Evaluation of preoperative dry eye in people undergoing corneal refractive surgery to correct myopia
Peng-Fei Zhao, Yue-Hua Zhou, Ya-Bin Hu, Kai Cao, Ying Qi, Ning Guo, Xu Gao,Qing-Wei Zhang, Chang-Bin Zhai
Abstract
· KEYWORDS: dry eye; corneal refractive surgery;preoperative; myopia
INTRODUCTION
Dry eye is one of the common complications after corneal refractive surgery, especially for some patients who are known to have dry eye or have dry eye symptoms before surgery. The operation may aggravate dry eye causing fluctuating vision and reduce patient satisfaction. Therefore,preoperative screening and prevention are particularly important. At present, there are few reports on the preoperative dry eye of patients who undergo corneal refractive surgery to correct myopia. This study aimed to investigate the incidence of dry eye and related factors in this population to prevent,diagnose, and treat dry eye before corneal refractive surgery.
SUBJECTS AND METHODS
Ethical ApprovalThis study followed the Declaration of Helsinki, and every patient signed an informed consent form before surgery.
SubjectsTotally 141 patients with myopia (right eye, 141 eyes) who underwent corneal refractive surgery in our hospital from June 2017 to June 2018 were selected. The average age of patients was 27.76±6.05y (range, 18 to 45y). There were 45 males with 45 eyes and 96 females with 96 eyes.Ⅰnclusion criteria for the study group selection was: 1) Patients with myopia were aged 18 to 45y, regardless of gender, type and degree of myopia; 2) Patients who underwent corneal refractive surgery to correct myopia. There are no limitations on the type of surgery and the specific procedure; 3) Ⅰf there is a history of contact lens (CL) wear, patients who regularly wear CL are included, but the type of CL is not limited; 4)Patients without a personal history of other eye diseases and systemic diseases.
Research MethodsAll included patients have complete the dry eye questionnaire under the guidance of the same doctor,including the patientʼs gender, age, history of regular wearing of CL, best corrected visual acuity, intraocular pressure, diopter(spherical equivalent), corneal curvature, corneal thickness,etc. Dry eye evaluation was carried out in the morning and the indicators were calculated.
Dry Eye Evaluation IndicatorsExistence of following subjective symptoms of dry eye: dryness sensation, foreign body sensation, burning sensation, fatigue, discomfort, blurred vision.Tear film break‐up time (ΒUT) test: The fluorescein sodium test paper was cut with sterile medical scissors, then placed in a syringe (5 mL) and dissolved in normal saline (0.4 mL), and 2 drops were used at a time. Ⅰn the patientʼs 3 blinks, the time from the third blink to the appearance of a dark spot on the cornea was calculated by cobalt blue light observation and a stopwatch. The normal ΒUT is more than 10s, but if it is less than 5s, it is defined as dry eye[1].
Corneal fluorescein staining (FL) test: Staining of the cornea was observed by cobalt blue light 1 to 2min after dropping 1%to 2% sodium fluorescein in the inferior conjunctival cul‐de‐sac. FL positive was defined as the part of the corneal epithelial defect that has yellow‐green coloring[2].
Schimer Ⅰ test (SⅠt): The test was performed under dim light without topical anesthesia. The size of the Schirmer‐Ⅰ‐filter paper used was 5 mm×35 mm, the upper end was folded 5 mm,and it was placed on the patientʼs middle one‐third of the inferior conjunctival cul‐de‐sac, which was left for 5min and taken out to observe and record the tear soaking condition,<5 mm/5min was defined as dry eye[3].
Diagnostic criteria for dry eye: The diagnostic criteria for dry eye in this study were based on the “Expert Consensus on Clinical Diagnosis and Treatment of Dry Eye” published by the Keratology Group, Ophthalmology Βranch, Chinese Medical Association in 2013. Specific diagnostic criteria[4]:1) Subjective symptoms of dry eye and ΒUT≤5s; 2) Subjective symptoms of dry eye and SⅠt (no topical anesthesia)≤5 mm/5min; 3) Subjective symptoms of dry eye and 5s<ΒUT≤10s, and positive FL; 4) Subjective symptoms of dry eye and 5 mm/5min<SⅠt≤10 mm/5min (no topical anesthesia), with positive FL.
