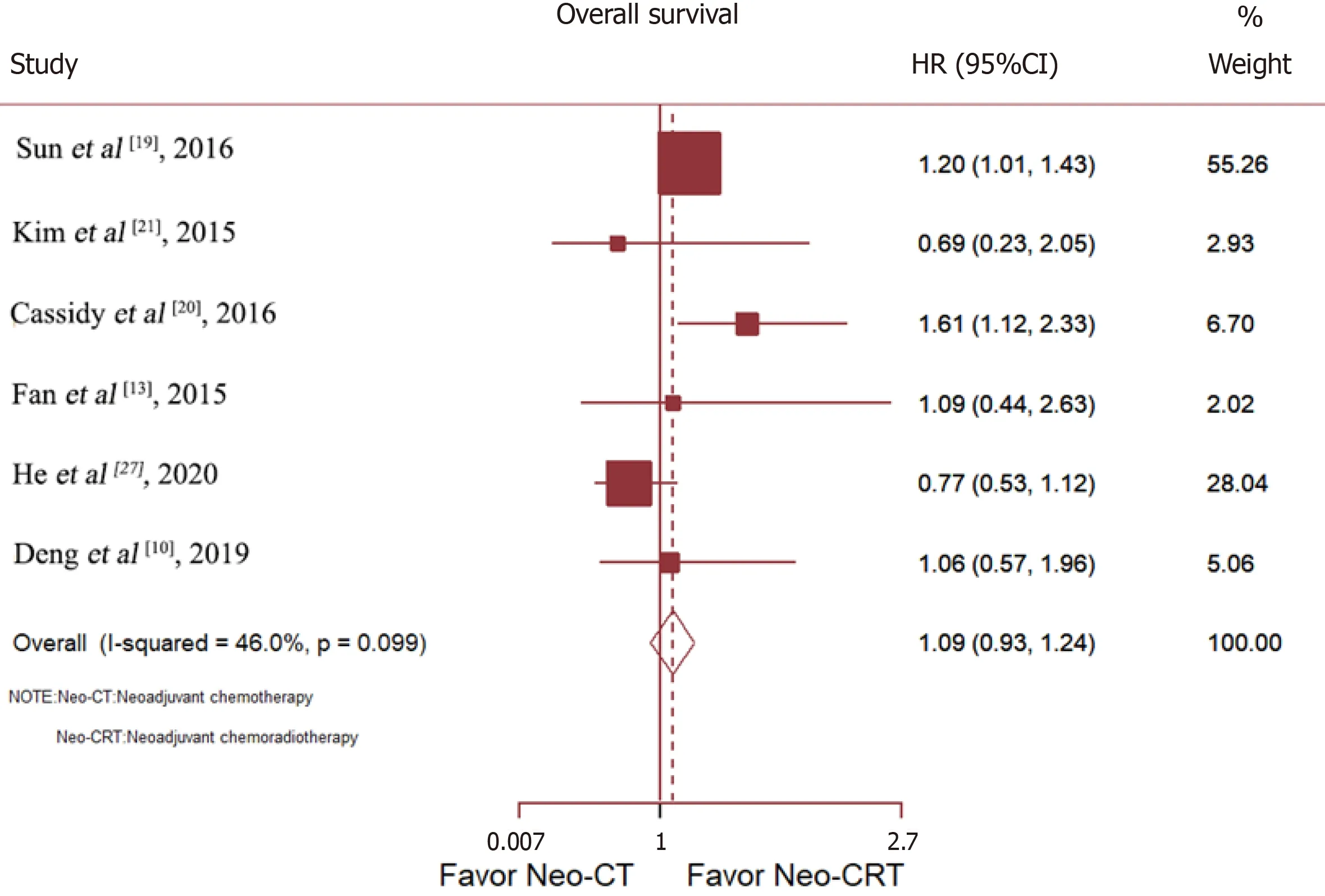
Figure 3 Neoadjuvant chemoradiotherapy improved overall survival of rectal cancer patients based on a meta-analysis of six studies.CI:Confidence interval;HR:Hazard ratio;Neo-CRT:Neoadjuvant chemoradiotherapy;Neo-CT:Neoadjuvant chemotherapy.
