Associations of new-onset atrial fibrillation and severe visual impairment in type 2 diabetes:A multicenter nationwide study
Wisit Kaewput,Charat Thongprayoon,Ram Rangsin,Tarun Bathini,Michael A Mao,Wisit Cheungpasitporn
Wisit Kaewput,Ram Rangsin,Department of Military and Community Medicine,Phramongkutklao College of Medicine,Bangkok 10400,Thailand
Charat Thongprayoon,Wisit Cheungpasitporn,Division of Nephrology and Hypertension,Department of Medicine,Mayo Clinic,Rochester,MN 55905,United States
Tarun Bathini,Department of Internal Medicine,University of Arizona,Tucson,AZ 85721,United States
Michael A Mao,Department of Nephrology and Hypertension,Mayo Clinic,Jacksonville,FL 32224,United States
Abstract BACKGROUND Many studies have demonstrated an association between type 2 diabetes mellitus(T2DM) and atrial fibrillation (AF).However,the potential independent contributions of T2DM and AF to the prevalence of visual impairment have not been evaluated.AIM To determine whether such an association between T2DM and incident AF with visual impairment exists,and if so,the prevalence and magnitude of this association.METHODS We conducted a nationwide cross-sectional study based on the DM/HT study of the Medical Research Network of the Consortium of Thai Medical Schools.This study had evaluated adult T2DM patients from 831 public hospitals in Thailand in the year 2013.T2DM patients were categorized into two groups:patients without and with incident AF.T2DM patients without AF were selected as the reference group.The association between incident AF and visual impairment among T2DM patients was assessed using multivariate logistic regression.RESULTS A total of 27281 T2DM patients with available eye examination data were included in this analysis.The mean age was 60.7±10.5 years,and 31.2% were male.The incident AF was 0.2%.The prevalence of severe visual impairment in all T2DM patients,T2DM patients without AF,and T2DM patients with incident AF were 1.4%,1.4%,and 6.3%,respectively.T2DM patients with incident AF were associated with an increased OR of 3.89 (95%CI:1.17-13.38) for severe visual impairment compared with T2DM patients without AF.CONCLUSION T2DM patients with incident AF were independently associated with increased severe visual impairment.Therefore,early eye screening should be provided for these high-risk individuals.
Key Words:Type 2 diabetes mellitus;Atrial fibrillation;Visual impairment;Retinopathy;Blindness
INTRODUCTION
Type 2 diabetes mellitus (T2DM) is a common chronic disease worldwide[1].T2DM is associated with significant morbidity and mortality and has rapidly emerged as a global public health issue[2,3].Diabetic retinopathy and visual impairment are among these common and severe complications of T2DM.
Atrial fibrillation (AF) is the most common arrhythmia diagnosed in the world[4,5].Its prevalence is predicted to more than double by 2050[6].Previous studies found that AF may be relatively common in diabetic patients,and it should be regarded as a marker of increased adverse cardiovascular outcomes[7].In addition,diabetes has long been recognized as a risk factor for AF[8,9].The overlap of the pathophysiology of diabetes and AF concordantly increase the risk of thromboembolic events,and this has been well-established in the literature[10].The potential independent contributions of diabetes and AF to the prevalence of visual impairment,however,has not been evaluated.
This study was thus aimed to determine whether such an association between T2DM and incident AF with visual impairment exists,and if so,the prevalence and magnitude of this association.
