Long-term outcomes of focal laser photocoagulation for the treatment of polypoidal choroidal vasculopathy
Sooyeon Choe, Hyun Goo Kang, Kyu Hyung Park, Christopher Seungkyu Lee,4, Se Joon Woo
1Department of Ophthalmology, Seoul National University College of Medicine, Seoul National University Hospital,Seoul 03080, Republic of Korea
2Department of Ophthalmology, Institute of Vision Research,Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul 06273, Republic of Korea
3Department of Ophthalmology, Seoul National University Bundang Hospital, Seongnam 13620, Republic of Korea
4Department of Ophthalmology, Institute of Vision Research,Severance Hospital, Yonsei University College of Medicine,Seoul 03722, Republic of Korea
Abstract
● KEYWORDS: long-term efficacy; polypoidal choroidal vasculopathy; focal laser photocoagulation
INTRODUCTION
Polypoidal choroidal vasculopathy (PCV) is a subtype of neovascular age-related macular degeneration characterized by a branching vascular network (BVN) and polypoidal dilatation of its termini, which is clinically shown as a reddish-orange polyp-like structure[1-2]. The prevalence of PCV varies from 20% to 60% in patients with neovascular age-related macular degeneration with ethnic predilection in East Asians[3].
Currently, PCV has various treatment options. Focal laser photocoagulation is the traditional treatment method where polyps identified by indocyanine green angiography (ICGA)are ablated. The early effect of focal laser photocoagulation was previously confirmed by optical coherence tomography angiography as well[4]. Verteporfin photodynamic therapy(PDT) and anti-vascular endothelial growth factor (VEGF)intravitreal injections emerged as effective treatment options for PCV. PDT monotherapy had some concerns over long-term visual outcome[5]. LAPTOP study reported that ranibizumab group had better visual acuity than PDT group at 5-year follow-up[6]. EVEREST-II and PLANET studies concluded that both anti-VEGF monotherapy and combination therapy with PDT show favorable visual outcomes at 1y[7-8]. Nowadays,two treatments are commonly accepted as initial therapies for PCV. However, a long-term observational study revealed that about 30% of eyes with PCV develop massive subretinal hemorrhage that significantly deteriorates vision during 10y of follow-ups[9]. Another recent report showed that focal laser photocoagulation yielded a very low long-term incidence rate(0) of massive submacular hemorrhage compared to anti-VEGF or PDT, which might have been related with the high rate of polyp regression post-laser treatment[10]. Previous reports showed cases of complete resolution of recalcitrant PCV after feeder vessel laser photocoagulation[11-12]. Thus,focal laser photocoagulation might have been undervalued and further assessment of its treatment efficacy may be needed.
In this study, we investigated the long-term effects and safety of focal laser photocoagulation treatment in eyes with PCV.
SUBJECTS AND METHODS
Ethical ApprovalThis study was approved by the Institutional Review Board of Seoul National University Bundang Hospital (IRB No.B-2003-601-111, Seongnam,Republic of Korea) and Yonsei University Severance Hospital(IRB No. 3-2019-0033, Seoul, Republic of Korea) adhered to the tenets of the Declaration of Helsinki.
SubjectsWe retrospectively reviewed the medical records of 13 eyes of 13 patients who were treated with focal photocoagulation for symptomatic PCV in Seoul National University Bundang Hospital and Gangnam Severance Hospital between May 2003 and February 2020. The patients were diagnosed with PCV by using the Japanese Study Group guidelines with ICGA[13]. We identified hyperfluorescent nodular polyps supplied by BVNviaICGA and located corresponding orange subretinal nodule on fundus photography. Patients with the presence of concomitant ocular diseases other than age related macular degeneration, such as glaucoma, diabetic retinopathy, retinal artery occlusion, and retinal vein occlusion were excluded from the study. Also,patients followed-up for less than 2y were not included.
Data CollectionThe baseline demographics data of the patients included age, sex, initial visual acuity, slit-lamp biomicroscopy, fundus examination, optical coherence tomography (Spectralis OCT; Heidelberg Engineering Inc,Heidelberg, Germany), and ICGA findings.
