Pediatric ocular trauma with pars plana vitrectomy in Southwest of China: clinical characteristics and outcomes
Zuo-Xin Qin, Yan He, Yu-Fei Xu, Tao Yu, Yong Liu, Nan Wu
1Southwest Hospital/Southwest Eye Hospital, Third Military Medical University (Army Medical University), Chongqing 400038, China
2Key Lab of Visual Damage and Regeneration & Restoration of Chongqing, Chongqing 400038, China
Abstract
● KEYWORDS: pediatric; ocular trauma; vitrectomy;outcome
INTRODUCTION
Ocular trauma is one of the major causes of acquired monocular blindness in children[1-3]. It was reported that the incidence of severe visual impairment or blindness caused by ocular trauma was 2% to 14% in children[4-5]. Vision loss has long-term social and psychological impact[6]. Therefore, it is necessary to evaluate the epidemiological characteristics of ocular trauma in children and reduce its morbidity and severity.To our best knowledge, there are limited literatures focusing on severe ocular trauma in children.
Pars plana vitrectomy (PPV) is a common employed technique in vitreoretinal surgery that has been used to treat conditions like severely ocular trauma[7]. Though some studies reported the epidemiological features and outcomes of surgical repair in pediatric ocular trauma[8-9], describing the clinical characteristics and outcomes of PPV in pediatric ocular trauma is lacking, especially in Chinese population. This study recruits the largest number of pediatric ocular trauma patients who receive PPV treatment in southwest China, and investigates the clinical characteristics and outcomes of these children. The prognostic factors of visual outcomes are also examined in the study.
SUBJECTS AND METHODS
Ethical ApprovalThe medical records of children diagnosed with ocular trauma from January 2007 to December 2017 in Southwest Hospital, Chongqing, China, were retrospectively reviewed. This retrospective study was approved by the ethics committee of the Southwest Hospital (KY201858) and followed the tenets of the Declaration of Helsinki. Informed consent was waived due to the retrospective nature of the study.
This study included children with ocular trauma who were less than 14 years old and received PPV treatment. Patients with anterior vitrectomy only were excluded. Patients who were followed up for less than 6mo were excluded. The following data of ocular trauma were collected: demographics including age, gender, and injury time; characteristics of injury including cause, mechanism, types, wound locations, and sizes;ophthalmological examinations including initial visual acuity(VA), slit lamp examination, B-scan, and fundus examination if possible; surgical intervention including the type and number of surgeries and intraocular tamponades; follow-up data including final VA and final anatomic outcomes of eyes.
The classification of ocular trauma is based on the Birmingham Eye Trauma Terminology (BETT)[10]. It is divided into open globe injury and closed globe injury. Open globe injuries include rupture, perforation, intraocular foreign body and penetrating. VA was recorded as the best corrected vision acuity using the Snellen acuity when possible. VA was graded in accordance with the published visual acuity grade set up by The Ocular Trauma Score[11]. Unfavorable anatomic outcome is defined as enucleation or evisceration of the eyeball, atrophy of the eyeball, inoperable retinal detachment, or long-term silicone oil-sustained. Unfavorable visual outcome is defined as eyes with the final VA less than 1/200 after 6mo follow-up.Statistical AnalysisAll analyses were performed by SPSS software (version 20.0, IBM, USA). Descriptive analysis, Chisquare test and binary Logistic regression analysis were used.The distribution of patients’ age and follow-up time were illustrated by descriptive analysis. The ratio of unilateral eyes,gender, anatomical outcomes, and visual outcomes between different groups were analyzed by Chi-square. The significant factors affecting the prognosis of vision outcomes were analyzed by univariate analysis and binary Logistic regression analysis.Pvalue less than 0.05 was considered statistically significant.
RESULTS
Totally 874 children with ocular trauma were hospitalized between January 2007 and December 2017, of whom 139 cases underwent vitrectomy, accounting for 15.9%. The demographic information of these 139 patients was presented in Table 1. The mean age was 7.4±3.7y (range 1-14) and the mean follow-up time was 18.1±19.4mo (range 6-104mo). All the cases were unilateral and no significant difference was obtained between the left eye and right eye (74 right eyes and 65 left eyes,P=0.445). A total of 116 (83.5%) cases were male and 23 (16.5%) cases were female (P<0.05). The age and gender distribution of the patients were shown in Figure 1.