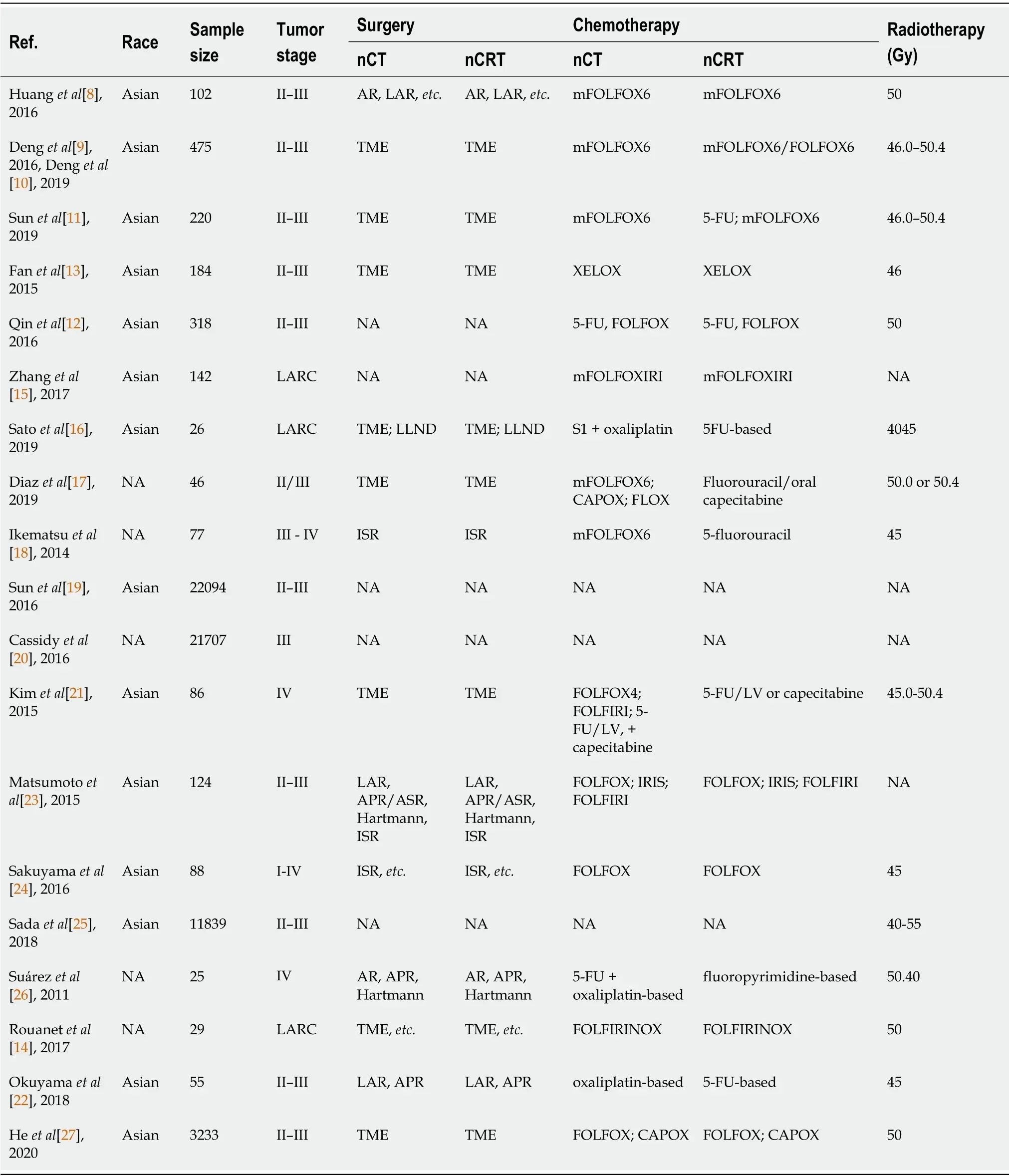
Table 1 Characteristics of all studies
Pooled analysis of HR and RR
Six studies compared the OS of patients with RC treated with Neo-CTvsNeo-CRT.Sunet al[19]and Cassidyet al[20]reported that Neo-CRT improved OS,while Denget al[10],Heet al[27],Fanet al[13],and Kimet al[21]reported no benefit.After merging all studies,Neo-CRT did not improve OS[HR=1.09,95% confidence interval(CI)=0.93–1.24;p=0.19](Figure 3).