We identified the locations of polyps by ICGA as follows:subfoveal, juxtafoveal, or extrafoveal. We performed ICGA before and after focal laser photocoagulation to check the regression and recurrence of polyps. The regression of the polyp was identified 1mo after the focal laser photocoagulation and was defined as reduction of more than half of the initial polyp size. The recurrence of polyps was identified 6mo after the treatment. Additional ICGA was performed when the recurrence of polyps was suspicious. The complication of subretinal hemorrhage was assessed by its size. When the size of subretinal hemorrhage was between 1 optic disc diameter(DD) and 4 DD, it was defined as a significant subretinal hemorrhage. When the size of hemorrhage was more than 4 DD,it was defined as a massive subretinal hemorrhage[9].
The focal laser photocoagulation of polyps was conducted by experienced retina specialists (Woo SJ, Park KH, and Lee CS). The spot size, exposure time, and power of laser was determined by the specialists performing the procedure.The laser photocoagulation was performed starting from low power and duration (200 mW, 50-100ms) which were gradually increased until the reddish polypoidal lesion became white. Also, anti-VEGF agents (bevacizumab, ranibizumab,or aflibercept) were injected intravitreally when needed at the discretion of the clinician. Most cases were included when persistent subretinal fluid or hemorrhage was present. We analyzed the number of intravitreal injections per year before and after the focal laser photocoagulation treatment.
The measurement outcomes were the regression rate of polyps after focal laser photocoagulation, incidence of subretinal hemorrhage as complication, recurrence rate of polyp, changes in visual acuities, and the number of intravitreal injections per year during the follow-up period.
Statistical AnalysisStatistical analysis was performed using SPSS version 22.0 for Windows (SPSS, Inc, Chicago,IL, USA). Pairedt-test was used to compare visual acuities before and after the focal laser treatment. APvalue <0.05 was considered statistically significant. The scatter plot was produced using GraphPad Prism version 8.00 for Windows(GraphPad Software, San Diego California USA, www.graphpad.com).
RESULTS
The demographics, baseline characteristics, and clinical courses are depicted in Tables 1 and 2. Thirteen eyes of 13 patients were included in the study, and the mean age at the time of the laser treatment was 70.2±5.5y. Eight patients were male, and 5 patients were female. The locations included 3 juxtafoveal polyps and 10 extrafoveal polyps, with no subfoveal polyps.The mean follow-up period was 72.3±31.0mo (range, 25-118mo). Six eyes underwent intravitreal anti-VEGF injections in combination with focal laser photocoagulation.
Nine eyes (69.2%) showed regression of polyps after laser treatment. The mean regression period was 1.7±1.2mo (range,0.9-4mo). Of the 9 eyes with regressed polyps, 5 eyes (55.6%)recurred during the follow-up periods. The recurrence ofpolyps occurred at 12.8±18.9mo (range, 1.9-48mo). Typical cases showing the regression or recurrence of polyps are depicted in Figures 1 to 3. Only two eyes (15.4%) showed the complication of newly appeared mild subretinal hemorrhage 2.4 and 0.9mo after laser treatment, respectively.