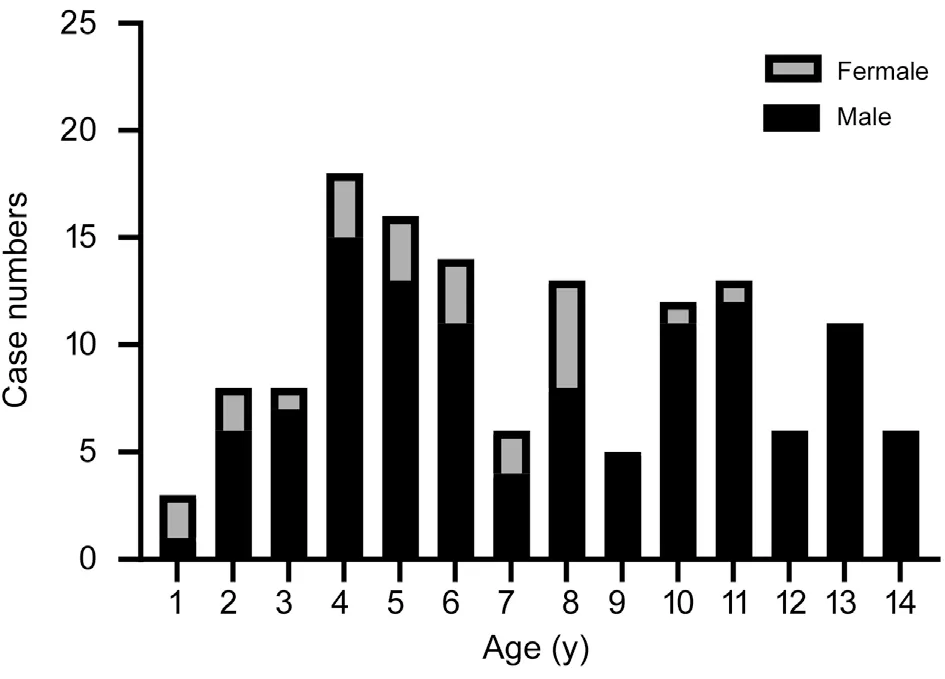
Figure 1 The age and gender distribution of pediatric ocular trauma patients.
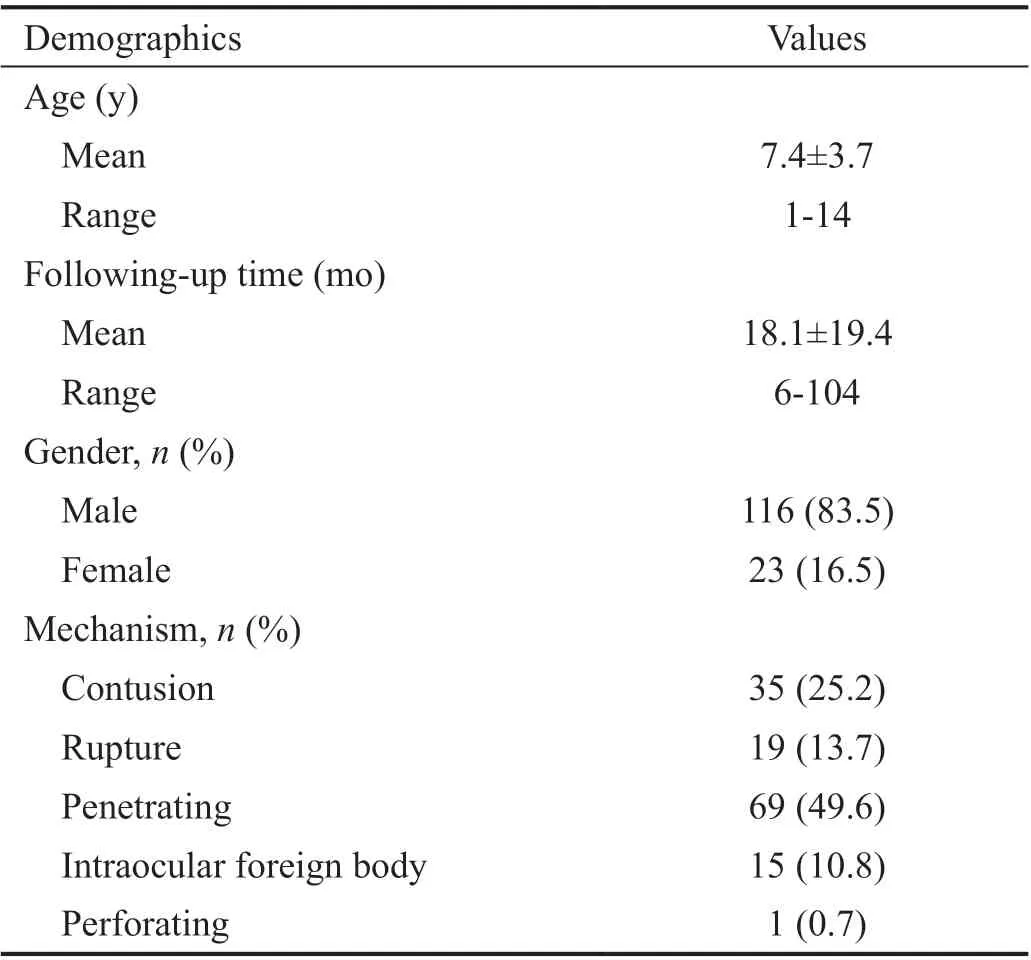
Table 1 Demographics of patients who received PPV after globe injury
Of the 139 patients, 35 (25.2%) suffered closed globe injuries and 104 (74.8%) experienced open globe injuries. Among the open globe injuries, there were 19 cases of eye rupture, 69 cases of penetrating injuries, 15 cases of intraocular foreign body, and 1 case of perforation injury. Penetrating injuries accounted for 49.6% (69/139), which was the main contributor of globe injuries in our study.
