Scar sarcoidosis with systemic involvement after blepharoplasty
Su Youn Suh, Jung Hyo Ahn
Department of Ophthalmology, Research Institute for Convergence of Biomedical Science and Technology, Pusan National University Yangsan Hospital, Pusan National University School of Medicine, Yangsan, Gyeongnam 50612,Republic of Korea
Dear Editor,
Sarcoidosis is a systemic disorder of unknown etiology characterized by non-caseating epithelioid granulomas.The lungs, lymph nodes, liver, spleen, phalangeal cartilages,parotid glands, eyes, and skin are affected[1]. Cutaneous sarcoidosis is seen in 10%-38% of patients with systemic disease[2]. Scar infiltrates may appear early in the disease before pulmonary parenchymal changes and may be associated with hilar lymphadenopathy[3]. At present, scar sarcoidosis following blepharoplasty have been rarely reported. Here, we reported two unusual cases of scar sarcoidosis with pulmonary involvement after upper blepharoplasty.
All procedures performed in this case were in accordance with the ethical standards of the Institutional Review Board of Pusan National University Yangsan Hospital in Republic of Korea and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. Written informed consent was obtained from the patients.
Case 1A 61-year-old woman presented with a 3-month history of linear, erythematous, and non-tender bilateral eyelid swelling. She had undergone bilateral upper blepharoplasty approximately 30 years ago. The patient had no history of cancer, genetic disease, diabetes, or hypertension. Physical examination revealed thick and raised papules along the blepharoplasty scars that were conspicuously non-pruritic(Figure 1A).
Ophthalmic examination revealed no ocular inflammation or fundus abnormality. An incisional biopsy was performed on the eyelid lesion, and histopathological examination revealed numerous, non-caseating granulomas with multinucleated giant cells surrounded by relatively few lymphocytes (Figure 2A).Asteroid bodies were found within giant cells (Figure 2B).These findings are presumed of sarcoidosis. No foreign body was observed, and the polymerase chain reaction (PCR) forMycobacterium tuberculosiswas negative. Routine laboratory measurements, including tests for complete blood counts,erythrocyte sedimentation rate, liver and renal function, and immunoglobulin G4 levels, showed normal results. The patient’s serum angiotensin-converting enzyme level was elevated at 120 U/L (normal: 20-70 U/L).
Furthermore, the patient experienced mild nocturnal coughs.The patient underwent chest radiography and computed tomography (CT). The chest radiograph revealed bilaterally enlarged hilar and mediastinal lymph nodes; CT revealed bilateral interlobar lymph node enlargement and multiple indeterminate nodules at indeterminate locations in both the lungs (<7 mm; Figure 2C, 2D). Upper and lower abdominal CT scans showed normal results. The patient’s symptoms were not severe; thus, the pulmonologists decided to manage the patient with regular follow-up and CT monitoring of the lung lesions.
The eyelid lesions resolved completely after four subcutaneous injections of triamcinolone acetate and the application of dexamethasone ointment for approximately 3mo (Figure 1B).At 2y post-treatment, evidence of eyelid lesion recurrence and lymph node enlargement in the bilateral lungs was absent.
Case 2A 55-year-old woman who had undergone bilateral upper blepharoplasty 15y previously presented with linear and purplish-red papules on the nasal aspect of the right eye(Figure 3A).
Furthermore, the patient had a non-tender and subcutaneous nodule on the right knee (Figure 4A). The patient had no history of cancer, endocrine disease, or drug abuse.An incisional biopsy was performed on the eyelid lesion.
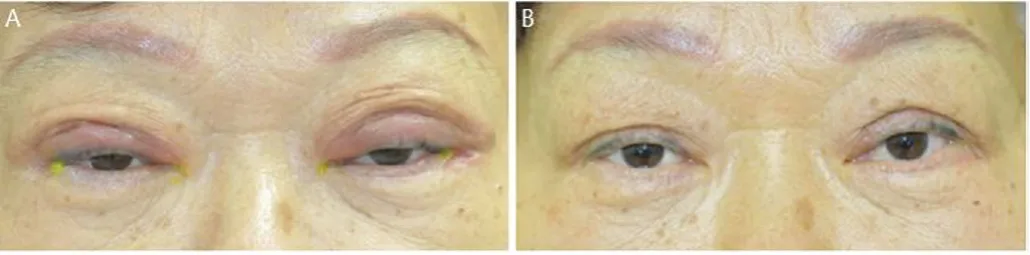
Figure 1 Photographs from Case 1 Α: Linear, erythematous, firm,but non-tender eyelid swelling in both eyelids; B: Resolution of the eyelid lesions after intralesional steroid injections and steroid ointment application.

Figure 2 Histopathological and radiological images from Case 1 A: Non-caseating granulomatous inflammatory structures with multinucleated giant cells (arrowheads) surrounded by relatively few lymphocytes (hematoxylin and eosin-stained specimens, 400×magnification); B: The giant cells contain asteroid bodies (arrow);C: Chest X-ray shows bilateral hilar enlargement (arrows); D: Chest computed tomography reveals interlobar lymphadenopathy and multiple widespread, indeterminate, pulmonary nodules (arrow).
Histopathological examination revealed non-caseating epithelioid granulomas with multinucleated giant cells and occasional lymphocytes, suggested with sarcoidosis (Figure 4B). Additionally,Mycobacterium tuberculosis(MTB) andNontuberculosis mycobacteria(NTM)using real-time PCR was negative. Routine laboratory tests, including that for angiotensin-converting enzyme levels, showed normal results.We performed a systemic evaluation using chest radiography and CT. Chest radiography revealed a bilaterally enlarged hilar lymph node, while CT revealed multiple enlarged lymph nodes in the upper/lower paratracheal, subcarinal, hilar, and interlobular regions (Figure 4C, 4D). All abdominal CT scans showed normal results. The patient underwent bronchoscopy and aspiration biopsies of the lung lesions in the Pulmonology Department. Histopathology revealed a granuloma without necrosis and no evidence of tuberculosis.
