Acute bilateral macular necrosis in a young healthy patient without herpetic virus infection: sequential multimodal imaging features
Xue-Feng Feng, Hai-Ping Li
Ophthalmology Department, Beijing Key Laboratory of Restoration of Damaged Ocular Nerve, Peking University Third Hospital, Beijing 100191, China
Dear Editor,
I am Dr. Xue-Feng Feng from the Ophthalmology Department, Peking University Third Hospital, Beijing,China. I am writing to present an unusual case of acute bilateral macular necrosis without peripheral retinal involvement in a young healthy patient.
Necrotizing retinopathies, a group of uncommon posterior segment complications of herpetic viral etiology caused by members of theHerpesviridaefamily, include acute retinal necrosis (ARN), progressive outer retinal necrosis (PORN),and cytomegaloviral retinitis within the immunocompromised patient population[1-2]. Macular necrosis is involved in the late stages of ARN; only a few cases of early-stage central macular necrosis have been reported, which all involved the subsequent development of peripheral lesions[3-5]. In this report, we present a patient who developed devastating acute bilateral macular necrosis but did not present with herpetic virus infection or an immunocompromising disease, especially with no peripheral retinal involvement. Sequential fundus features on multimodal imaging are also presented.
A healthy 25-year-old man presented with 4d of painless vision decreasing in the left eye with no past medical history.The best corrected visual acuity was 0.9 in the right eye and 0.02 in the left eye. The intraocular pressure was 16 mm Hg in the right eye and 12 mm Hg in the left eye. Examination of the right eye was normal. Slit-lamp examination of the left eye showed 1+ anterior chamber cells. Funduscopy of the left eye revealed mild vitreous opacification, whitish macular necrosis in a geographical pattern, with a few scattered dot retinal hemorrhages, but without any other peripheral retinal findings. Fundus fluorescein angiography (FFA) of the left eye demonstrated slight vasculitis without obstruction or infarction of the retinal capillaries. Spectral-domain optical coherence tomography (SD-OCT; Heidelberg Engineering,Heidelberg, Germany) showed severe macular edema with significant destruction of the macular layers (Figure 1). Α week later, similar but less severe lesions developed in the right eye. The vision decreased to 0.1 in the right eye and finger counting (FC) in the left eye (Figure 2A-2D). Hematological work-up revealed negativity for human immunodeficiency virus, syphilis, cytomegalovirus (CMV), herpes simplex virus(HSV), andToxoplasmaimmunoglobulin (Ig)M and IgG. His C-reactive protein level and erythrocyte sedimentation rate were also within normal ranges. The interferon‐γ release assay result was negative. Cell counts and blood chemistry results were all within normal ranges.
Early-stage ARN was suspected, but subsequent polymerase chain reaction (PCR) analysis of the aqueous humor and vitreous revealed negativity for HSV-1, HSV-2, varicella zoster virus, and CMV.

Figure 1 Fundus images at presentation A: Color fundus photography of the left eye showed whitening necrosis of the macula;B: Fundus fluorescein angiography of the left eye revealed mild vasculitis with no vascular occlusion or infarction; C: SD-OCT image of the left eye showed high macular edema with destruction of the retinal layers; D, E: Color fundus photography and SD-OCT image of the right eye showed a normal macula.