MATERIALS AND METHODS
Study design and population
This was an analysis of the DM/HT dataset from 2013[11].This was a nationwide survey conducted annually in Thailand to evaluate the status of medical care in T2DM patients who visited the public hospitals of the Thai Ministry of Public Health and the clinics in the Thailand National Health Security Office’s program.The inclusion criteria of this DM/HT survey consisted of T2DM patients aged ≥ 35 years who received regular medical care in the targeted hospital for at least 12 mo.Patients who received care at primary care units outside Bangkok and university hospitals were excluded from this study.A two-stage stratified cluster sampling method was utilized to select a nationally and provincially representative sample of T2DM patients in Thailand.The first stage of sample collection consisted of the provinces that constituted 77 strata.The second stage of sample collection was the hospitals’ levels in each province,which were stratified into five strata according to the size of the hospital.These five strata were regional (>500 beds),provincial (200-500 beds),large community (80-120 beds),medium community (60 beds),and small community (10-30 beds) hospitals.All regional (n=25) and provincial (n=70) hospitals were enrolled,but only 456 (62% out of 736) community hospitals were included.Of 456 community hospitals,10%,20%,and 70% were large,medium,and small community hospitals,respectively.
All patients were recruited from the outpatient clinic.Written informed consent was obtained from patients before enrolment.This study was approved by both the Institutional Review Board of the Royal Thai Army Medical Department and the Ethical Review Committee for Research in Human Subjects of the Ministry of Public Health of Thailand,due to the bureaucratic system regulations in Thailand.Well-trained research nurses reviewed medical records and collected data into a case record form.Data entry into this form was then transferred to the central data management of the Medical Research Network of the Consortium of Thai Medical Schools.This data management team adjudicated the process of data collection to ensure it was compiled according to the study protocol.This team was also responsible for inquiries to study sites to verify data.Site monitoring was randomly performed in approximately 10% of study sites.This study was conducted by the Strengthening the Reporting of Observational Studies in Epidemiology[12].
Data collection
Clinical characteristics,demographic information,medication,and laboratory data were collected using a manual data retrieval from the medical record as described above.The laboratory data included results from 12 mo prior to the consent process.Incident AF was identified by ICD10 code I48,and subsequently verified by medical record review during the 12 mo of the study period.This verification of AF consisted of electrocardiogram (ECG).The date of first ECG documenting the presence of AF was considered the onset of atrial fibrillation.We exclude patients who had prior history of AF before the start date.Estimated glomerular filtration rate (eGFR) was estimated based on age,sex,race,and most recent creatinine with calculationviathe Chronic Kidney Disease Epidemiology Collaboration equation[13].CHA2DS2VASc score was calculated by using clinical data from the medical record.Primary outcome was diagnosis of severe visual impairment within 12 mo of data collection.Binocular visual acuity (VA) was examined using a semi-qualitative assessment and documented by physicians.Severe visual impairment was based on the worst VA exam of both eyes that consisted of “counting fingers,” “hand motions,” “projection of light,” “perception of light,” and “no light perception.”
Statistical analysis
Continuous variables were presented as mean±SD.Categorical variables were presented as count with percentage.Clinical characteristics and outcomes were compared among the different groups using the independent t-test for continuous variables,and Chi-squared test,and Fisher’s exact test for categorical variables.T2DM patients were categorized into two groups:(1) T2DM patients without AF;and (2)T2DM patients with incident AF.T2DM patients without AF were selected as the reference group.Univariate and then multivariate logistic regression analysis,adjusting for priori-defined variables,were performed to assess the independent association between AF onset and severe visual impairment.Odds ratio (OR) with 95%confidence interval (CI) was reported.The adjusted variables consisted of age,sex,duration of T2DM,body mass index (BMI),smoking,comorbidities,complications,and medications.Comorbidities and complications were hypertension,ischemic heart disease,cerebrovascular disease,diabetic retinopathy,eGFR,and CHA2DS2VASc score.Medications were insulin,antiplatelets,and anticoagulants.APvalue<0.05 was considered statistically significant.All statistical analyses were performed using SPSS version 22 (SPSS,Inc.,Chicago,IL,United States).
RESULTS
Clinical characteristics
A total of 27339 adult T2DM patients with eye examination data from 831 public hospitals in Thailand were included in this analysis.Clinical characteristics are summarized in Table 1.The mean age was 60.7±10.5 years,and 31.2% were male.The mean diabetic duration was 7.1±4.8 years.The mean BMI was 25.6±4.5 kg/m2.The mean eGFR was 66.9±25.9 mL/min per 1.73 m2.The mean CHA2DS2VASc was 2.9±1.0.The prevalence of T2DM with incident AF was 0.2% (n=48).
