Five-year results of refractive outcomes and visionrelated quality of life after SMlLE for the correction of high myopia
Department of Ophthalmology, Daping Hospital, Army Medical University, Chongqing 400042, China
Abstract
● KEYWORDS: small incision lenticule extraction; high myopia; long-term follow-up
INTRODUCTION
Recently, femtosecond lasers have been widely used in ophthalmology, such as anterior capsulotomy with femtosecond laser in cataract surgery, femtosecond laserassisted keratoplasty, flap construction with femtosecond laser in femtosecond assisted laserin situkeratomileusis(FS-LASIK) and lens reation in the corneal stroma with femtosecond laser in small incision lenticule extraction(SMILE).
SMILE, a new type of corneal refractive surgery, uses a femtosecond laser to construct a lens in the corneal stroma and then separates and removes the lens through a small incision. Its flapless, minimally invasive features have a unique advantage over previous refractive surgery methods.In 2011, refractive outcomes of SMILE 6mo postoperatively were first reported by Sekundoet al[1]. SMILE largely preserves the corneal anterior surface and remodeled better in corneal biomechanical strength when compared to laserin situkeratomileusis (LASIK)[2]. Since then, SMILE is favoured by a large number of corneal refractive surgeons and myopia patients. Many short term studies of SMILE have confirmed the safety, effectiveness, predictability and stability of SMILE[3-8], but there have been few long-term observations about SMILE for correction of high myopia[9-11]. The majority of these studies focus on the objective measures for evaluation,yet often neglect the subjective experience or quality of life outcomes of the patient. Few publications compare quality of life following SMILE technique, and a paucity of the literature exists for any com-parative measures. To support evidencebased medicine, the present study reports visual, refractive outcomes and vision-related quality of life at 5y after SMILE correction.
SUBJECTS AND METHODS
Ethical ApprovalThe retrospective clinical study adhered to the tenets of the Declaration of Helsinki and was consistent with good clinical practices and local regulatory requirements.Written informed consent was obtained from all study subjects, and the protocols were reviewed and approved by the Institutional Review Board of the Army Medical University of China.
PatientsHigh myopia who have underwent SMILE for more than 5y were selected as SMILE group, and patients with high myopia who wore corrective spectacles for more than 5y were selected as the control group to evaluate the vision-related quality of life.
The inclusion criteria included age over 18y, corrected distance visual acuity (CDVA) of 20/25 or better, spherical equivalent (SE) over -6.00 diopters (D), myopic astigmatism up to -3.00 D, stable refraction for 2y, no use of any kind of contact lens within the previous 2wk. Patients with suspected keratoconus, severe dry eye syndrome, previous ocular trauma or ocular surgery, ocular diseases, or general diseases and patients who were pregnant or lactation were excluded. The calculated residual stromal bed thickness was greater than 280 μm preoperatively. Patients who underwent SMILE in the Department of Ophthalmology of Daping Hospital of Army Medical University (Former third military Medical University) from December, 2011 to May, 2013 received a phone invitation for an additional follow-up; 30 of 129 patients accepted this invitation. Thirty patients (60 eyes) with high myopia who underwent preoperative myopia examination in Daping Hospital from July to October 2019 were selected.The inclusion criteria included age 18-40y, CDVA of 20/25 or better, an SE over -6.00 D with astigmatism up to -3.00 D,stable refraction for 2y, use of corrective spectacles for more than 5y. Patients with systemic diseases, a history of ocular surgery or a history of ocular disease were excluded.