Treatment was initiated with a retro-bulb injection of triamcinolone acetonide (20 mg) and oral prednisolone(60 mg/d). Two weeks after initiating treatment, macular whitish edema was reduced, retinal hemorrhages were mostly absorbed, and SD-OCT showed a significant loss in the macular architecture along with reduced macular edema. Four weeks later, the macular edema had further reduced, and the visual acuity was 0.06 and 0.03, respectively; however, the macular thickness had reduced to a highly reflective line in the left eye, and loss of the outer retinal layers in the right eye were noted on SD-OCT. Oral prednisolone was tapered to cessation 8wk later. Three months later, the visual acuity increased to 0.1 in the right eye and 0.06 in the left eye; the fundus showed that the macular color had recovered to nearly normal, but SD-OCT showed thinning of the inner retinal layers and loss of the outer retinal layers in the right eye, and only a line was remaining in the macular area in the left eye (Figure 2E-2H). Six months later, no changes were noted in his vision. No peripheral retinal lesions developed throughout the disease course in either eye.The differential diagnoses of central macular necrosis are ARN, PORN, and cytomegaloviral retinitis. Clinically, ARN appears as full-thickness, opaque, yellow-white, necrotic lesions initially outside of the vascular arcades with significant intraocular inflammation. The hallmark sign of PORN is multifocal, opaque, yellow-white necrotic lesions manifesting initially either in the periphery or posterior pole. ARN and PORN are observed in individuals often diagnosed with compromised immune system or herpetic virus infection.Cytomegaloviral retinitis is the result of systemic reactivation of latent infection and is often asymptomatic. Clinical presentation involves pale, full-thickness retinal lesions that initially spread along the vasculature, with prominent focal hemorrhaging[1]. Our patient was healthy and had no history or signs of immunocompromised diseases, as supported by the negative laboratory workup results. The efficacy of prednisolone with no antiviral therapy further suggested that he had not contracted a viral infection. Ischemic retinal vasculitis, either idiopathic or secondary to systemic diseases such as Behçet’s disease, sarcoidosis, tuberculosis, multiple sclerosis, and systemic lupus erythematosus, were ruled out, as the patient had neither retinal vascular obstruction or infarction on FFA nor systemic findings. It is unique that our patient had bilateral macular necrosis, and the lesions were localized only in the macular area without any peripheral involvement.Macular necrosis involves the full thickness of the retina,which is similar to the findings in patients with herpetic virus infection[1,5]. The macula is devastatingly damaged as revealed on SD-OCT and leads to very poor vision. Further observation and follow-up of this patient are needed to determine the underlying causes of this case of severe bilateral acute macular necrosis.
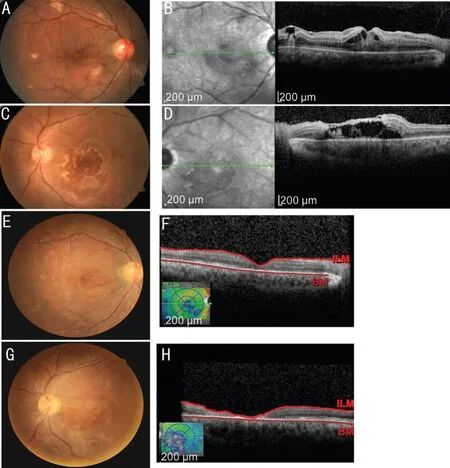
Figure 2 Fundus images at one week (A-D) and 3mo (E-H)after initial presentation A: Fundus photography of the right eye showed whitish macular lesions; B: SD-OCT image of the right eye showed macular edema; C: Fundus photograph of the left eye showed regression of macular edema; D: SD-OCT image of the left eye showed reduced macular edema along with a loss of macular structure; E, F: Color fundus photograph and SD-OCT image of the right eye showed that the macular necrosis had resolved and loss of the outer retinal layers and thinning of the inner retinal layers; G, H:Color fundus photograph and SD-OCT image of the left eye showed that the macular edema had resolved, but only a line remained in the necrotic macular area. SD-OCT. Spectral-domain optical coherence tomography.
ACKNOWLEDGEMENTS
Conflicts of Interest:Feng XF,None;Li HP,None.
 International Journal of Ophthalmology2021年8期
International Journal of Ophthalmology2021年8期
- International Journal of Ophthalmology的其它文章
- Macular density alterations in myopic choroidal neovascularization and the effect of anti-VEGF on it
- ldentification and validation of tumor microenvironmentrelated lncRNA prognostic signature for uveal melanoma
- Factors associated with axial length elongation in high myopia in adults
- Visualizing the intellectual structure and recent research trends of diabetic retinopathy
- Therapeutic effect of Keap1-Nrf2-ARE pathway-related drugs on age-related eye diseases through anti-oxidative stress
- Newly-found functions of metformin for the prevention and treatment of age-related macular degeneration