The time distribution of injuries was shown in Figure 2.Compared with other times, the incidence in January and February was significantly higher (35% of total cases).
The causes of injuries were shown in Table 2. The three main causes were sharp metal objects (43.9%), wooden sticks(13.7%) and fireworks (11.5%). Sharp metal objects mainly included scissors, knives, needles, and nails. With regards to toys, toy bullets and slingshots were the most dangerous toys that can lead to severe ocular trauma. Besides, the cause of injuries was not clear in six children.
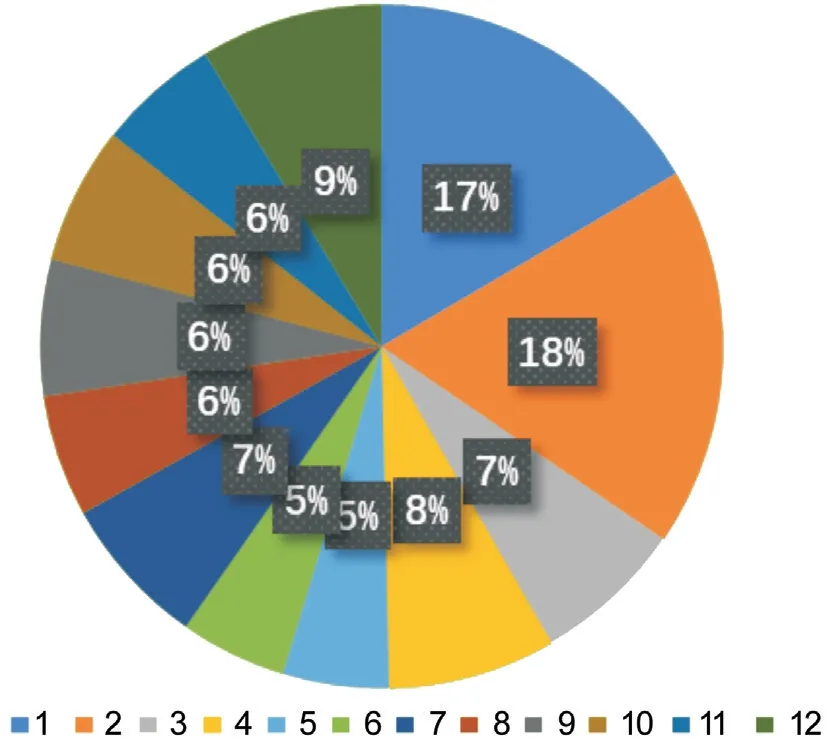
Figure 2 Time distribution of injuries in a year.