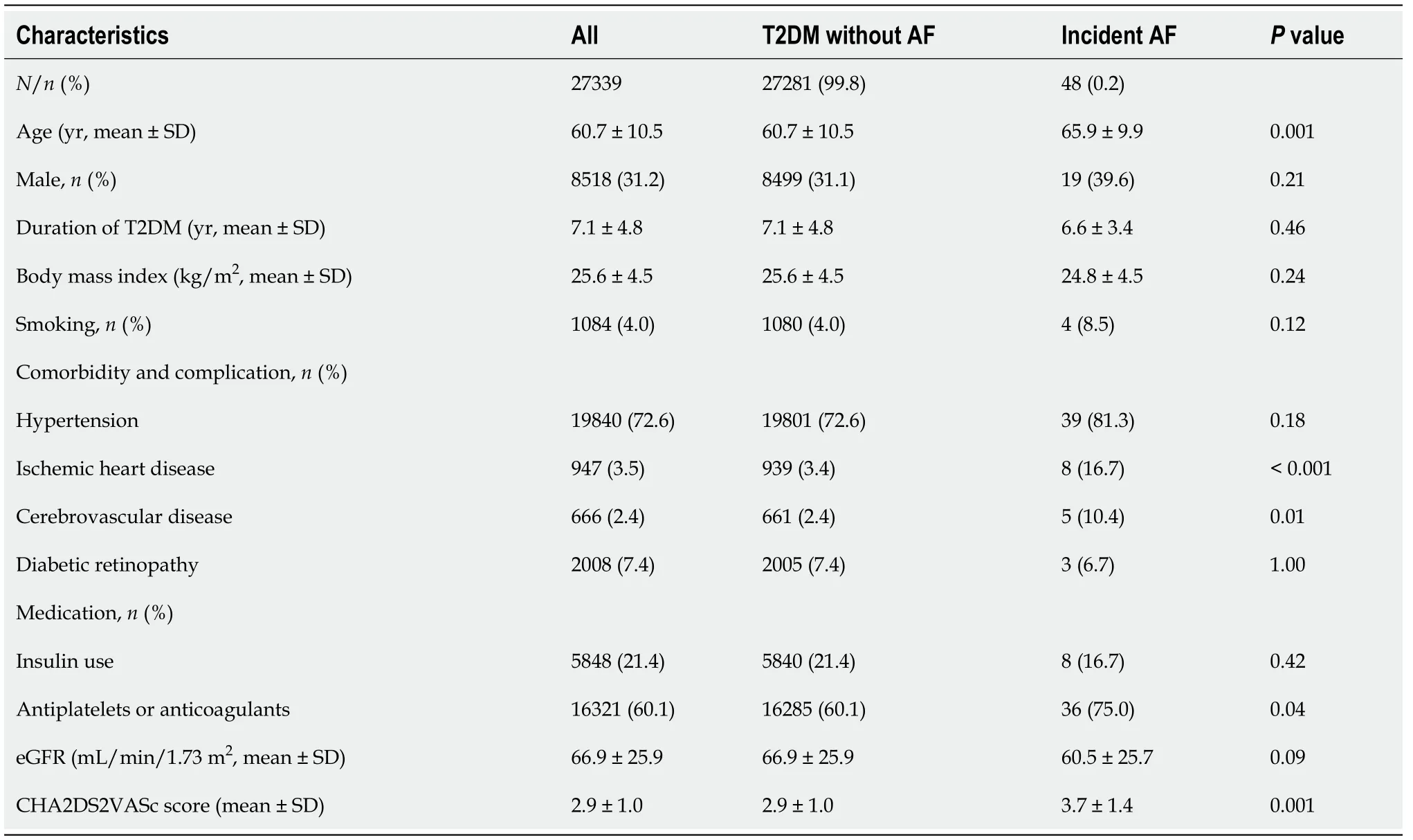
Table 1 Baseline characteristics
Association between of AF and severe visual impairment in T2DM
The prevalence of severe visual impairment in all T2DM was 1.4%.Severe visual impairment was documented in 1.4% of patients without AF and in 6.3% of patients with incident AF (Table 2).
