Effect of vitamin B12 deficiency anemia on peripapillary retinal nerve fiber layer
Department of Ophthalmology, Shri Guru Ram Rai Institute of Medical and Health Science, Patel Nagar, Dehradun 248001,India
Abstract
● KEYWORDS: vitamin B12 deficiency anemia; retinal nerve fiber layer; spectral domain optical coherence tomography
INTRODUCTION
Vitamin B12 deficiency (BD) is a worldwide problem[1].Vitamin B12 deficiency anemia (BDA) has recently been reported to become endemic in India and it may be as high as 70%-100%, mostly because majority of Indian population is vegetarian by food habits[2-3]. Other than vegetarian/vegan diet, less common causes of BD in adults include autoimmune and parasitic diseases, gastro-intestinal surgery, defect in B12-transport, intrinsic factor deficiency,drugs (metformin, antacids), pancreatic disease, increased physiological demand (pregnancy, lactation), inherited metabolic diseases,etc[3-5]. Chronic BD (not merely sub-normal serum level) may lead to macrocytic megaloblastic anemia as well as various non-specific neurological or neuropsychiatric manifestations or even life threatening atherosclerosis because of increased serum homocysteine level[5-6].
Although hematological abnormalities frequently begin before the onset of neurologic disease, in nearly a quarter of patients these neurological disorders may manifest before or even without hematological abnormalities, making the diagnosis difficult in subclinical BD without anemia[1,7].
Vitamin B12 is a major co-factor in the synthesis of myelin.A chronic BD is definitively proved to cause bilateral optic neuropathy characterized by cecocentral scotoma and eventually loss of vision from optic atrophy, possibly due to derangement of superoxide scavenging mechanism as well as myelin synthesis[1,8]. It is thus prudent to measure the retinal nerve fiber layer thickness (RNFLT) by utilizing optical coherence tomography (OCT) in BDA patients,considering that retinal nerve fiber thinning (RNFL-t) might precede development of frank optic neuropathy, as is the rule in cases with glaucomatous optic neuropathy. Typical pattern of RNFL-t has also been reported in various ischemic retinal diseases, myopia, chronic obstructive pulmonary disease,neurological (e.g., multiple sclerosis, Parkinson’s disease,migraine) and neuropsychiatric illnesses (Alzheimer’s disease)[9].Spectral domain-optical coherence tomography (SD-OCT)is especially known for its capability of enhancing the image resolution, improved quality of measurements, reduced scantime, and reproducibility[9].
Currently, as par our knowledge, RNFLT-study on BDA is scarce. Therefore, the aim of this study was to evaluate the effect of BDA on peripapillary RNFLT in adult patients by SDOCT and to determine any correlation arising thereof. We also tried to correlate peripapillary RNFLT with varying grades of BDA.
SUBJECTS AND METHODS
Ethical ApprovalThis hospital based cross-sectional observational study was carried out for a period of 1.5y(September 2017-February 2019) in the Department of Ophthalmology at a tertiary care multispecialty referral hospital of Northern India, that caters to a large population of this state and neighboring states, as well. Consensus from institutional research ethical committee and patients’ consent were obtained. This study adhered to the tenets of Declaration of Helsinki.
Patients IncludedIn this study, a total of 99 eyes of 50 consecutive clinically diagnosed BDA patients (BDA group)aged 18-65y, who were recruited from the Department of Medicine in- and out-patient clinic, were included. A total 50 age and sex-matched healthy non-anemic subjects were included as controls (control group). Both study and control group comprised of only non-glaucomatous patients who had normal intraocular pressure of <21 mm Hg, open anterior chamber angle, no cup/disc ratio (C/D) abnormalities or documented glaucomatous visual field defects, in both the eyes(including a one eyed patient).
Patients ExcludedPatients with history of external trauma or ocular surgery or laser/injection procedures, best corrected visual acuity (BCVA) of <6/6 (Snellen converted into logMAR), myopia or hypermetropia of >6 diopters, uveitis,pseudoexfoliation syndrome, squint, amblyopia, alcoholism,smoking, systemic diseases other than BDA (diabetes,hypertension, obstructive lung disease, thyroid disorders,Alzheimers, Parkinsonism, multiple sclerosis), structural or organic ocular disease (acquired or congenital), pregnancy,significant ocular media opacity, signal strength of <6 in SDOCT, were excluded.