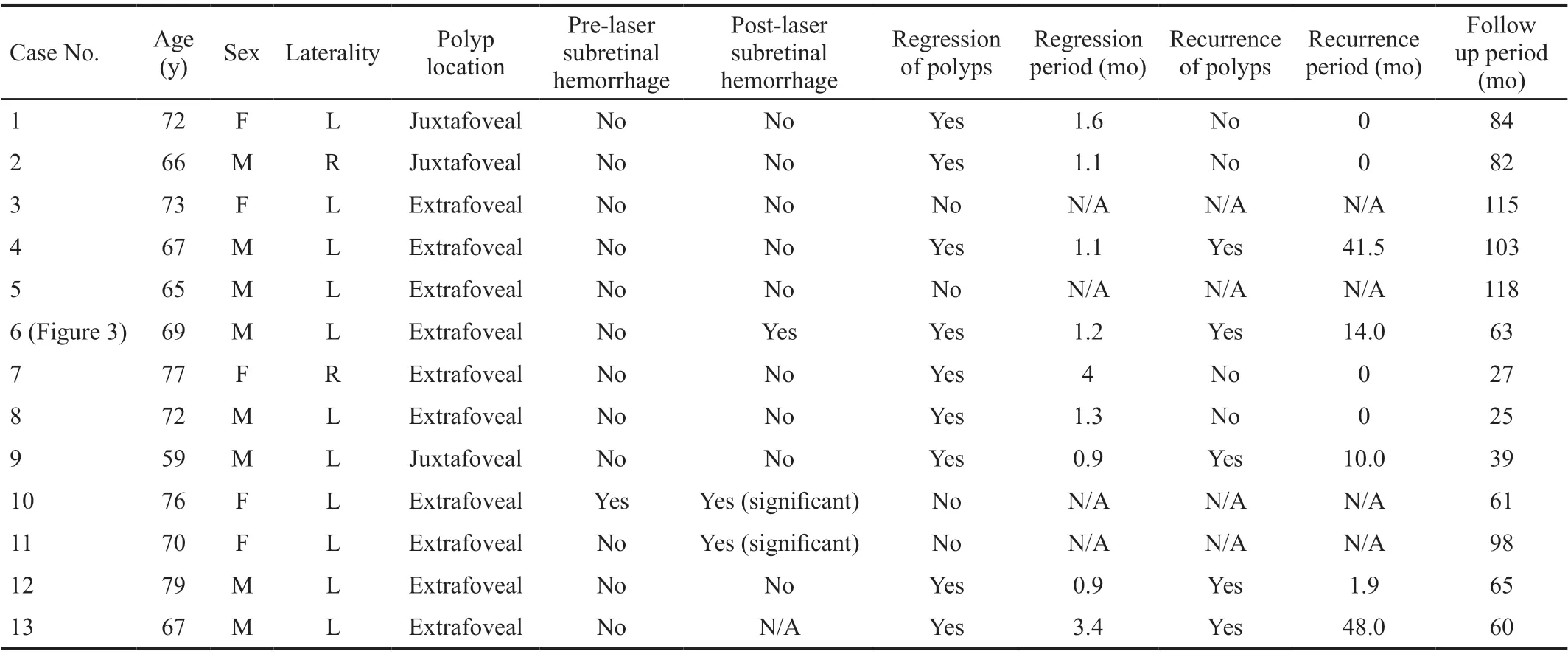
Table 1 Baseline characteristics and clinical courses of eyes with polypoidal choroidal vasculopathy
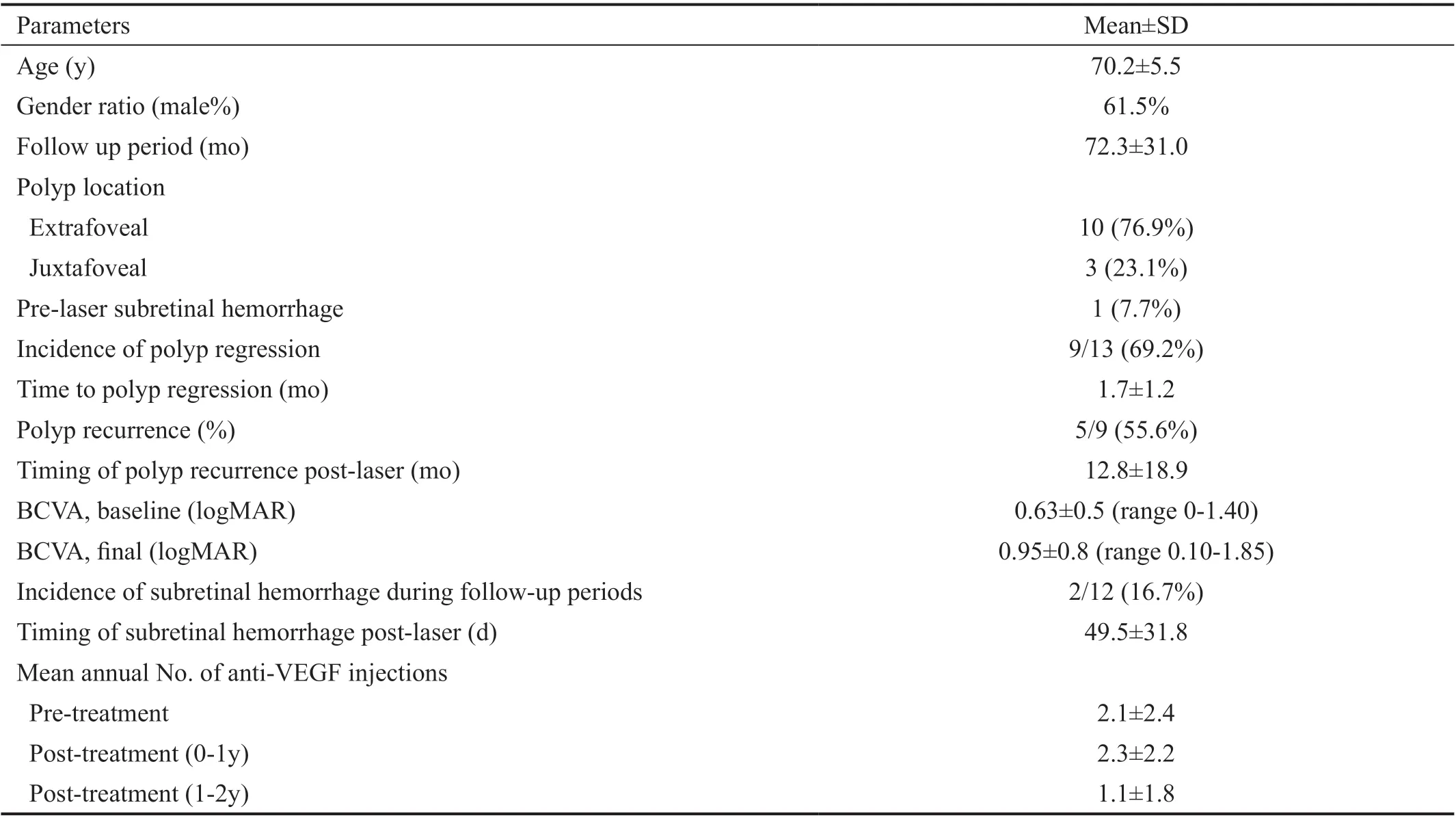
Table 2 Demographics of patients and clinical courses
The number of anti-VEGF injections per year was 2.1±2.4 before the treatment, 2.3±2.2 at the first year, and 1.1±1.8 at the second year. The mean visual acuity at baseline, 3mo, 1,2, 3y, and final visit were 0.63±0.5, 0.57±0.58, 0.73±0.70,0.67±0.57, 0.75±0.7, and 0.95±0.8 logMAR, respectively. The comparison of pre-laser and final visual acuities are depicted in a scatter plot (Figure 4). There were no significant differences between visual acuities before and after the treatment (allP>0.05).
DISCUSSION
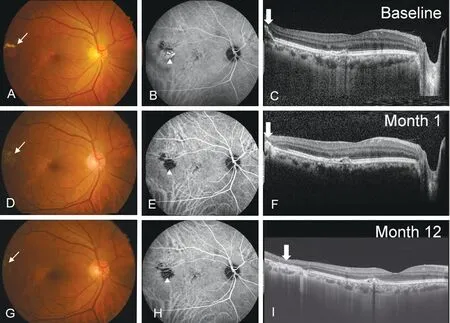
Figure 1 Images of a 63-year-old man with polypoidal choroidal vasculopathy in his right eye who was successfully treated with focal laser photocoagulation Top row images show a round orange-colored subretinal nodule with exudates nearby (A), corresponding to the nodular choroidal vascular lesion shown on indocyanine green angiography (B) and dome-like elevation of retinal pigment epithelial detachment on optical coherence tomography (C). Images in the middle (D-F) and bottom (G-I) rows demonstrate successful regression of the polyp at 1 and 12mo after the laser treatment, respectively.