ProceduresAll patients received preoperative 0.3% tobramycin eye drops (S.A. Alcon-Couvreur N.V), four times daily for three days before SMILE. Due to the undercorrection of high myopia and the potential ectasia risk, -0.50 D sphere refraction was added to the preoperative manifest refraction for patients younger than 40y. Surgery in both eyes of the patients was performed by a single, experienced surgeon using the VisuMax femtosecond laser system (Zeiss, Germany) at power setting of 500 kHz, with a cumulative energy of 140 nJ. A cap thickness of 120 μm was planned to have a diameter of 6.0 mm with a 105 side cut in the superior region. The laser spot separation spot distance of the lenticule and sidecuts was 3 μm, 2.8 μm.After laser treatment, the upper and lower layers of the lens were bluntly separated, and then the lens was grasped with a pair of forceps and removed. Postoperatively, treatment was administered 0.5% levofloxacin (Santen Pharmaceuticals,Japan), 0.5% loteprednol etabonate ophthalmic suspension(Bausch & Lomb, USA) and artificial tears.
Postoperative Treatment and Follow-upThe postoperative follow-up for the SMILE included routine 1-day, 1-week,1-month, 3-month, 6-month, 1-year follow-ups and additional 5-year follow-up by phone. Routine examination included manifest refraction, noncontact tonometry, slit lamp examination, uncorrected distance visual acuity (UDVA)and CDVA. At 5-year follow-up, additional examination included the manifest refraction and ocular axial length (AL;IOLMaster 500, Carl Zeiss, Germany). The Chinese version of the National Eye Institute Visual Function Questionnaire-25(CHI-NEI-VFQ-25) was used to evaluate the vision-related quality of life between SMILE group and the control group.