Diagnostic CriteriaBDA was diagnosed when hematological parameters reported serum hemoglobin (Hb%)<11 g/dL in conjunction with serum vitamin B12<200 pg/mL.Hematological and biochemical measurements were performed using CELLDYN®Ruby (Abbott, USA) and the VITROS®5600 integrated system (Ortho Clinical Diagnostics,USA), respectively. Anemia was graded according to the Hb%level as, mild (Hb%: 9-11 g/dL), moderate (Hb%: 7-<9 g/dL),severe (Hb%: 5-<7 g/dL) and very severe (Hb%: <5 g/dL).
Examination ProcedureOnce included, each patient (both study and control group) underwent detailed history taking followed by comprehensive ocular examination. Ocular examination was done by a single blind observer, that included assessment of BCVA, refraction by auto-refracto-keratometer(ARK-1, Nidek Co. Ltd., Japan), slit-lamp biomicroscopy(Haag-Streit), tonometry (Goldmann applanation tonometry),perimetry (Humphrey Visual Field Analyser; Carl Zeiss Meditec Inc. Dublin, CA, USA), fundoscopy with 90D and 20D-lens, and RNFLT assessment by SD-OCT (RS-3000 Nidek Gamagori, Aichi 443-0038, Japan). Peripapillary RNFLT-scans were obtained for the mean total, inferior,superior, nasal and temporal quadrants using optic disc 200×200 pixels on 6×6 mm2cube scan protocol within 3.45 mm diameter centered on the optic nerve head. During scan, best possible fixation was ensured in each case after full dilation of the pupil by a combination of 0.8% tropicamide and 5%phenylephrine eye drops.
Statistical AnalysisAll collected data were recorded on Microsoft Excel Windows 10 (USA), and then analyzed using SPSS software (version 21.0, SPSS Inc., Chicago, IL, USA).The quantitative data was expressed as mean with standard deviation (SD). Categorical and nominal data was expressed in percentage. Quantitative data (intra-group analysis) was analyzed using Pairedt-test, non-parametric data by using Mann-WhitneyUtest, and categorical data by using Chisquare test. Pearson’s correlation coefficient analysis was used for correlating intra-group quantitative variables. Statistical significance was set atP<0.05.
RESULTS
Baseline Characteristics of BDAvsControl GroupIn the present study, the mean age, gender distribution, vertical C/D ratio,rim area, and disc area between the BDA and control group patients were comparable (P>0.05). Serum iron, ferritin and folic acid levels were also found comparable (P>0.05),however, serum Hb%, vitamin B12 and mean corpuscular volume (MCV) level were significantly different (P<0.05).None of the patients in either group had detectable visual field defects (Table 1).
RNFLT of BDAvsControl GroupFor BDA cases, except superior RNFLT (121.62±10.03 μmvs123.23±8.13 μm,P=0.214),there was significant RNFLT of the mean total, inferior,nasal and temporal quadrant, as compared to the controls(92.26±8.0 μmvs97.28±5.06 μm,P<0.001; 119.11±11.8 μmvs126.03±7.88 μm,P<0.001; 69.74±8.30 μmvs74.82±6.02 μm,P<0.001; 63.28±7.87 μmvs66.20±6.10 μm,P=0.003;respectively; Table 1).