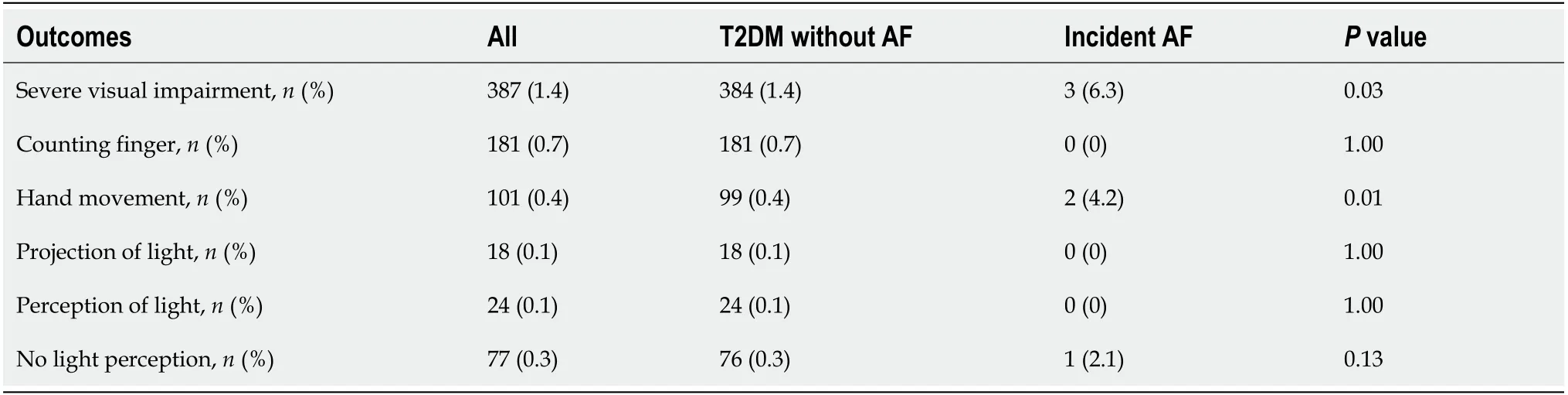
Table 2 Prevalence of severe visual impairments stratified by presence of incident atrial fibrillation in type 2 diabetes mellitus patients
In adjusted analysis,incident AF was associated with an increased OR of 3.89(95%CI:1.17-13.38) for severe visual impairment (Table 3).

Table 3 Association of incident atrial fibrillation and severe visual impairment in type 2 diabetes mellitus patients after multivariate logistic regression analysis
DISCUSSION
An analysis of the baseline patient characteristics showed that T2DM with incident AF was associated with older age.Moreover,T2DM patients with AF had a higher prevalence of ischemic heart disease,cerebrovascular disease,and increased use of antiplatelet medications compared to patients without AF.These findings are consistent with a study performed by Nicholset al[14] and Benjaminet al[9],where AF was similarly found to be correlated with older age and ischemic heart disease.However,in their study,history of smoking was not associated with AF in T2DM patients.It is not surprisingly to find these associations,as it could be hypothesized that since these clinical characteristics are established risk factors for development of any cardiovascular diseases,it follows that they could also precipitate AF development in T2DM patients.