Statistical AnalysisThe data were analyzed with SPSS 20.0(Inc., Chicago, IL, USA). The Kolmogorov-Smirnov test was used to test for normality. Statistical analysis of SE before and after surgery was performed with repeated measures tests, and multiple comparisons among means was performed using least significant difference (LSD) tests. Changes in ocular AL were analyzed with paired Student’sttest. The qualitative classification index analysis used a 4×2 column.Mann-Whitney tests were used to compare the composite and subscale scores of the CHI-NEI-VFQ-25. APvalue less than 0.05 was considered to indicate significance. Visual acuity and refraction analysis were performed according to the Standard Graphs for Reporting Refractive Surgery[12].
RESULTS
Fifteen men and fifteen women with sixty eyes were reviewed.The preoperative median age of the patients was 22.5y. The preoperative mean SE was -7.29±0.87 D (range -6.00 to -9.125 D).The preoperative eye characteristics are shown in Table 1.
EfficacyThe cumulative percentage of preoperative CDVA and postoperative UDVA is shown in Figure 1A. Forty-four eyes (73%) obtained UDVA of 20/20 or better and 58 eyes(97%) obtained UDVA of 20/25 or better at the 5-year followup. The efficacy index (postoperative UDVA/preoperative CDVA) was 1.09±0.18.
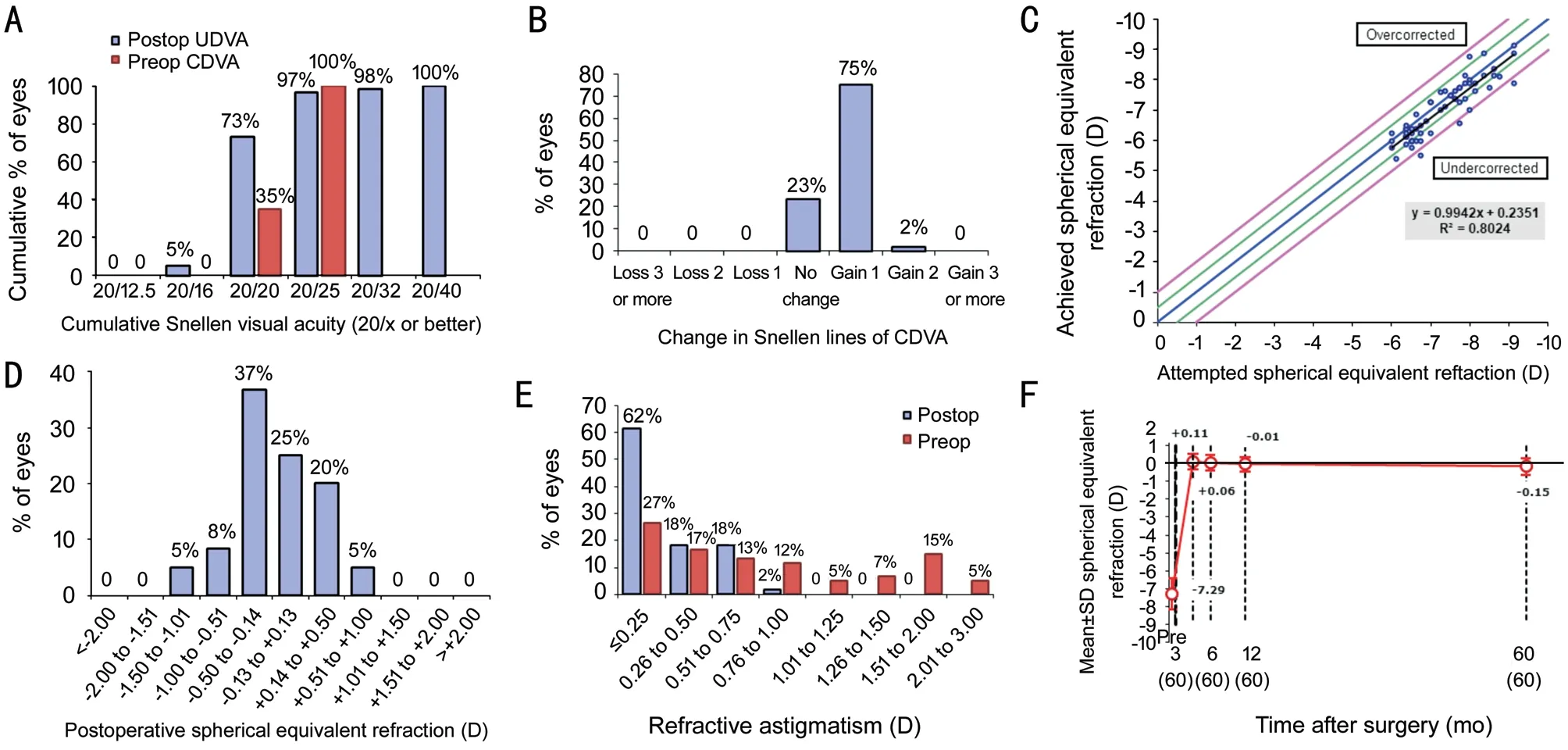
Figure 1 Refractive outcomes at 5y post surgery for 60 eyes with high myopia treated with SMILE A: Uncorrected distance visual acuity;B: Change in corrected distance visual acuity; C: Attempted vs achieved SE; D: SE refractive accuracy; E: Refractive astigmatism; F: Stability of SE refraction.
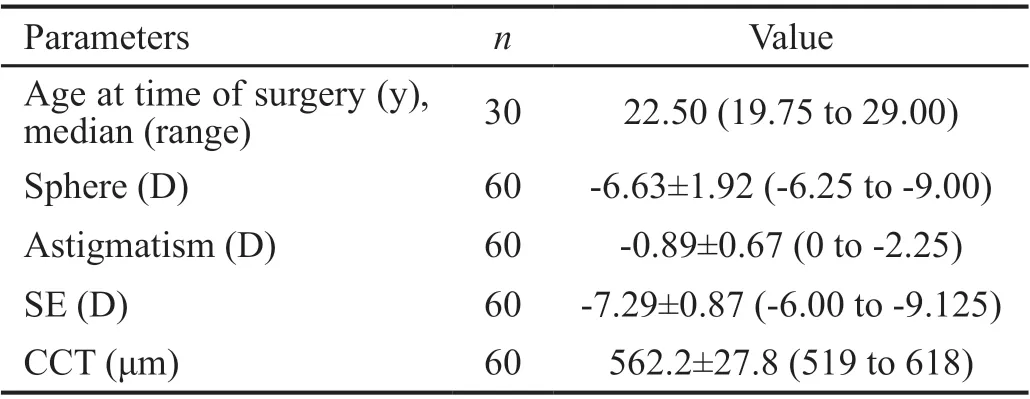
Table 1 Preoperative eye characteristics mean±SD (range)
SafetyThe change in CDVA lines are shown in Figure 1B. At the 5-year follow-up visit, there were no eyes with CDVA of one or more Snellen lines, and 14 eyes (23%) had no changes;45 eyes (75%) had gained one Snellen line, and 1 eye (2%)gained two Snellen lines. The safety index (postoperative CDVA/preoperative CDVA) was 1.19±0.12.