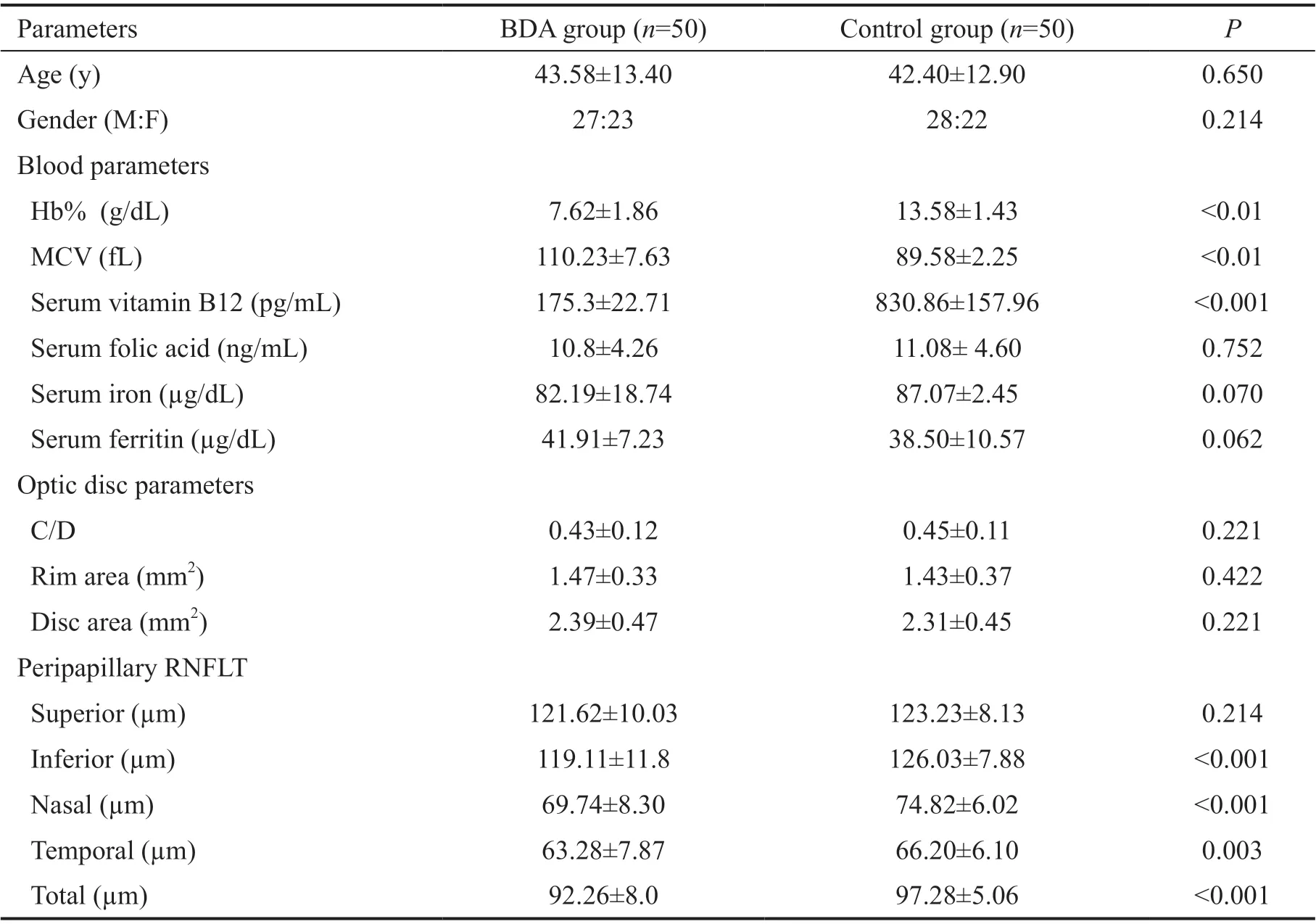
Table 1 Baseline demographic, hematological and clinical characteristics of the BDA and control group mean±SD
RNFLT and Blood ParametersSerum Hb%, B12, and MCV level correlated significantly (P<0.05) with the mean total (r=0.310, 0.435, -0.386; respectively), inferior (r=0.932,0.481, -0.513; respectively) and nasal RNFLT (r=0.344, 0.254,-0.233; respectively). However, no significant correlation could be established (P>0.05) in the superior (r=0.111, 0.070, -0.099;respectively) and temporal RNFLT (r=0.144, 0.167, -0.096;respectively; Table 2; Figure 1).
