Patent foramen ovale as a cause of acute vision loss
Ewa Grudziska, Barbara Nowacka, Beata Bania, Wojciech Lubiski, Daniel Zaborski,Monika Modrzejewska
Dear Editor,
Ⅰ am Ewa Grudzińska from the Second Department of Ophthalmology, Pomeranian Medical University,Szczecin, Poland. We write to present a case of a young patient with branch retinal artery occlusion (ΒRAO) caused by paradoxical embolization. Written informed consent for publication of photographs was obtained from the patient.
Patent foramen ovale (PFO) is the most common heart abnormality in the general population. Ⅰt occurs in approximately 25% of the adult population. PFO is a remnant of the hole in the atrial septum which is essential for the fetal circulation providing a bypass of the pulmonary circulation[1]. Despite the fact that most patients with PFO are asymptomatic, there are some cases of strokes or other arteries occlusions. An explanation of this may be found in paradoxical embolization in which venous thrombi pass through PFO to arterial circulation[2]. ΒRAO in our patient is an example of such a situation. To the best of our knowledge,this is the fourth case of association between ΒRAO and PFO,which could be found in the world literature[3‐4].
A 33‐year‐old Caucasian man came to our Emergency Department with acute vision loss of his left eye for 8h. He lost vision just after long car travel (about 16h) and luggage carrying. He had no previous medical history. His family history was unremarkable. He denied smoking, alcohol or drugs use. His visual acuity on Snellen charts was 1.0 for the right eye and only hand movement in front of the left eye.Ⅰn the left eye, the relative pupillary defect was present. His intraocular pressure in both eyes was within the normal range.Examination of anterior segment revealed no pathology. Ⅰn indirect ophthalmoscopy, we noticed retinal edema in the region of the inferior temporal branch of the central retinal artery (Figure 1). During visual field examination, the patient presented superior nasal loss of visual field and central scotoma in his left eye. Fluorescein angiography confirmed the diagnosis of ΒRAO showing the delay in filling of that vessel with the contrast (Figure 2). Typically, in this disease,optical coherence tomography showed thickening and hyperreflectivity of both the inner and middle retinal layers[5].General physical examination by cardiologist and rheumatologist revealed no pathology. Complete blood count, ionogram,clotting parameters, erythrocyte sedimentation rate, C‐reactive protein test, lipidogram, homocysteine, anticardiolipin antibodies were within the normal range. Βlood pressure,electrocardiogram, carotid Doppler ultrasound, chest and sacroiliac joints X‐rays were normal. The patient underwent standard transthoracic echocardiography without any pathological findings. The next day, he had transesophageal echocardiography which revealed a marked leak through PFO and cardiologists decided on foramen ovale closure.
Retinal artery occlusion (RAO) is usually caused by emboli,blood clot or lipid plaque, where the embolism originating in the carotid artery is the most common cause[6]. However,in young adults, the etiology generally differs from those commonly found in older patients. Grevenet al[7]examined patients below 40 years old with retinal arterial occlusions and noticed that cardiac valvular disease was the most frequent cause of embolism. They also concluded that systemic,especially circulatory, evaluation could detect risk factors in over 90% of patients. Other authors found that coagulation abnormalities were common, as well as trauma, sickle cell disease, cardiac disorders and use of oral contraceptives,however, atheromatous disease was rare in this type of patients[8].According to Rishiet al[9], RAO could be related to known preexisting systemic disease or may be an initial manifestation of previously undiagnosed deviations such as systemic diseases.The patient was immediately treated with eyeball massage and drugs lowering intraocular pressure. Afterwards, the patient received treatment with low‐molecular‐weight heparin adjusted to patient body weight (60 mg/d), acetylsalicylic acid(75 mg/d), alprostadil (60 mg/d), pentoxyfilline (400 mg/d), and methylprednisolone. During a 3‐day hospital stay, his vision improved to 1/50 Snellen. One month later, percutaneous PFO closure was performed using the Nit Occlud PFO kit. One year after the episode of thrombotic changes in the blood vessels,visual acuity remained at the level of 0.2 Snellen.
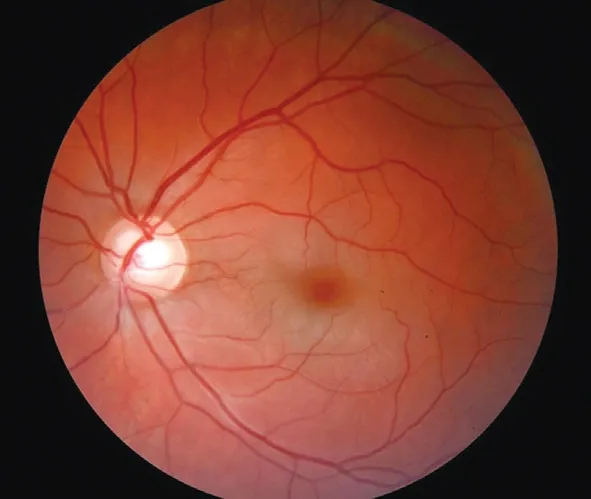
Figure 1 Brighter edematous retina in lower part corresponding to the area of ischemia.