PredictabilityA scatterplot of the attempted versus achieved correction of 60 eyes after 5y is shown in Figure 1C. The preoperative mean SE was -7.29±0.87 D, the mean SE was-0.15±0.46 D at 5y postoperatively. A total of 82% of eyes were within ±0.50 D and 95% were within ±1.00 D of the attempted SE, respectively (Figure 1D). And a total of 80%had astigmatism <0.50 D (Figure 1E).
StabilityThe stability outcomes are shown in Figure 1F.The postoperative mean SE values at 3-month, 6-month,1-year, and 5-year were 0.11±0.44, 0.07±0.45, -0.02±0.41,and -0.15±0.46 D. SE LSD test results areP=0.228 for 3 to 6mo,P=0.096 for 3 to 6mo;P=0.000 for 3mo to 5y;P=0.002 for 6mo to 5y,P=0.015 for 1 to 5y. The refractive regression within 5y was 0.26 D. The overall mean difference between postoperative 3-month and postoperative 5-year of SE was significant (P<0.05). The changes in SE in 6 eyes (10%) were more than 0.5 D between 1-year and 5-year follow-up. There were 2 eyes that exhibited postoperative loss of UDVA of one or more Snellen lines.
Ocular Axial LengthThe ocular AL was 26.08±0.96 mm preoperatively and 26.01±0.94 mm at 5-year postoperatively.The preoperative and 5-year postoperative ocular ALs were not significant different (P=0.068, paired samplet-test).
Quality of Life EvaluationNo significant difference in general situation was found between the SMILE group and the control group (Table 2). There were 30 patients (non-driving,n=21) in the SMILE group and 30 patients (non-driving,n=17)in the control group. As shown in Table 3, the composite score of the SMILE group was higher than the control group(P<0.05); subscale scores of the CHI-NEI-VFQ-25 in general vision, distance activities, social functioning, mental health,role difficulties, dependency, color vision and peripheral vision were significantly different (P<0.05).
DISCUSSION
The present study reports long-term visual, refractive outcomes and vision-related quality of life obtained in 30 patients (60 eyes) with high myopia who underwent SMILE. We have analyzed the efficacy, safety, predictability, stability and visionrelated quality of life with a follow-up time of 5y.
In this study, the efficacy index of high myopia was 1.09±0.18.At 5y postoperatively, 44 eyes (73%) obtained a UDVA of 20/20 or better, and 58 eyes (97%) obtained a UDVA of 20/25 or better at the 5-year follow-up. Compared to preoperative CDVA, UDVA was worse in 2 eyes of 2 patients at 5-year postoperatively. The regression might have been the result of longterm growth of the AL in high myopia. Previous studieshave reported that the efficacy index of SMILE in cases of high myopia was found to be lower when compared to its efficacy in mild-to-moderate myopia. At 5-year visit, Ağcaet al[13]reported an efficacy index of mild-to-moderate myopia of 0.98±0.21 and found that 54 of the eyes (80%) achieved a postoperative UDVA of 20/20 or better. However, the efficacy index of high myopia has been found to be 0.89±0.26, with 37 of the eyes (30%) achieving a postoperative UDVA of 20/20 or better[10].