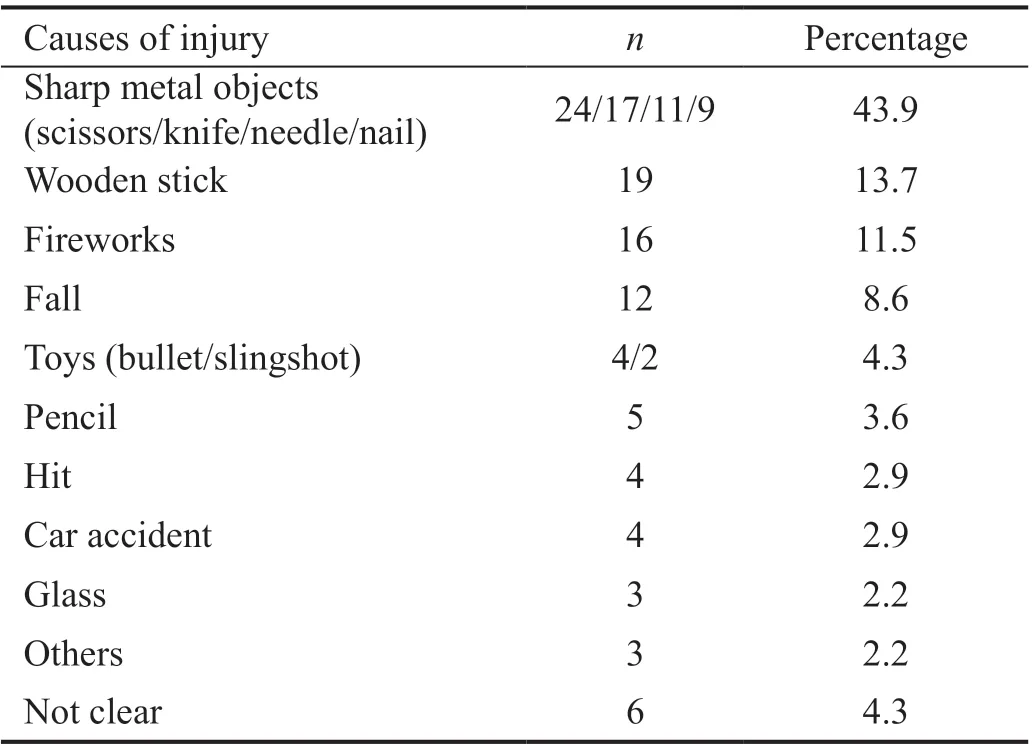
Table 2 Causes of ocular trauma in pediatric patients
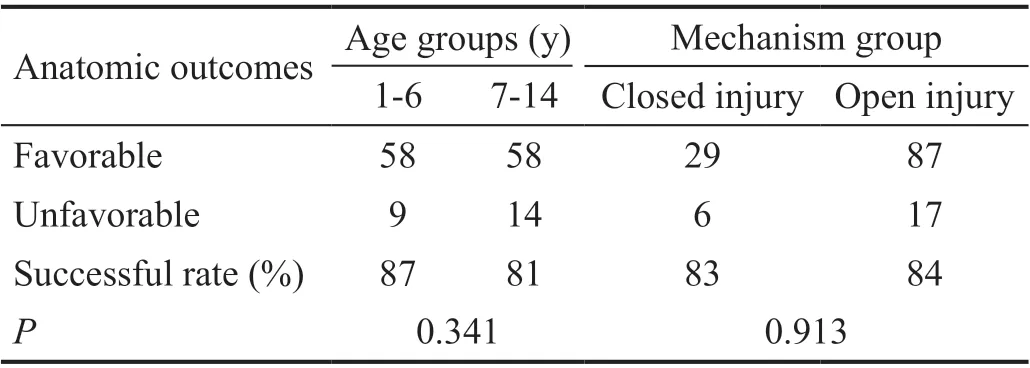
Table 3 Anatomic outcomes of different age and mechanism groups
Anatomic outcomes of these injured eyes were shown in Table 3. At the last follow-up, 116 out of the 139 patients had favorable anatomic outcomes. Among the 23 eyes with unfavorable anatomic outcomes, three ended up with enucleation, one had atrophy, and the other 19 were subjected to silicone oil-sustained treatment for unrecoverable recurrent retinal detachment. There was no significant difference(P=0.341) with respect to the incidence of unfavorable anatomic outcomes between the 1-6y group and the 7-14y group. There was no significant difference (P=0.913) for the cases between the closed globe injury group and the open globe injury group.