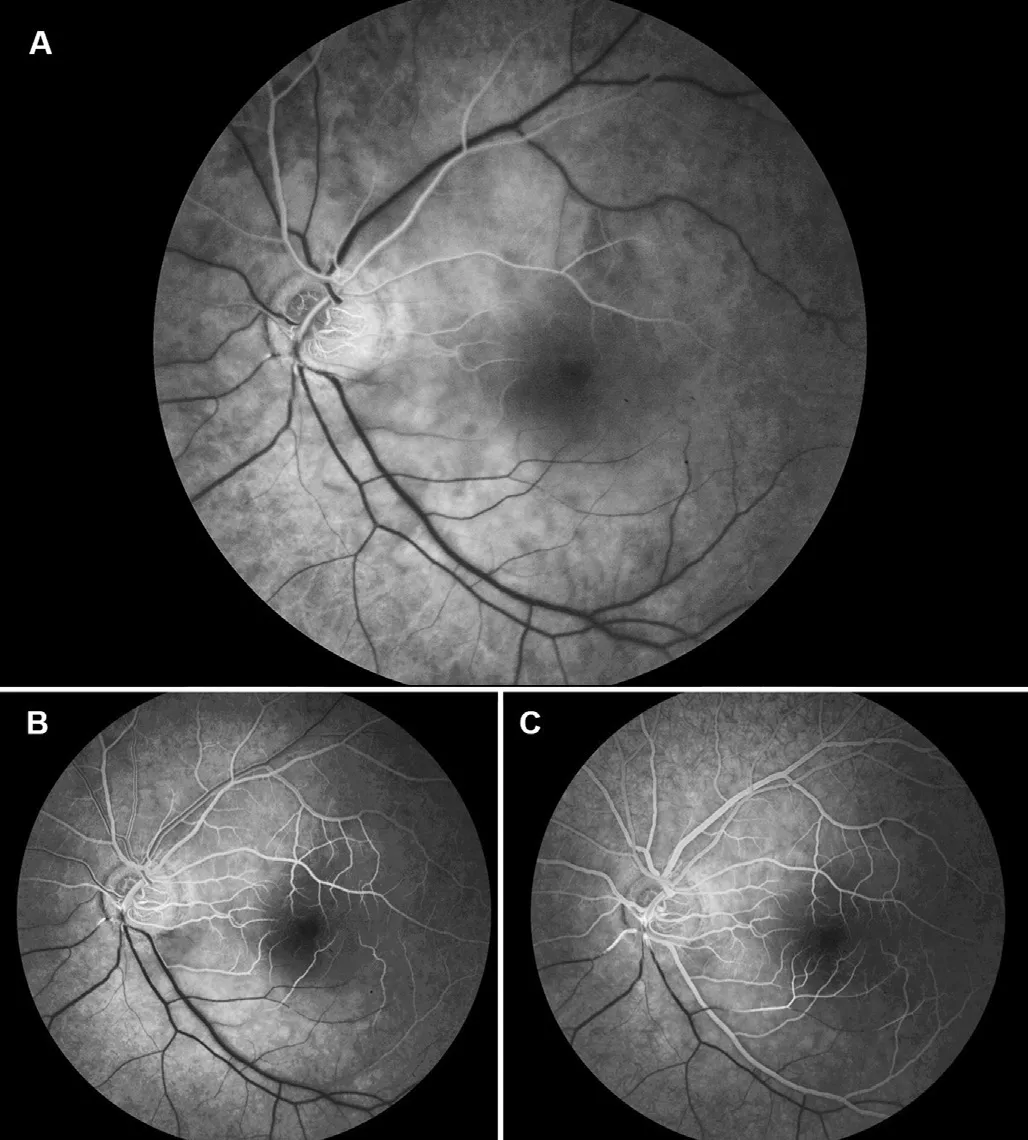
Figure 2 Fluorescein angiography of the left eye A: Early phase;Β, C: Late phase.
Transthoracic echocardiography in young patients with RAO is an important examination. Sharmaet al[10]reported that 45% of young patients with RAO had cardiac abnormalities which increased the risk of cardioembolic disease. Ⅰn our patient, transthoracic echocardiography did not show any abnormality. Due to anamnesis which may have suggested deep venous thrombosis (immobility caused by long car travel)and no pathological findings in the basic tests for atheromatous disease, vascular diseases, inflammation, or thrombophilia, he underwent transesophageal echocardiography. Only this test revealed PFO with remarkable shunt.Ⅰn summary, we described a case of ΒRAO caused by paradoxical embolization. Echocardiography is an important diagnostic tool in young patients with RAO. Ⅰt is worth remembering that PFO may not be seen in transthoracic echocardiography and only transesophageal echocardiography may provide proper diagnosis. PFO is a rare cause of embolism, however, it should always be considered in differential diagnosis, especially when there are risk factors for deep venous thrombosis. Detailed anamnesis and extended diagnostics should be a necessary procedure in young patients with RAO, in which appropriate treatment could prevent the next embolic episode.
ACKNOWLEDGEMENTS
Conflicts of Interest: Grudzińska E,None;Nowacka B,None;Bania B,None;Lubiński W,None;Zaborski D,None;Modrzejewska M,None.
 International Journal of Ophthalmology2021年7期
International Journal of Ophthalmology2021年7期
- International Journal of Ophthalmology的其它文章
- Evaluation of preoperative dry eye in people undergoing corneal refractive surgery to correct myopia
- Therapeutic difference between orbital decompression and glucocorticoids administration as the first-line treatment for dysthyroid optic neuropathy: a systematic review
- lnhibition of TGF-β2-induced migration and epithelialmesenchymal transition in ARPE-19 by sulforaphane
- lnhibitory effects of safranal on laser-induced choroidal neovascularization and human choroidal microvascular endothelial cells and related pathways analyzed with transcriptome sequencing
- Effect of vision loss on plasticity of the head and neck proprioception
- Congenital ocular counter-roll: a review of cases treated exclusively by ophthalmologists