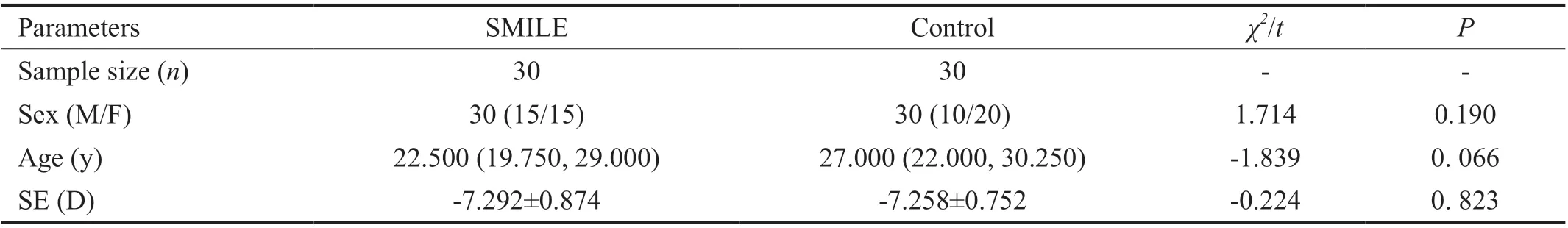
Table 2 General situation of the SMILE and control groups
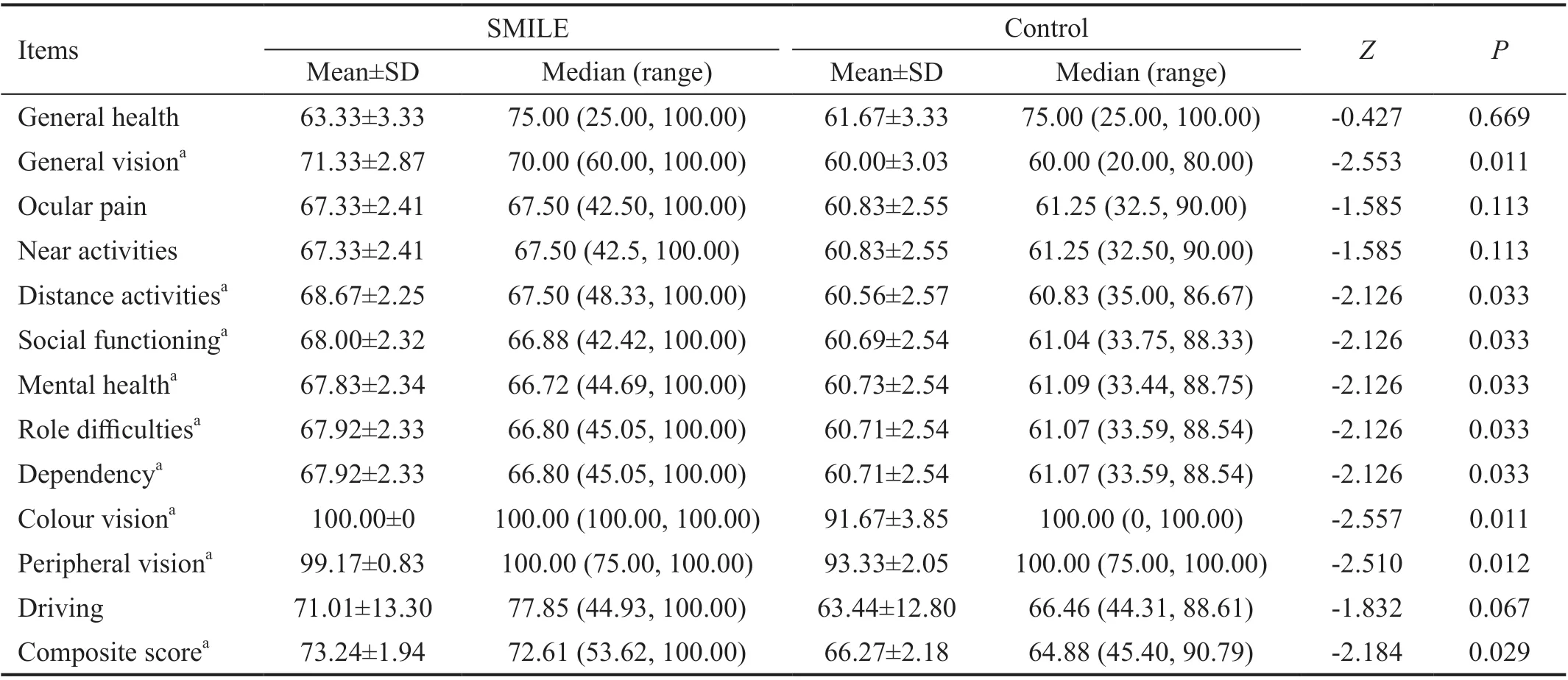
Table 3 Mann-Whitney test results for the CHI-NEI-VFQ-25 subscale and composite scores
At the 5-year follow-up visit, the safety index in this study was 1.19±0.12. There were no eyes with CDVA loss of one or more Snellen lines, and 14 eyes (23%) exhibited no changes.Forty-five eyes (75%) gained one Snellen line, and 1 eye (2%)gained two Snellen lines. Similar results have been reported in other studies. Pedersenet al[11]reported a safety index of 1.13 and found that 10 eyes (12%) had a CDVA less of one Snellen line, 35 eyes (40%) had no change, and 42 eyes (48%)gained one Snellen line or more. Ağcaet al[10]reported a safety index of 1.16±0.20 in high myopia at the 5-year follow-up visit; no eyes lost two or more lines of CDVA, 46% of eyes exhibited no changes; 27% of eyes gained one Snellen line and 16% of eyes gained two Snellen lines. On the one hand,one benefit of SMILE is that the postoperative CDVA is not lower than the preoperative CDVA. The other aspect is that the corneal biomechanical changes are small after surgery,and no corneal ectasia was found at the 5-year follow-up in this study. Unlike LASIK surgery, SMILE does not create corneal flaps and involves small incisions, thus preserving the integrity of the corneal tissue to the greatest extent possible.Therefore, it better preserves corneal biomechanics than LASIK. Randlemanet al[14]reports that the tension of the collagen fibers in the anterior 40% of the cornea stroma is almost 2 times higher than that of the collagen fibers in the lower 60% of the cornea stroma. Other studies have confirmed this view. Reinsteinet al[15]used a mathematical model to calculate the postoperative total stromal tensile strength(TTS), and SMILE led to the greatest strength; SMILE was