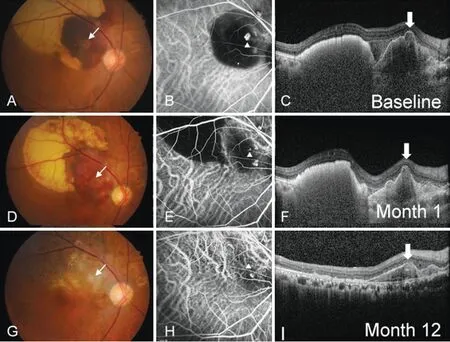
Figure 2 Images of a 76-year-old man with polypoidal choroidal vasculopathy in his right eye who was successfully treated with focal laser photocoagulation Images in the top row (A-C) show a round orange-colored subretinal nodule surrounded by a subretinal hemorrhage.Images in the middle (D-F) and bottom (G-I) rows demonstrate a decreased in polyp size 1 and 12mo after the laser treatment, respectively.
In this study, the effects and complications of focal laser photocoagulation were reviewed for a follow-up period of at least 2y (the average follow-up period was 6y). Of 13 eyes, about 70%of eyes had regressed polyps immediately after laser treatment while 56% showed recurrence 23.1mo post-treatment. During the follow-up period, no massive submacular hemorrhages developed and the visual acuities remained the same.Several previous reports have investigated the regression rate of polyps after focal laser treatment. Leeet al[14]demonstrated that in 28 eyes, 18 eyes (64.3%) showed complete resolution of polyps during a 12-month follow-up period. Lafautet al[15]reported that in 14 eyes, 10 eyes (71.4%) had regressed polyps 6mo after the treatment. Choet al[10]reported a polyp regression rate of 100% (7 eyes of 7 eyes) after focal laser