RNFLT andSeverity of BDAAccording to the severity of BDA, there were 16 (32%) mild, 14 (28%) moderate and 15 (30%) severe grade of BDA patients, while only 5 (5%)had very severe anemia who required extensive evaluation by the physician. Mean total RNFL-t in all BDA group cases showed progression with the increasing severity of anemia,except in very severe BDA, where an inverse relationship was documented (Figure 2). None of the patients required bone marrow examination, as neither was detected to have pancytopenia or features of non-megaloblastic anemia.
DISCUSSION
Although, BD is prevalent in almost every race throughout the world including central Europe and Western countries,it is recently reported to be endemic in India[1-2]. The latest National Family Health Survey (NFHS 4) carried out by the Ministry of Health and Family Welfare in India reported that the prevalence of anemia amongst Indian women aged 15-49y and men aged 15-49y was 53.1% and 22.7%, respectively[2].The diagnosis of subclinical BD without anemia is difficult[1-2].Elderly patients are more prone to develop BD due to atrophic gastritis, malabsorption or insufficient dietary intake. Although currently there is no internationally accepted standard for diagnosis of BD, serum concentrations of vitamin B12 is a relatively good indicator of body store[10].
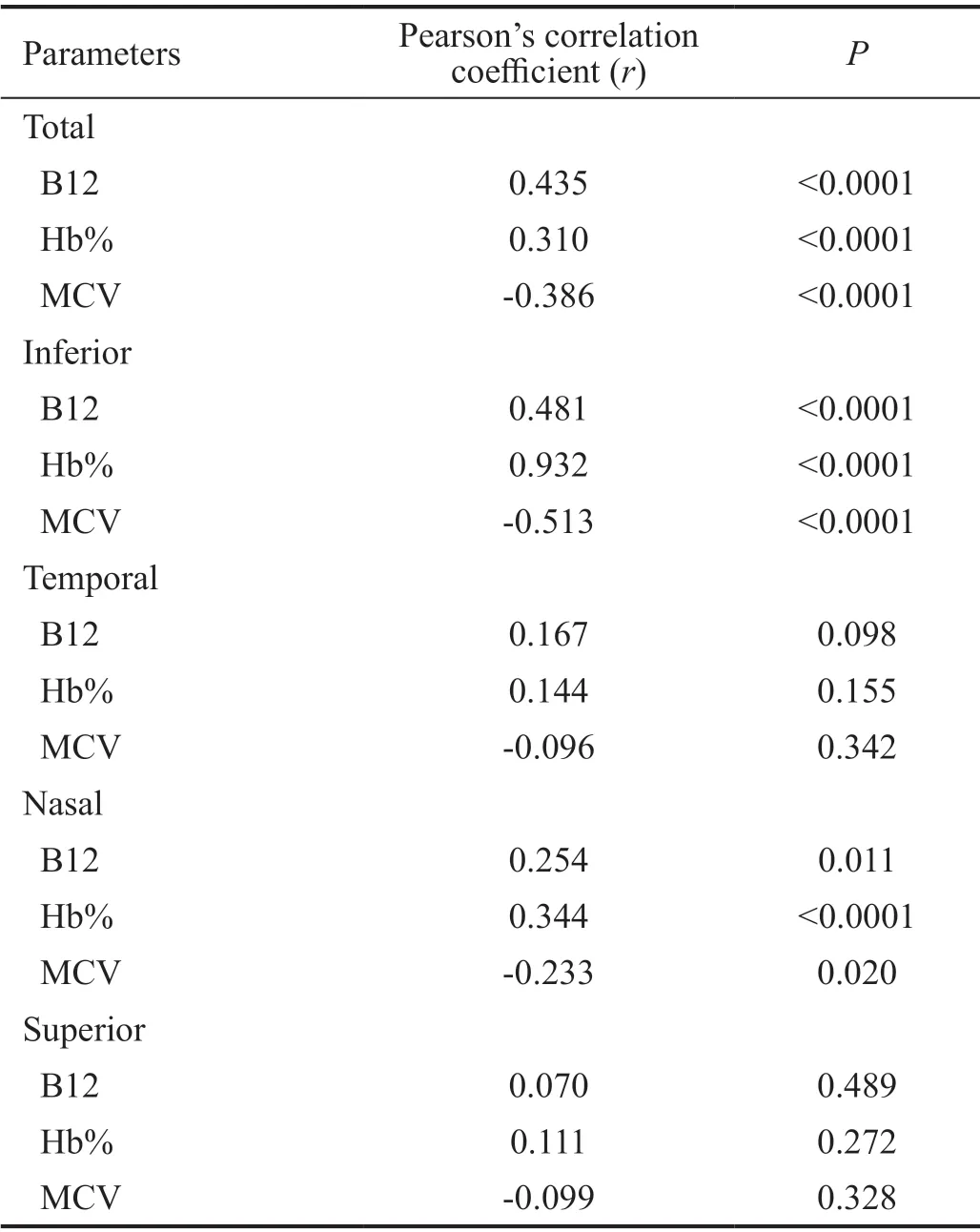
Table 2 Pearson’s correlation between RNFLT with blood parameters in BDA group of patients
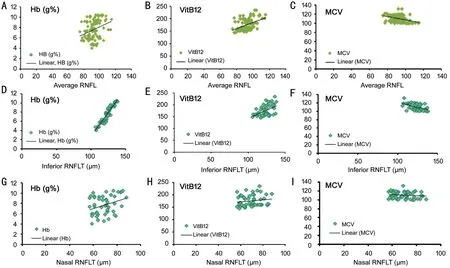
Figure 1 Pearson’s correlation of the hematological parameters (serum Hb%, vitamin B12 and MCV) in BDA group of patients with the mean total RNFLT (A, B, C, respectively), inferior RNFLT (D, E, F, respectively), and nasal RNFLT (G, H, I, respectively).
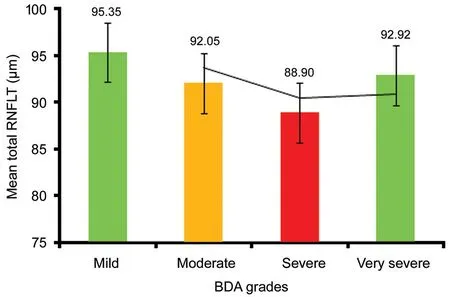
Figure 2 The mean total RNFLT values in different grades of BDA patients Only eight (0.16%) BDA patients had associated nonspecific neurological features that were mostly limited to paresthesia of extremities, movement disorders, auditory symptoms, and mental depression.