Data on the rate of sphincter preservation,incidences of temporary colostomy,and anastomotic fistula were available from nine,three,and six trials,respectively.As compared to Neo-CRT,Neo-CT without radiotherapy was associated with a significant decrease in the incidences of anastomotic fistula(RR=0.49,95%CI=0.35–0.68;P=0.000)and temporary colostomy(RR=0.69,95%CI=0.58–0.83;P=0.000).Moreover,Neo-CT without radiotherapy resulted in a higher sphincter preservation rate(RR=1.07,95%CI=1.01–1.13;P=0.029)(Figure 4).
Neo-CRT had no significant effect on the tumor downstaging rate(RR=0.85,95%CI=0.70–1.03;P=0.088),overall complications(RR=0.66,95%CI=0.37–1.18;P=0.158),or urinary complications(RR=0.84,95%CI=0.25–2.85;P=0.775)(Figure 5).
The pCR rate was available for nine studies with a total of 13005 patients.The results showed that as compared with Neo-CT,Neo-CRT was associated with a significant benefit in the pCR rate(RR=0.67,95%CI=0.52–0.85;P=0.001).However,for all cohort studies,there was no difference in the pCR rate between Neo-CT and Neo-CRT(RR=0.79,95%CI=0.61–1.03;P=0.086)(Figure 6).
Heterogeneity and publication bias
Sensitivity analysis determined high heterogeneity among the pCR rates(I2=56.9%P=0.000).Subsequently,exclusion of the study by Denget al[9]resulted in higher heterogeneity.Finally,there was no significant difference in the pCR rate(I2=38.4%)between the Neo-CT and Neo-CRT groups(Figure 7).
As is shown in Figure 7,there was no significant publication bias in regard to OS(Begg,Pr >|z|=1.000;Egger,P >|t|=0.460),pCR(Begg,Pr >|z|=0.348;Egger,P>|t|=0.399),and the sphincter preservation rate(Begg,Pr >|z|=0.602;Egger,P >|t|=0.191).

Figure 4 Neoadjuvant chemoradiotherapy was associated with lowering incidences of anastomotic fistula and temporary colostomy and increasing the sphincter preservation rate.CI:Confidence interval;nCRT:Neoadjuvant chemoradiotherapy;nCT:Neoadjuvant chemotherapy;RR:Risk ratio.
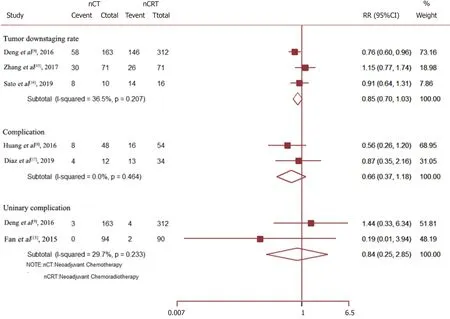
Figure 5 There were no significant differences in the tumor downstaging rate,overall complications,and urinary complications between the neoadjuvant chemoradiotherapy and neoadjuvant chemotherapy groups.CI:Confidence interval;nCRT:Neoadjuvant chemoradiotherapy;nCT:Neoadjuvant chemotherapy;RR:Risk ratio.
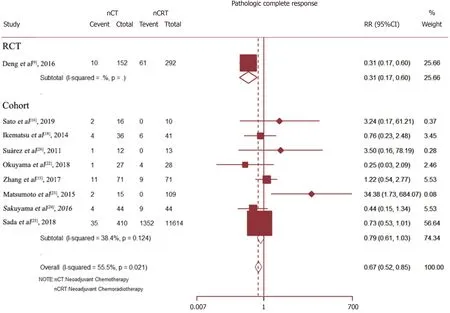
Figure 6 The pathological complete response rate was significantly higher in the neoadjuvant chemoradiotherapy group compared to the neoadjuvant chemotherapy group.CI:Confidence interval;nCRT:Neoadjuvant chemoradiotherapy;nCT:Neoadjuvant chemotherapy;RCT:Randomized controlled trial;RR:Risk ratio.

Figure 7 Publication bias.
DISCUSSION
A Swedish trial conducted in 1997 demonstrated that Neo-CRT improved not only local control,but also OS in Western countries[28].Neo-CRT followed by TME has been adopted as an indispensable treatment regimen for LARC.However,despite the low local relapse rate associated with this treatment regimen,systemic recurrence remains a significant problem,occurring in 30%–40% of patients,along with late morbidities of the bowel,bladder,and sexual function[29].More Japanese and Chinese physicians prefer a preoperative aggressive chemotherapy regimen to suppress distant metastasis and reduce the toxicity of CRT,followed by lateral lymph node dissection,especially for poor risk cases of LARC[30].However,the suitability of Neo-CT without radiation for LARC remains controversial.