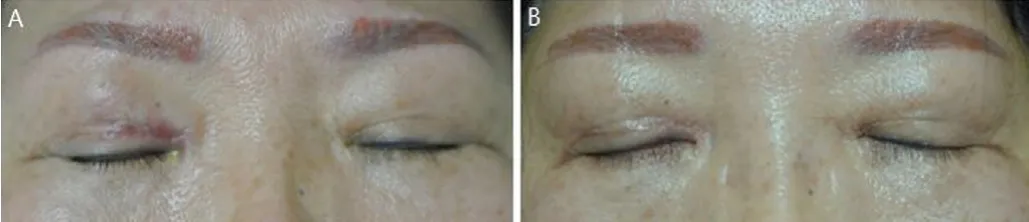
Figure 3 Photographs from Case 2 A: Linear and purplish-red papules on the nasal aspect of eyelid crease in right eye; B: Resolution of the eyelid lesion after intralesional steroid injections and systemic steroids.

Figure 4 Systemic, histopathological, and radiological images from Case 2 A: Subcutaneous nodule in the right knee; B:Histopathological images of non-necrotizing, non-caseating,granulomatous inflammation (hematoxylin and eosin-stained specimens, 400× magnification); C: Chest X-ray shows bilateral hilar enlargement (arrows); D: Chest computed tomography reveals enlargement of interlobar lymphatic nodules in the hilar and interlobular areas (arrow).
The eyelid lesions completely resolved after subcutaneous triamcinolone acetate injections and oral steroid (40 mg/d)treatment for approximately 1mo (Figure 3B). In addition,the size of the subcutaneous nodule on the right knee and pulmonary lymph nodes decreased after systemic steroid treatment. At 1y post-treatment, there was no evidence of recurrence of the eyelid and pulmonary lesions.
Scar sarcoidosis is a rare but specific form of cutaneous sarcoidosis in which old scars are infiltrated by non‐caseating epithelioid cell granulomas. The exact incidence of scar sarcoidosis is unknown but has been reported to range from 2.9% to 13.8% in a series of adults with cutaneous sarcoidosis[4]. Scar sarcoidosis has been reported at the sites of previous wounds, sites of intramuscular injection, blood donation punctures, tattoo scars, herpes zoster scars, ritual scars, sites of desensitization injections, sites of hyaluronic acid injections, and scars from laser surgeries[5]. Scar sarcoidosis may be isolated or may precede or accompany systemic sarcoidosis. Most patients present with bilateral hilar lymphadenopathy and restrictive lung disease[3].Reports of scar sarcoidosis with systemic involvement after blepharoplasty in the literature are rare. Kwonet al[6]reported a case of linear scar sarcoidosis on a thin blepharoplasty line; however, systemic involvement was not reported.The study[7]presented a case of eyelid scar sarcoidosis that developed after trauma (but not blepharoplasty).
A previous study reported that systemic involvement occurred in 30% of patients who had isolated cutaneous lesions after a period of 1mo to 1y[4]. Our cases showed cutaneous involvement with scar sarcoidosis together with hilar and mediastinal lymphadenopathy. Case 1 had only pulmonary involvement, but Case 2 had pulmonary and knee joint involvement with eyelid sarcoidosis.
Scar sarcoidosis generally presents as a diffuse infiltration of a scar, such as a keloid or hypertrophic scar, or as focal papules, nodules, and subcutaneous nodules, in the scar area[7]. The cutaneous lesions initially develop as purplish-red erythema and subsequently turn brown and are non-pruritic[2].The reported latency period of scar sarcoidosis before its reactivation in old cutaneous scars is between 6mo and 59y[8].Cases 1 and 2 showed latency periods of approximately 30y and 15y after blepharoplasty, respectively.
The differential diagnosis of scar sarcoidosis includes infectious skin diseases (e.g., mycobacterial infections),hypertrophic scars, keloids, and foreign body granulomatous diseases[8].
Eyelid scar sarcoidosis was treated with intralesional triamcinolone acetate injections or systemic oral steroids in our cases. However, systemic involvement, including hilar lymphadenopathy of the lung, should be monitored by medical doctors.
Scar sarcoidosis should be considered when nonspecific eyelid swelling occurs in patients with a history of eyelid surgery.Systemic examinations, such as chest radiography and CT,should be considered, especially if the patient presents with pulmonary involvement, after histopathologic results have been confirmed.
ACKNOWLEDGEMENTS
The authors would like to thank the patients and their families for providing consent regarding the collection and publication of clinical data.
Conflicts of Interest: Suh SY,None;Ahn JH,None.
 International Journal of Ophthalmology2021年8期
International Journal of Ophthalmology2021年8期
- International Journal of Ophthalmology的其它文章
- Macular density alterations in myopic choroidal neovascularization and the effect of anti-VEGF on it
- ldentification and validation of tumor microenvironmentrelated lncRNA prognostic signature for uveal melanoma
- Factors associated with axial length elongation in high myopia in adults
- Visualizing the intellectual structure and recent research trends of diabetic retinopathy
- Therapeutic effect of Keap1-Nrf2-ARE pathway-related drugs on age-related eye diseases through anti-oxidative stress
- Newly-found functions of metformin for the prevention and treatment of age-related macular degeneration