The comparison of the initial VA and the final VA was shown in Table 4. Eleven patients (7.9%) were not cooperative to obtain accurate initial VA. However, the final VA was obtained in all cases except for three cases of enucleation. Only 15 patients (10.8%) had initial VA better than 1/200. After treatment, 73 (52.5%) had final VA better than 1/200 after PPV,and only 30 patients (21.6%) achieved 20/200 or better.
The predictive factors for the final VA were shown in Table 5.Univariate analysis showed zone Ⅲ injuries (P=0.021), poor initial VA (P=0.005), endophthalmitis (P=0.024), and recurrent RD (P<0.001) were the poor prognostic factors for pediatric ocular trauma with significance. Other factors such as age,gender, type of injury, wound length, retinal detachment,vitreous hemorrhage, time between injury and vitrectomy failed to show significant effect on final VA.
The results of multivariate Logistic regression analysis were presented in Table 6. Poor initial VA and recurrent retinal detachment were significantly correlated with unfavorable visual outcome. The odds ratio was 8.276 (95%CI: 1.597-42.897,P=0.012) and 6.455 (95%CI: 2.372-17.562,P<0.001),respectively.
DISCUSSION
Ocular trauma is one of the most common causes of acquired blindness in children. The pediatric ocular trauma is subjected to high risk of severe visual impairment or permanent visual loss if not managed properly. In addition, the severe ocular trauma in children places a heavy burden on both families and society. Even with treatment, the outcomes of pediatric ocular trauma are usually difficult to predict[12]. In this study,we recruited patients who were under 14 years old and underwent vitrectomy due to severe ocular trauma in the past 11y, and analyzed their demographics, clinical characteristics,and prognostic risk factors for visual outcomes. This study will provide direct evidence for early prevention and clinical management of pediatric ocular trauma.
In terms of demographics, it is well appreciated that a higher incidence of ocular injury occurred more in boys than girls[1,13].Consistent with this, our study found that the ratio of males to females is 5:1. Boys were more likely to have ocular injuries.This is perhaps because they are more mischievous and difficult to be supervised.
Regarding causes of injuries, our finding was consistent with previous reports that penetrating injury caused by sharp objects was in absolute predominance in pediatric ocular trauma[14-17].Previous reports showed that 90% of all ocular trauma was avoidable[17]. Therefore, figuring out the major causes of ocular injury will help to reduce the risk of ocular trauma in children and protect vision. Wear protective eyewear or goggles during risky activities and supervise using of sharp objects are the main approaches to prevent serious pediatric ocular trauma.
With regards to the time distribution of ocular trauma in our study, 35% of cases occurred in January and February. This is directly associated with children playing with fireworks in Chinese Spring Festival[16]. This was also showed as one of the main causes of injury in our study.

Table 4 Comparison of initial VA and final VA

Table 5 Predictive factors for final VA
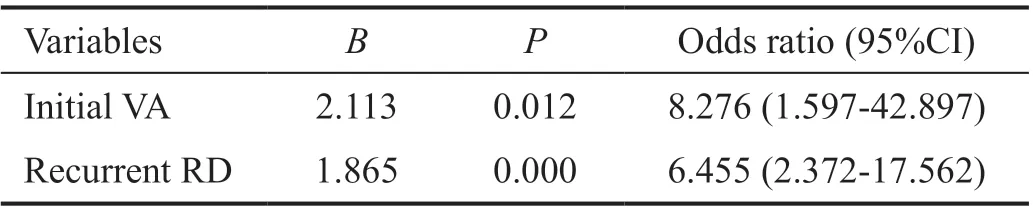
Table 6 Prognostic factors for final VA developed by Logistic analysis
At the last follow-up, 116 patients had favorable anatomic outcomes at a rate of 83.5%, similar to other reports[18]. In disagreement with previous reports[19-20], age and injury types did not affect anatomical outcomes in our study. This may be related to a small sample size in our study.