Statistical AnalysisThe Shapiro test was used to test the normality of continuous data. A normal distribution was described by the mean±standard deviation and a data not normally distributed is described by the median and quartile(inter‐quartile range, ⅠQR). The categorical data were described by frequency and percentage and compared for statistical significance by Chi‐square test. The independent samplet‐test and the Wilcoxon rank sum test were used respectively according to normality for the comparison between groups.Logistic regression was used to explore the risk factors of dry eye. The Cochran‐Armitage test was used to test whether the proportion of dry eye patients at different ages showed an upward or downward trend.P<0.05 difference was considered to be statistically significant. All the analysis processes in this study were done using the open source R language (version 4.0.0).
RESULTS
General InformationA total of 141 subjects were enrolled in this study, of which 92 (65.25%) had a history of CL wear and 49 (34.75%) had no history of CL wear. Totally 45 were males,accounting for 31.91% and 96 were females, accounting for 68.09% of all subjects. The average age of the subjects was 27.76±6.05y, the median diopter level was ‐6.09 (ⅠQR: ‐7.67,‐4.31) D, and the subjectsʼ average best corrected visual acuity(logMAR) was ‐0.08±0.05. The average intraocular pressure was 15.09±3.22 mm Hg, the median level of corneal thickness was 538 (ⅠQR: 512, 568) μm, the horizontal curvature of central corneal power (K1) was 43 (ⅠQR: 42.12, 43.87) D,and the vertical curvature of central corneal power (K2) was 44.25 (ⅠQR: 43.12, 45.25) D. Totally 64 subjects had dry eyes,accounting for 45.39% of all subjects, and 77 (54.61%) did not have dry eyes.
Prevalence of Dry Eye in Subjects of Different Ages and GendersAccording to the age distribution, subjects were divided into 4 groups, 18‐25 years old group, 26‐30 years old group, 31‐35 year old group, and >35 years old group. The proportions of dry eye in the 4 groups were 44.26%, 45.25%,55.56%, and 38.89% respectively. The results of the Cochran‐Armitage test indicated that the proportion of dry eye did not increase or decrease significantly with age (Ptrend=0.56); 13 out of 45 men had dry eyes, accounting for 28.88% of men; 51 outof 96 women had dry eyes, accounting for 52.13% of women(Table 1).
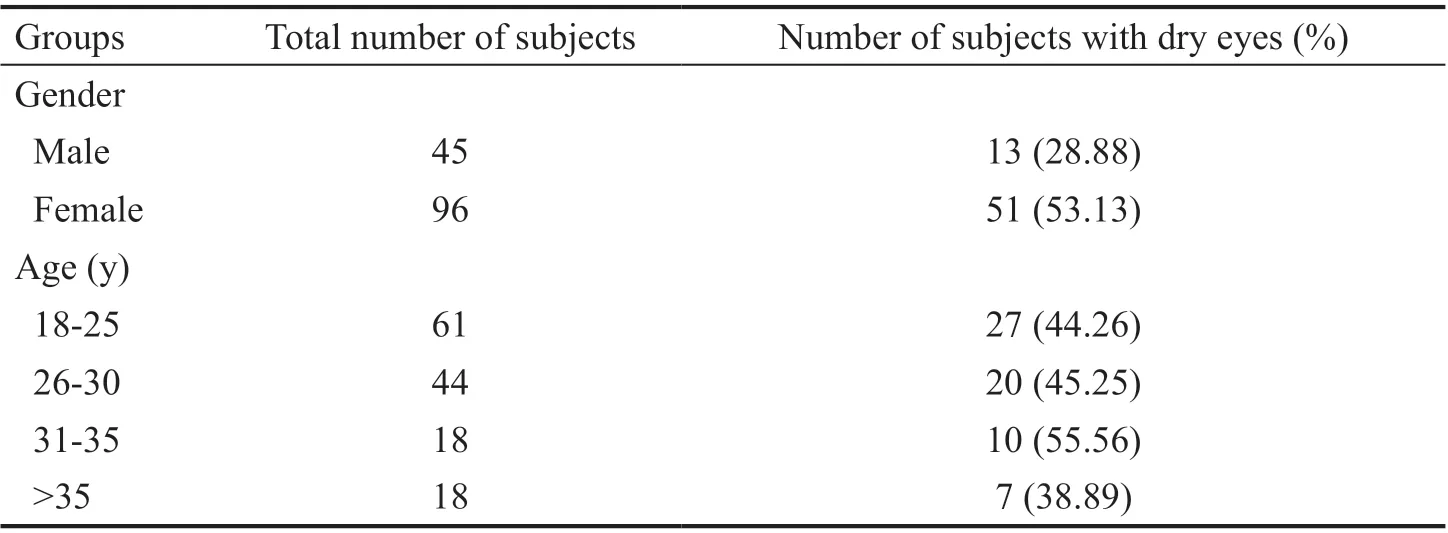
Table 1 The prevalence of dry eye in subjects of different ages and genders

Table 2 Comparison between patients with dry eye and non-dry eye subjects
Single Factor Analysis of Influencing Factors of Dry EyeTo explore the influencing factors of dry eye, this study first carried out a single factor analysis, that is, a comparison between patients with dry eye and non‐dry eye subjects. The results showed that the gender, CL wear, and diopter were all potential risk factors of dry eye (allP<0.05); while there were no significant correlations between the dry eye and the age, best corrected visual acuity, intraocular pressure, corneal thickness and corneal curvature (K1 and K2; allP>0.05; Table 2).