followed by photorefractive keratectomy (PRK) and then LASIK. Increasing the thickness of the corneal cap increases the tension of the cornea in SMILE; in contrast, increasing the thickness of the corneal flap reduces the tension of the cornea in LASIK. A 160 μm cap thickness has less effect on corneal biomechanics than a 100 μm cap thickness in SMILE[16]. However, some studies have different conclusions.He and his colleagues compared small differences in rabbit corneal biomechanics resulting from the use of 100 μm versus 160 μm cap thicknesses in SMILE[17]. When the same corneal tissue is abled, SMILE and FS-LASIK cause no differences in corneal biomechanics[18]. Although SMILE surgery involves fewer changes in corneal biomechanics than FS-LASIK, some studies have reported corneal ectasia after SMILE and have shown that the procedure can affect the corneal biomechanics[19-22]. If a patient has conical or early keratoconus before surgery, he may develop significant corneal ectasia after SMILE surgery[20-22]. Corneal ectasia can occur after SMILE even in patients older than 40y and with normal preoperative topography[23-24]. These findings highlight the importance of thorough preoperative evaluation for possible keratoconus with changing corneal topography to avoid postoperative ectasia.
In terms of predictability, the results in patients with high myopia are good. In a study by Chansueet al[25]93% of the eyes were within ±0.50 D and 99% were within ±1.00 D at the 1-year follow-up. Yıldırımet al[26]reported 92% of high myopic eyes were within ±0.50 D and 100% of eyes were still within ±1.00 D at the 2-year follow-up. Hanet al[27]reported 89% of eyes were within ±0.50 D of the intended refractive target at the 4-year follow-up. In this study, 82% of eyes were within ±0.50 D of the intended refractive target at the 5-year follow-up, while 95% were within ±1.00 D.