With respect to visual outcomes, only 15 patients (10.8%)presented with 1/200 or better initial VA. Indications for PPV were intraocular foreign bodies, endophthalmitis, severe vitreous hemorrhage, traumatic retinal detachment, and other severe posterior ocular injuries. In this study, 28 patients underwent vitreoretinal surgeries more than twice for recurrent retinal detachment. Finally, 73 patients (52.5%) achieved vision of 1/200 or better, and 30 patients (21.6%) achieved 20/200 or better. The percentage of favorable visual outcomes was lower than other reports[19]. Despite this, vitreoretinal surgery is still an effective method to treat severe ocular trauma in children. With wide use of PPV and improvement of this technique, PPV has not only preserved the severe damaged eyes that would have been enucleated but also saves vision of many eyes, as reported previously[21].
In our study, we found wounds involving zone III had significantly poorer visual outcomes versus those involving zone I or II (P=0.021). This would be clinically expected, as posterior segment injury can cause irreversible damage to the retina of posterior pole and thus render a poor visual prognosis,albeit the structure of the globe had been repaired[22]. In our study, 40 patients developed endophthalmitis, of which 25 (62.5%) had poor visual outcome (P=0.024). Previous study has reported that visual outcome of posttraumatic endophthalmitis in children was poor[23-24]. Fenget al[7]had reported that endophthalmitis was an independent risk factor for poor VA after vitrectomy in pediatric ocular trauma.Furthermore, our regression analysis showed that initial VA and recurrent retinal detachment were independent risk factors for final visual outcomes. It had been reported that the initial VA had a significant impact on the prognosis of visual outcome. This is because the initial VA usually represents the degree of ocular damage. The worse the initial vision, the severer the damage. Therefore, it’s rational to check the initial VA to better predict the visual outcomes.
Moreover, recurrent retinal detachment was also strongly related to finial visual outcomes in our study, which was consistent with previous reports[25]. It was reported that the most common cause of an unsuccessful outcome of retinal surgery following trauma was the development of proliferative vitreoretinopathy (PVR)[26]. Posttraumatic PVR was the final arbiter for anatomical and functional outcome after trauma.Compared with adult patients, children with retinal detachment tend to respond poorly to treatment due to a higher percentage of PVR and challenging operation in postoperative positioning.In this study, 35 recurrent retinal detachment patients were associated with severe PVR. Nevertheless, the risk factors for recurrent retinal detachment need to be further explored.
One of the primary limitations in our study is that PPV surgeries were not performed by the same surgeon, which will undoubtedly subject the patients to variation of surgical performance.
In summary, our study found age and injury types did not affect anatomical outcomes in pediatric ocular trauma. The treatment of vitrectomy for severe ocular trauma resulted in favorable anatomic outcomes, but visual improvement was not as good as to anatomic outcomes. Initial VA and recurrent retinal detachment are the independent prognostic indicators for unfavorable visual outcome of severe pediatric ocular trauma. Keep children out of reach of sharp objects and wear protective eyewear can reduce the incidence of ocular trauma.
ACKNOWLEDGEMENTS
The authors express their gratitude to Prof. Hua Yan, MD,Tianjin Medical University, China, for helpful suggestions for conducting the cases studied and critical review of the manuscript.
Foundations:Supported by National Natural Science Foundation of China (No.81770972); Military Scientific Grant of Army Medical University (No.2020HQZX18).
Conflicts of Interest: Qin ZX,None;HE Y,None;Xu YF,None;Yu T,None;Liu Y,None;Wu N,None.
 International Journal of Ophthalmology2021年9期
International Journal of Ophthalmology2021年9期
- International Journal of Ophthalmology的其它文章
- Five-year results of refractive outcomes and visionrelated quality of life after SMlLE for the correction of high myopia
- One-step viscoelastic agent technique for lCL V4c implantation for myopia
- miRNA-26b suppresses the TGF-β2-induced progression of HLE-B3 cells via the PI3K/Akt pathway
- Socio-economic disparity in visual impairment from cataract
- Disseminated hydatid disease in the orbit and central nervous system
- A ten years follow-up case of bilateral idiopathic multifocal retinal pigment epithelium detachments with rhegmatogenous retinal detachment and a literature review