Prevalence of severe visual impairment in T2DM patients
The prevalence of severe visual impairment in all T2DM patients,T2DM patients without AF,and T2DM patients with incident AF were 1.4%,1.4%,and 6.3%,respectively.According to previous studies from the United Kingdom[15] and the United States[3],the overall prevalence of visual impairment in T2DM ranges between 0.75% to 3.80%.Etiologies of visual impairment in T2DM patients include retinopathy of any type (particularly diabetic retinopathy),glaucoma,and cataracts[16].A recent meta-analysis found that diabetes was associated with an increased incidence of glaucoma[3].
Association between AF and severe visual impairment
This study showed that AF is independently associated with severe visual impairment in adult T2DM patients.No prior studies have investigated this association.The pathogenesis of poor vision in recently diagnosed AF may be multifactorial,including retinal emboli[17,18].Retinal artery occlusion (RAO)[19] and retinal vein occlusion(RVO)[20] are increasingly common in older subjects.As age increases,the risk of AF also substantially increases.Previous studies from Hayrehet al[21] and Yenet al[19]draw a potential pathophysiologic association,as they have reported that patients with AF are at increased risk of developing RAO.A study by Christiansenet al[22] also found that RAO was associated with an increased risk of incident AF.O'Mahoneyet al[23] and Christiansenet al[24] reported that RVO might be an important cause of blindness in populations with high atherosclerotic risk.These conditions share the same traditional risk factors as for cardiovascular diseases,possibly due to shared pathophysiologic mechanisms.
Conditions like anterior ischemic optic neuropathy (AION)[25],age-related macular degeneration (AMD)[26,27],and cataracts may all be other potential etiologies for visual impairment in this population[28].Callizoet al[25] found that AION may cause blindness in patients with AF.Clemonset al[26] and Topouziset al[27] suggest an increased risk of AMD with diabetes mellitus.In a cohort study by Hahnet al[29],it was found that diabetic retinopathy might increase the risk of both dry and wet AMD.These studies support a potential similar pathophysiologic mechanism between diabetic retinopathy and AMD.Optimal diabetic control may reduce the development of AMD.Kleinet al[28] found that T2DM is associated with an increased incidence and progression of cataracts,which may be worsened by suboptimal glycemic control.In summary,cardiovascular disease and its associated risk factors have an adverse effect on the incidence of age-related cataracts.These risk factors need to be promptly investigated in order to reduce ophthalmologic complications through early interventions.
Strengths
Our study consisted of a large-size sample from a multicenter and nationwide population-based design that provided detailed eye examination information while accounting for potential confounders in order to allow an adequate estimate of severe visual impairment burden in T2DM patients with AF.Our analysis of the association between eGFR and DR utilized a multiple logistic regression model that accounted for several possible confounders,including age,sex,duration of T2DM,body mass index(BMI),smoking,other comorbidities,and medications.Comorbidities included hypertension,ischemic heart disease,cerebrovascular disease,and diabetic retinopathy.Medications that were adjusted for included insulin and antiplatelet medication.Lastly,visual impairment severity was measured using a semi- qualitative clinical scale composed of bedside testing items,which is an easy test to perform in the community setting.
Limitations
This study had several limitations.First,we identified AF using ICD 10 codes and then subsequently confirmed by medical record review for documented ECGs.As ECGs were usually performed when clinically indicated rather than universally,our study may have underdiagnosed asymptomatic AF.This may explain the low prevalence of AF in our study compared to previous reports[30-33].Future studies utilizing advanced cardiac monitoring technology such as signal-averaged ECGs and Holter monitors would more accurately capture total prevalence of AF.In addition,AF could be paroxysmal,and periodic ECGs may not have detected these paroxysmal AF episodes.Thus,future studies are needed to better assess the associations of visual impairment with asymptomatic AF and AF subtypes among T2DM patients.Second,our study was cross-sectional in nature.A longitudinal study in the future may provide further details on the etiology of visual impairments in order to better confirm the association and elucidate the pathophysiology of new-onset AF and poor vision in T2DM patients.Third,information on prior eye surgeries,such as vitrectomy due to retinal hemorrhage,was scarce.These patients may have suffered a prior visual impairment rather than incorrectly associated with incident AF.Fourth,information on the etiology of visual impairment other than diabetic retinopathy was not available.Finally,although we performed multivariate analysis for further adjustment of potential confounders including CHA2DS2-VASC and anticoagulation,we did not have information on the specific type of AF,type of anticoagulation therapy used,international normalized ratio (INR) levels,previous AF medications for rate control,and outcomes of AF treatment.These are potential confounding factors that were unaccounted for.Therefore,this study was unable to determine the association between optimally treated AF and visual impairment in T2DM patients.