To the best of our knowledge,this is the first meta-analysis to compare the efficacy and safety of Neo-CT without radiationvsNeo-CRT for RC patients.This study included 19 randomized control trials or cohort studies published up to September 30,2020.The results showed that Neo-CT could decrease the incidences of anastomotic fistula and temporary colostomy and increase the sphincter preservation rate.Meanwhile,there was no significant difference in OS,the tumor downstaging rate,overall complications,and urinary complications.Although Neo-CT was associated with a higher rate of pCR after merging all trials,there was no significant difference in the pCR rate between the Neo-CT and Neo-CRT groups in all cohort studies.
Most studies of Neo-CRT treatment have demonstrated pCR rates of up to 30%[31-33].For example,the FOWARC study reported a higher pCR rate for fluorouracil alonevspreoperative mFOLFOX6 concurrent with radiotherapy(27.5%vs14.0%,respectively)[9].However,in the present study,there was no significant difference in the pCR rate between the Neo-CT and Neo-CRT groups in all cohort studies(9.5%vs11.6%,respectively,P=0.086),likely because of the chemotherapy regimens.
In contrast,previous randomized trials investigating the addition of weekly oxaliplatin to fluoropyrimidine-based preoperative CRT regimens reported increased acute toxicity without substantial improvements in pCR rates[34,35].A possible explanation for these results was that patients who received a full dose of mFOLFOX6 chemotherapy concurrent with full-dose radiation radiotherapy had a higher rate of treatment compliance than in previous negative trials.The efficacy and varying pCR rate of Neo-CT without radiation have also been associated with regimens involving target drugs and the interval to surgery after chemotherapy.Schraget al[5]treated patients with clinical stage II-III RC with neoadjuvant FOLFOX-based chemotherapy(six cycles of FOLFOX with bevacizumab in the first four cycles)followed by TME and observed a pCR rate of 27%,a R0 resection rate of 100%,and no local failure during a median follow-up period of 18.2 mo.The phase II GEMCAD 0801 trial involving patients with stage II–III RC reported a pCR rate of 15% and a R0 resection rate of 100% after treatment with capecitabine,oxaliplatin,and bevacizumab[36].Specifically,in the N-SOG 03 phase II trial,aggressive chemotherapy regimens(neoadjuvant oxaliplatin and capecitabine plus bevacizumab)reported a pCR rate of 13% and tumor regression rate of 37%,indicating a poor risk of these regimens for RC patients[6].The results of these studies suggested that pelvic external radiation therapy was avoided by selecting appropriate patients with RC other than stage T4 and that the strategy of combining full-dose chemotherapy with multiple agents was more effective.
Pathological stage is still the most reliable predictor of survival of patients undergoing Neo-CRT and surgery,and the pCR status appears to be associated with a favorable prognosis.However,it remains controversial whether Neo-CRT can improve OS.When all studies were merged,there was no significant difference in OS between the two groups(HR=1.09,95%CI=0.93–1.24;P=0.19).Similarly,a Japanese randomized study reported no significant difference in the 5-year survival rate(67.2vs69.2%,respectively)or disease-free survival(DFS)(60.5vs63.0%,respectively)between the treatment and control groups[37].Meanwhile,the results of the JIAO2015 trial showed no significant improvements in OS and DFS,although the rate of distant metastasis was reduced[5].Some researchers believed that the DFS benefit in the CAO/ARO/AIO-04 trial was due to the adaptation of OX-based CT regimens[38,39].Yanget al[40]reported that DFS was marginally but significantly higher in the fluorouracil-based Neo-CRT with OX group than the fluorouracil-based Neo-CRT group,although the distant metastasis rate was significantly decreased in the latter.However,there is no clear consensus regarding whether patients who achieved a pCR should undergo CRT even though the prognosis of these treatments is favorable because the supporting data are rather limited.Nonetheless,patients who achieve a pCR or a clinically significant downstaging to ypT1/T2N0 after neoadjuvant therapy usually have an excellent prognosis.