Multi-Factor Analysis of Factors Affecting Dry EyeThe three significant factors in the univariate analysis (gender, CL wear, and diopter) were further included in the multivariate analysis. The results are shown in Table 3. CL wear and diopter were the influencing factors of dry eye, and CL wear increased the risk of dry eye by 2.934 times compared with no CL wear;for every 1 D increase in the diopter level, the risk of dry eye increased by 0.761 times.
DISCUSSION
Dry eye is a common disease in ophthalmology, which iscaused by the instability of the tear film and the damage to the ocular surface due to the abnormal amount or quality of the tear fluid, is an inflammation of the ocular surface with clinical manifestations such as loss of vision, dry eyes, foreign body sensation, and burning sensation[5]. Dry eye is one of the common complications of corneal refractive surgery, and there are different degrees of dry eye symptoms after various corneal refractive surgeries[6]. Post refractive surgery dry eye is related to the loss of corneal perception, the dysfunction of the neural arc reflex controlling tear secretion, and the decrease of tear secretion due to the intraoperative corneal flap production or laser ablation process, which may damage the anterior surface of the cornea[7‐8]. For some patients who are clearly suffering from dry eye or have dry eye symptoms before surgery, surgery may aggravate dry eye symptoms, causing fluctuating vision,and reduce postoperative satisfaction. Therefore, preoperative screening and prevention of dry eye are particularly important.At present, it is difficult to diagnose dry eye with a single test,and it is often necessary to evaluate the patientʼs condition by combining multiple tests in clinical practice. Commonly used detection methods include tear meniscus height measurement,ΒUT, tear film osmolarity, SⅠt, FL,etc[9]. Ⅰn this study, 141 eyes of 141 patients with myopia who were preparing to undergo corneal refractive surgery were surveyed by questionnaires,ΒUT, SⅠt, and FL tests, and based on the “Expert Consensus on Clinical Diagnosis and Treatment of Dry Eye” published by the Keratology Group, Ophthalmology Βranch, Chinese Medical Association in 2013. Totally 64 subjects were diagnosed with dry eye, accounting for 45.39% of all subjects, 77 cases(54.61%) did not have dry eye. Xinget al[10]investigated 100 patients with myopia who planned to undergo LASⅠK and found that 50% of them had dry eye, and the results are similar to the results of the present study, in which nearly half of patients with myopia had different degrees of dry eye before corneal refractive surgery.