Implications
Our study found a nearly three-fold higher prevalence of poor vision in T2DM patients with incident AF.Several conditions such as glaucoma,cataracts,and retinopathy are potentially reversible causes of vision impairment,especially if treated early.It may be useful to screen for visual impairment and its etiologies in T2DM patients with recent-onset AF (less than 1-year).The results of our study could encourage public health initiatives to institute early eye screening in these high-risk individuals in order to prevent vision impairment.Further studies are needed to elucidate whether these interventions would translate into improved clinical outcomes.
CONCLUSION
The prevalence of severe visual impairment in T2DM patients with incident AF was nearly three times higher than the prevalence of impaired vision in all T2DM patients.Moreover,T2DM patients with incident AF were independently associated with severe visual impairment.Early eye screening should be performed in these high-risk individuals as it may provide an earlier diagnosis,allowing for prevention and treatment of potentially reversible causes of vision impairment.
ARTICLE HIGHLIGHTS
Research background
Previous studies have shown an association between type 2 diabetes mellitus (T2DM)and atrial fibrillation (AF).However,the independent contributions of T2DM and AF on the prevalence of visual impairment have not been evaluated.
Research motivation
Earlier studies have demonstrated that AF is relatively common in diabetic patients,and it should be regarded as a marker for adverse cardiovascular outcomes in T2DM.
Research objectives
To investigate whether an association between T2DM and incident AF with visual impairment exists,and if so,the prevalence and magnitude of this association.
Research methods
This study evaluated adult T2DM patients from 831 public hospitals in Thailand in the year 2013.The association between T2DM with incident AF and visual impairment were assessed using multivariate logistic regression.
Research results
A total of 27281 T2DM patients with available eye examination data were included in this analysis.The prevalence of incident AF in T2DM patients was 0.2%.The prevalence of severe visual impairment in all T2DM patients,T2DM patients without AF,and T2DM patients with incident AF were 1.4%,1.4%,and 6.3%,respectively.T2DM patients with incident AF were associated with an increased OR of 3.89 (95%CI:1.17-13.38) for severe visual impairment compared to those without AF.
Research conclusions
T2DM patients with incident AF were independently associated with severe visual impairment.Early eye screening should be provided for these high-risk individuals.
Research perspectives
Overlapping diabetes and AF leads to an increased risk of thromboembolic events.However,the independent contribution of T2DM and AF to the prevalence of visual impairments has not been evaluated.Therefore,it may be useful to screen for visual impairment and its etiologies in T2DM patients with incident AF.
ACKNOWLEDGEMENTS
The authors wish to thank the Medical Research Network of the Consortium of Thai Medical Schools (MedResNet) Thailand,which granted access to the diabetes and hypertension dataset in the DAMUS website (http://www.damus.in.th/damus/index.php).
 World Journal of Cardiology2021年8期
World Journal of Cardiology2021年8期
- World Journal of Cardiology的其它文章
- ISCHEMIA trial:How to apply the results to clinical practice
- Shortened dual antiplatelet therapy in contemporary percutaneous coronary intervention era
- Multimodality imaging in the diagnosis and management of prosthetic valve endocarditis:A contemporary narrative review
- Potential role of an athlete-focused echocardiogram in sports eligibility
- In-depth review of cardiopulmonary support in COVID-19 patients with heart failure
- Surgical strategies for severely atherosclerotic (porcelain) aorta during coronary artery bypass grafting