treatment. In our study, 9 of 13 eyes (69.2%) showed resolution of polyps after a minimum follow-up period of 2y.These regression rates of polyps were relatively high compared to those after treatment with other modalities such as anti-VEGF injections or PDT. In the PLANET and EVERESTII studies, the regression rates were 38.9% after intravitreal injection of aflibercept and 34.7% after intravitreal injection of ranibizumab, respectively[7-8].
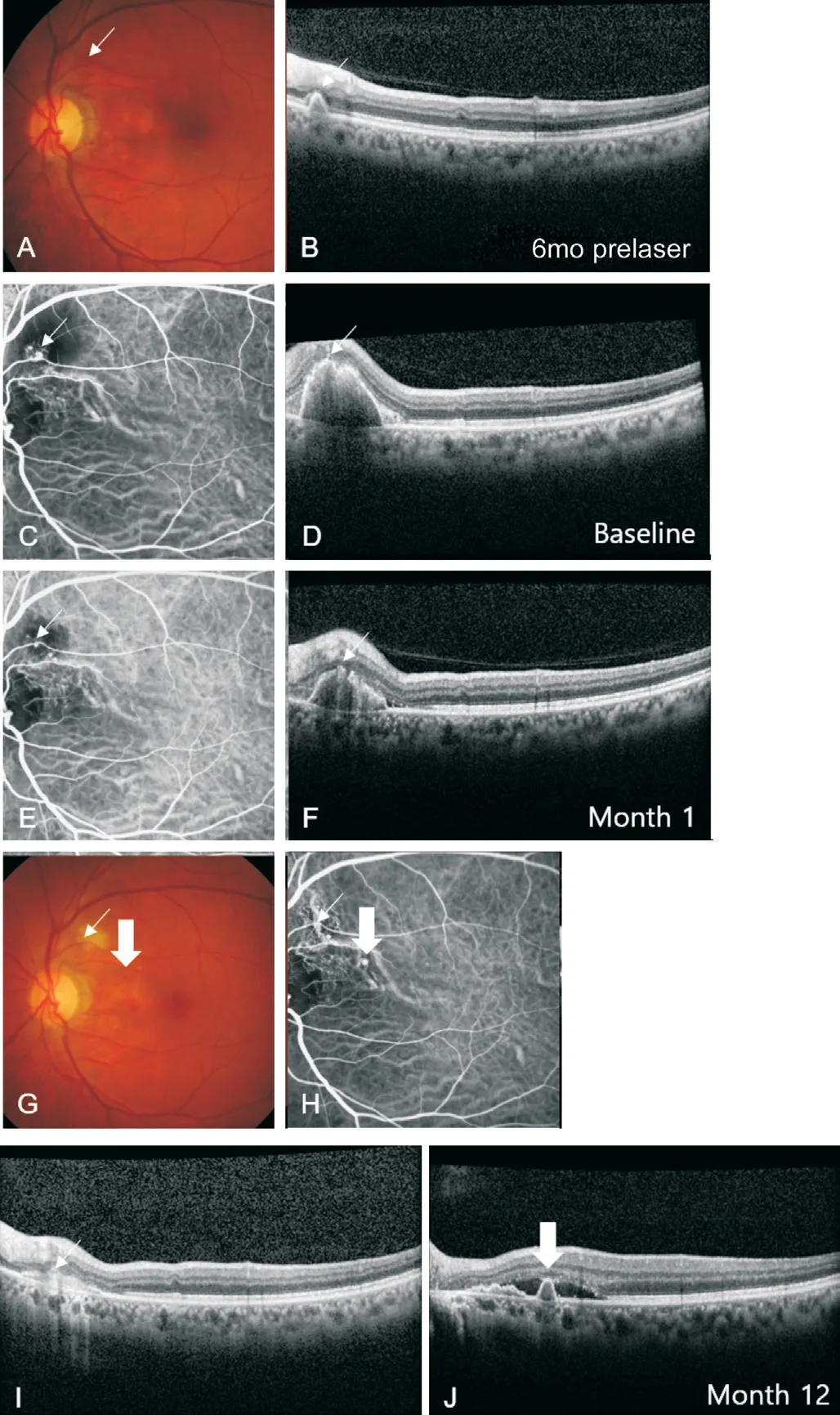
Figure 3 Images of a 69-year-old man with polypoidal choroidal vasculopathy in his left eye with recurred polyp Top row images were fundus photograph (A) and optical coherence tomography (B)at 6mo prior to a subretinal hemorrhage. Images in the second row(C, D) show the advent of subretinal hemorrhage as a complication of the polyp. The patient underwent focal laser treatment on the same day. Images in the third row (E, F) show a decrease in polyp size after 1mo. Images in the bottom row (G-J) were taken 1y after the focal laser treatment and show the recurrence of polyp from the branching vascular network.
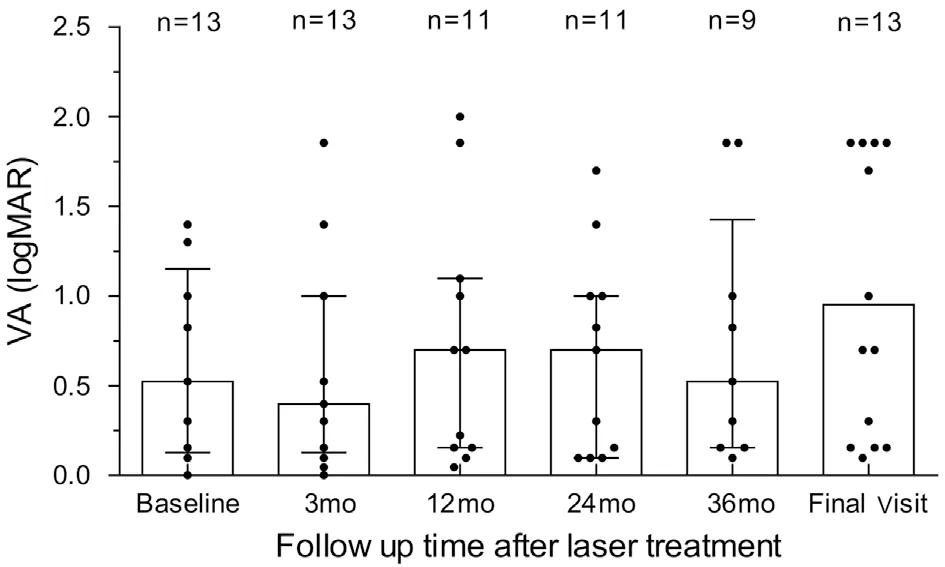
Figure 4 Scatter plot showing logMAR visual acuity (VA) There were no statistical differences between baseline VA and the VA at each follow-up period (P>0.05).