Although Neo-CRT may improve the pCR rate,the technical difficulty of this regimen is significantly greater due to radiation-induced pelvic fibrosis and the increased risks of surgical complications.Due to these concerns,surgery is often postponed beyond 6–8 wk.However,neo-CRT still leads to temporary ileostomy to prevent anastomotic fistula.Besides,a second surgery is necessary to return the stoma,which severely delays postoperative CT treatment.Moreover,neo-CRT is also considered an independent risk factor for major low anterior resection syndrome[11].The potential adverse events of pelvic radiation in neo-CRT could have long-term impacts on the bowel,bladder,and sexual function,and can destroy bone marrow reserves,while decreasing future tolerance to chemotherapy[41].The results of the present study indicated that Neo-CT without radiotherapy significantly decreased the incidences of anastomotic fistula(RR=0.49,95%CI=0.35–0.68;P=0.000),temporary colostomy(RR=0.69,95%=0.58–0.83;P=0.000)and increased the sphincter preservation rate(RR=1.07,95%CI=1.01–1.13;P=0.029).For these reasons,an RC treatment paradigm that incorporates radiation selectively would be advantageous.
However,LARC is associated with great heterogeneity;therefore,any single treatment modality will not be optimal for all patients.Notably,the choice of treatment should be based on clinical presentations,imaging findings,and molecular biology to precisely stratify patients.Besides,the scheme should be dynamically adjusted according to the therapeutic response to realize the dual goals of prolonging patient survival and improving quality of life.Meanwhile,the choice of treatment for the target population under the guidance of biomarkers should be dynamically and individually adjusted based on the therapeutic effect.This approach will become the future development direction and objective for the precise medical treatment for RC.
There were some limitations to this meta-analysis that should be noted.Although this article provided an up-to-date synthesis of the best available evidence and most of the endpoints contained a medium or large sample size,detailed tumor staging,and different chemotherapy regimens should be further compared to validate the results.Moreover,further studies are needed to explore related endpoints,including the tumor downstaging rate,various complications,and other treatment-related adverse events.Finally,the survival endpoints should be verified in subsequent studies.All in all,owing to the negligible heterogeneity of every endpoint and the inclusion of only high-quality studies,these preliminary results suggested that the combination of fulldose Neo-CT without radiation presented a new neoadjuvant treatment option for LARC.
CONCLUSION
Neo-CT administration can lower the incidences of anastomotic fistula and temporary colostomy and increase the sphincter preservation rate compared to Neo-CRT and could provide an alternative to CRT for LARC.
ARTICLE HIGHLIGHTS
Research background
Neoadjuvant chemoradiotherapy(Neo-CRT)is the current standard strategy for treatment of locally advanced rectal cancer(LARC).However,it delays the administration of optimal chemotherapy and increases toxicity.
Research motivation
This meta-analysis aimed to compare the feasibility and efficacy of neoadjuvant chemotherapy(Neo-CT)vsNeo-CRT for treatment of LARC.
Research objectives
To the best of our knowledge,this is the first meta-analysis to compare the efficacy and safety of Neo-CT without radiationvsNeo-CRT for rectal cancer patients,which included 19 randomized control trials or cohort studies published up to September 30,2020.
Research methods
The hazard ratio of overall survival and the risk ratio for the pathological complete response,the sphincter preservation rate,and treatment-related adverse events were analyzed.
Research results
The results of this study showed that Neo-CT decreased the incidences of anastomotic fistula and temporary colostomy and increased the sphincter preservation rate.Meanwhile,there was no significant difference in overall survival,the tumor downstaging rate,overall complications,urinary complications,and pathological complete response rates.
Research conclusions
Neo-CT was effective for treatment of LARC,especially to lower the incidences of anastomotic fistula and temporary colostomy and increase the sphincter preservation rate as compared to Neo-CRT and could have the potential to provide an alternative to CRT for LARC.
Research perspectives
All in all,owing to the negligible heterogeneity of every endpoint and the inclusion of only high-quality studies,these preliminary results suggested that the combination of full-dose Neo-CT without radiation presented a new neoadjuvant treatment option for LARC.
 World Journal of Gastrointestinal Oncology2021年9期
World Journal of Gastrointestinal Oncology2021年9期
- World Journal of Gastrointestinal Oncology的其它文章
- Use of liquid biopsies in gastrointestinal cancers
- Prognostic value of modified Lauren classification in gastric cancer
- Scoparone inhibits pancreatic cancer through PI3K/Akt signaling pathway
- Effect of oncometabolic surgery on gastric cancer:The remission of hypertension,type 2 diabetes mellitus,and beyond
- Characterization of metabolic landscape in hepatocellular carcinoma
- Immune aspects of hepatocellular carcinoma:From immune markers for early detection to immunotherapy