In terms of long-term follow-up stability, high myopia presents slight undercorrection. In a study by Jinet al[28],the SEs in the high myopia group and the mild-to-moderate group were -0.20±0.37 and 0.01±0.19 D, respectively, at 3mo postoperatively. Ağcaet al[10,13]reported a 5-year followup study of mild-to-moderate myopia and high myopia. The refractive results were stable over long-term follow-up in mild-to-moderate myopia. The mean SEs in the first, third and fifth years after the operation were -0.09, -0.12,-0.13 D,respectively. However, there was regression of the refractive effect over extended follow-up in high myopia. The mean SEs in the first, third and fifth years after the operation were-0.26, -0.33, -0.43 D, respectively. In addition, in our research,the mean SEs at 3, 6mo, 1 and 5y after operation were +0.11,+0.06, -0.01 and -0.15 D, respectively. The mean regression between 3-month and 5-year visits was only 0.26 D, but the difference was significant. Blumet al[29]reported a regression of 0.48 D within a 5-year period. High myopia may be more prone to refractive regression after laser surgery than mild-tomoderate myopia. Whether we can adjust the initial correction value of high myopia patients to avoid undercorrection should be investigated.
The ultimate goal of refractive surgeries is to improve the quality of vision and life. Klokovaet al[30]found SMILE confered a better quality of life than pre-operation. There is a paucity in the literature regard-ing vision-related quality of life following refractive correction surgery, particularly long-term following SMILE. The National Eye Institute Visual Function Questionnaire-25 (NEI-VFQ-25) is a reliable questionnaire for evaluating vision-related quality of life. All items are from the NEI-VFQ-51, and the questionnaire included a base of 11 vision-targeted questions representing 11 vision-related constructs. Its reliability and Validity are similar to those observed for the 51-item version of the survey[31]. Chanet al[32]translated NEI-VFQ-25 into Chinese and showed that this questionnaire is a reliable and valid tool for assessing visionrelated quality of life in Chinese patients with eye diseases.In this study, the composite score of the NEI-VFQ-25 was significantly higher in the SMILE group than in the control group. Compared to those of the control group, the subscale scores of the SMILE group were elevated for general vision,distance activities, social functioning, mental health, role difficulties, dependency, colour vision and peripheral vision.Not only did the SMILE group get better distance vision, they also scored higher in vision-related behaviors. It shows that after SMILE operation, patients are mentally healthier and have more confidence in life. Belfortet al[33]evaluated patients who had received PRK and LASIK with the NEI-VFQ-25 and found that the patients showed improvements in quality of life and vision at three months after surgery.
There were some limitations of this study. The patients were invited for an additional 5-year examination. Selection bias may have occurred, because those with visual complaints may have been more willing to accept the invitation than those with no postoperative visual complaints. In our future work, the long-term changes in visual quality, higher-order aberrations,and corneal biomechanics and a large sample size of SMILE patients is needed.
In the present study, we have demonstrated that correcting high myopia with SMILE is safe, effective, and predictable in the long-term. Vision-related quality of life after SMILE is better in the SMILE group than in the control group who wore corrective spectacles.
ACKNOWLEDGEMENTS
Conflicts of Interest: Lang M,None;Cao KW,None;Liu T,None;Zhu Y,None;Ye J,None.
 International Journal of Ophthalmology2021年9期
International Journal of Ophthalmology2021年9期
- International Journal of Ophthalmology的其它文章
- One-step viscoelastic agent technique for lCL V4c implantation for myopia
- miRNA-26b suppresses the TGF-β2-induced progression of HLE-B3 cells via the PI3K/Akt pathway
- Pediatric ocular trauma with pars plana vitrectomy in Southwest of China: clinical characteristics and outcomes
- Socio-economic disparity in visual impairment from cataract
- Disseminated hydatid disease in the orbit and central nervous system
- A ten years follow-up case of bilateral idiopathic multifocal retinal pigment epithelium detachments with rhegmatogenous retinal detachment and a literature review