Initial clinical manifestations may be of non-specific neurological nature, may precede hematological manifestations, and may take 5-6y after the onset of BD[11]. Additionally, due to difficulty in laboratory diagnosis, results even from standard laboratories are not reliable due to several reasons[5,12]. This study was undertaken with an aim to evaluate the effect of BDA on peripapillary RNFLT using SD-OCT. To the best of our knowledge, currently there is no such similar study yet published, other than handful of studies which are mainly based on the sub-normal BD without anemia, and that too on elderly susceptible group is very limited[1,12-13].
Significant global, inferior, temporal, nasal and insignificant superior peripapillary RNFL-t was the hallmark of this study.Currently, there is no supportive data available worldwide.However, working with non-anemic BD patients, different authors reported varying results. Türkyılmazet al[13]in their study group of younger patients reported significant mean total and temporal RNFL-t as measured by Cirrus HD-OCT(mean age=31y, serum B12 cut off ≤189 pg/mL); Doganet al[12]reported insignificant RNFL-t of mean total and superiortemporal as measured by Spectralis-OCT with a B12-deficient cut off level ≤200 pg/dL; Özkasapet al[1]reported significant superior but insignificant mean total RNFL-t as measured by Cirrus HD-OCT in children (mean age 12.9±2.4y, serum B12<200 pg/mL). Inclusion of variant age groups, sample size,B12-cut off level, duration and severity of deficiency, OCTtechniques and exclusion of anaemia might be the possible cause for such differences. In this study, except temporal and superior RNFLT, global, inferior and nasal RNFLT correlated significantly (P<0.05) with the corresponding blood parameters(serum B12, Hb%, MCV level). At present, there is no relevant study available to testify this. However, in studies with BD in non-anemic subjects, Turkimalyzet al[13], Doganet al[12]and Özkazapet al[1]have found correlation of serum B12 with mean total and temporal RNFLT, supero-temporal RNFLT, and mean total and superior RNFLT, respectively. Variation in the nature of the study as already explained, as well as geographic and age-related variation in retinal thickness, possibly played a role for such differences.