Our study had two eyes with late post-treatment mild subretinal hemorrhage. All of them had failed closure of polyps after focal laser treatment. This result is compatible with those of a former study by Choet al[10]. They demonstrated that the long-term massive submacular hemorrhage risk of PCV is higher in eyes with persistent polyps despite treatment,suggesting that treatment methods that can regress polyps are better for long-term visual preservation by avoiding massive submacular hemorrhages. The presumptive mechanism is that remaining active polyps may be subject to rupture, resulting in massive subretinal hemorrhage and irreversible damage to photoreceptors and retinal pigment epithelium.
There are concerns of polyp rupture after laser photocoagulation on polyps, but in this study, no massive subretinal hemorrhage was observed after laser treatment. Only mild subretinal hemorrhage not involving the fovea occurred in 2 of 13 eyes(15.4%). Taken together, the focal laser photocoagulation treatment can be safely performed in patients with PCV while substantially reducing the risk of future hemorrhages.In our previous study[10], additional anti-VEGF injections after PDT in eyes with PCV lowered the risk of massive submacular hemorrhage than PDT alone, which indicates that consistent anti-VEGF injections after focal laser treatment on PCV may reduce the long-term risk of polyp progression and massive submacular hemorrhage. This potential long-term effect of anti-VEGF agents needs to be confirmed by future studies.
Previous studies have reported a visual gain over 12mo after focal laser photocoagulations on eyes with PCV. Gemmy Cheunget al[16]reported that 28 of 33 eyes (84.9%) showed stable or improved vision for 1y. Leeet al[14]also reported that of 28 eyes, 75% showed stable or improved vision at 1y after laser treatment. Yuzawaet al[17]reported that about 90% of treated eyes showed visual gain or maintenance when polyps and network are treated by laser therapy concomitantly. In our study, although there was no significant visual gain after focal laser photocoagulation over 2 and 3y, the visual acuity was maintained during the long-term follow-up period of up to 10y post-laser treatment.
The strength of our study is the long-term follow-up period:the average was 72.3mo with a minimum follow-up period of 25mo. To the best of our knowledge, this is the first study to report the long-term results of focal laser photocoagulation on eyes with PCV. Also, we investigated the regression and recurrence rates, unlike previous reports that focused mostly on visual gains only[14,16-17]. The limitations of our study are the retrospective nature of the study and the relatively small size of the cohort. Also, focal laser treatment can be limited because it can only be applied on eyes with extrafoveal or juxtafoveal polyps not involving the papillomacular bundle. Therefore, an appropriate treatment modality should be chosen in eyes with PCV considering the location of polyps.
In conclusion, focal laser photocoagulation showed a high polyp regression rate without significant subretinal hemorrhage,while half of the eyes showed polyp recurrence more than 2y post-treatment. With a high rate of polyp regression and longterm visual maintenance without significant hemorrhages, focal laser photocoagulation could be considered for the treatment of eyes with PCV that have juxtafoveal or extrafoveal polyps.
ACKNOWLEDGEMENTS
Foundation:Supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT;No.2020R1F1A1072795).
Conflicts of Interest:Choe S,None;Kang HG,None;Park KH,None;Lee CS,None;Woo SJ,None.
 International Journal of Ophthalmology2021年9期
International Journal of Ophthalmology2021年9期
- International Journal of Ophthalmology的其它文章
- Five-year results of refractive outcomes and visionrelated quality of life after SMlLE for the correction of high myopia
- One-step viscoelastic agent technique for lCL V4c implantation for myopia
- miRNA-26b suppresses the TGF-β2-induced progression of HLE-B3 cells via the PI3K/Akt pathway
- Pediatric ocular trauma with pars plana vitrectomy in Southwest of China: clinical characteristics and outcomes
- Socio-economic disparity in visual impairment from cataract
- Disseminated hydatid disease in the orbit and central nervous system