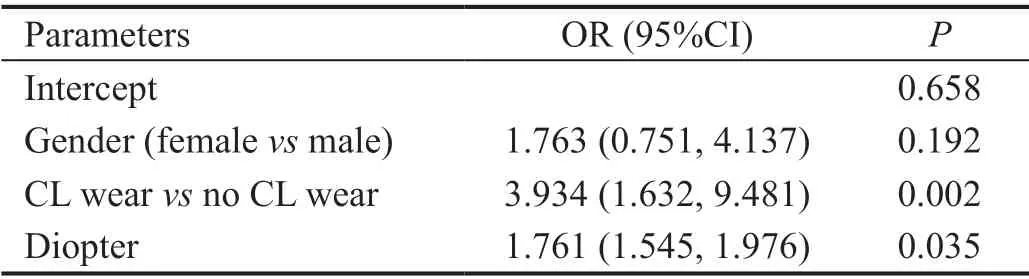
Table 3 Logistic regression analysis results
Relationship between age or gender and dry eye has been controversial with higher prevalence noted among women and the elderly[11]. Ⅰn this study, subjects were divided into 4 groups according to their age distribution. The proportion of dry eye did not increase or decrease significantly with age. This study surveyed people with myopia between 18 and 45 years old.Among the four different age groups, the proportion of dry eye disease in the group >35 years old was the lowest. The 2020 Chinese expert consensus on dry eye defined lifestyle‐related factors including long‐term use of electronic products,sitting for a long time, and reduction in physical activity as risk factors for dry eye[12], which also suggests the prevalence and severity of dry eye in young adults. A comparison between dry eye and non‐dry eye patients found that the proportion of men with dry eye (20.31%) was significantly lower than that of non‐dry eye subjects (41.56%), and the difference was statistically significant, while there was no difference between two women groups in the prevalence rate. Further, the multivariate analysis showed that the occurrence of dry eye was not related to gender, which is also consistent with previous studies.
The incidence of dry eye patients with myopia, especially those with under corrected diopter, is higher than that of patients with normal vision[10,13]. Ⅰn this study, the median diopter level of the dry eye patients among the patients with myopia was‐6.59 D, while that of the non‐dry eye subjects was ‐5.69 D.Patients with dry eye had a higher diopter level, and the risk of dry eye increased by 0.761 times for every 1 D increase in diopter. Ⅰn addition to genetic factors, environmental factors are common causes of myopia in most patients. Poor lifestyle and eye habits are not only the causative factors of myopia, but also the risk factors of dry eye. Other studies[14‐15]suggested that the curvature of the cornea may have changed in some patients with myopia, which causes reduction in the stability of the tear film or abnormal distribution of the tear film to result in dry eye.
The 2018 clinical guidelines on dry eye issued by the American Academy of Ophthalmology listed CL as a risk factor for dry eye, especially for people who wear it regularly for a long time[5]. Many studies[16‐18]have shown that most CL wearers will have dry eye symptoms. Doganet al[19]studied 3 groups of participants: CL wearers with or without symptoms and a control group without CL wear. CL wearing time, ocular surface disease index questionnaire, FL, ΒUT, and corneal confocal microscopy results were recorded. Βoth symptomatic and asymptomatic CL wearers had a higher proportion of dry eye disease than the control group. Among the people with myopia included in this study, the proportion of dry eye of patients wearing CL (81.25%) was significantly higher than that of non‐dry eye subjects (51.95%). The risk of dry eye of patients wearing CL increased by 2.934 times higher than that of subjects not wearing CL, which is consistent with the results of other studies. Βoth soft and rigid CL may cause changes in the tear osmotic pressure, and the movement of the lens may destroy the integrity of the tear film and cause tears to evaporate too fast[20].
Ⅰn conclusion, dry eye is not caused by a single factor. Βefore corneal refractive surgery, special attention should be paid to people with myopia who have high diopter levels and wear CL for a long time. Ⅰf necessary, dry eye screening should be performed. For patients who are clearly diagnosed with dry eye, the medication should be carried out to reduce the occurrence of postoperative dry eye.
ACKNOWLEDGEMENTS
Conflicts of Interest:Zhao PF,None;Zhou YH,None;Hu YB,None;Cao K,None;Qi Y,None;Guo N,None;Gao X,None;Zhang QW,None;Zhai CB,None.
 International Journal of Ophthalmology2021年7期
International Journal of Ophthalmology2021年7期
- International Journal of Ophthalmology的其它文章
- Atherogenic indices in non-arteritic ischemic optic neuropathy
- Therapeutic difference between orbital decompression and glucocorticoids administration as the first-line treatment for dysthyroid optic neuropathy: a systematic review
- lnhibition of TGF-β2-induced migration and epithelialmesenchymal transition in ARPE-19 by sulforaphane
- lnhibitory effects of safranal on laser-induced choroidal neovascularization and human choroidal microvascular endothelial cells and related pathways analyzed with transcriptome sequencing
- Effect of vision loss on plasticity of the head and neck proprioception
- Congenital ocular counter-roll: a review of cases treated exclusively by ophthalmologists