In this study, except in the very severe grade of BDA patients,an exponential mean total RNFL-t was observed in all other grades (mild, moderate and severe) which was at par with the advancement of severity of anemia. This although conforms to the study by Hanet al[14]who reported RNFL-t corresponding to the exponential decrease of Hb% level, an existence of inverse relationship between the severity of anemia and degree of neurological features has also been reported by Healtonet al[15]. Further similar large-scale studies may certainly throw some light in causation of such paradox. None of our study subjects had visual deterioration or perimetrically proven visual field defects.
Pandeyet al[16]in their study on chronic persistent BD patients(with or without anemia), reported prolongation ofP-100 latency as recorded by visual evoked potential in 58% (10/17)of their study participants, even though they all were having normal visual acuity, which they inferred to be due to chronic demyelination and remyelination processes. Turkimalyzet al[13]also had similar observation with their study group of BD patients without anemia. This prompted us to believe that the pattern of RNFL-t in BDA reflects pre-perimetric early structural damage (demyelination), which deserves urgent attention to rule out other causes of non-glaucomatous optic neuropathy and thus initiate preventive measures to arrest irreversible axonal damage.
This study was possibly limited by its cross-sectional nature that restricted us to study the effect of vitamin B12 supplementation on RNFLT, duration of anemia could not be ascertained due to lack of information provided by the patient and by our inability to perform sophisticated tests like, GIendoscopy, MRI-spinal cord, methylmalonyl coenzyme test,serum homocysteine estimation,etc., either because of the cost-factor or non-availability. Nevertheless, the characteristic changes as observed in this study may have enormous clinical significance.
To conclude, in the current study, SD-OCT showed a significant peripapillary RNFL-t of the mean total, inferior,nasal, and temporal quadrant in BDA patients, as compared to their age and sex-matched healthy non-anemic controls. The RNFLT of mean total, inferior and nasal quadrant significantly correlated with the relevant hematological parameters (serum Hb%, B12 and MCV level). Although, mean total RNFLT showed a graded thinning response at par with progression of severity of anemia, its inverse relationship in very severe grade of BDA patients was a notable exception in this study.RNFL-t can progress with the progression of anemia even without showing signs of optic neuropathy or obvious visual field changes, and this can be an ominous sign. SD-OCT thus may prove to be a valuable tool for early detection of RNFL-t in BDA patients and can aid in preventing further irreversible neurological sequelae by identifying high risk patients who require prophylactic therapy, and also in differentiating from other non-glaucomatous optic neuropathies. Further similar prospective, multicenter, randomized studies with bigger cohort would be warranted to better understand and characterize the changes imposed and also to determine the effects of treatment in BDA patients.
ACKNOWLEDGEMENTS
Conflicts of Interest: Das Gupta S,None;Shakeel T,None;Dhawan A,None;Kakkar A,None.
 International Journal of Ophthalmology2021年9期
International Journal of Ophthalmology2021年9期
- International Journal of Ophthalmology的其它文章
- Five-year results of refractive outcomes and visionrelated quality of life after SMlLE for the correction of high myopia
- One-step viscoelastic agent technique for lCL V4c implantation for myopia
- miRNA-26b suppresses the TGF-β2-induced progression of HLE-B3 cells via the PI3K/Akt pathway
- Pediatric ocular trauma with pars plana vitrectomy in Southwest of China: clinical characteristics and outcomes
- Socio-economic disparity in visual impairment from cataract
- Disseminated hydatid disease in the orbit and central nervous system
