Ocular surface squamous neoplasia resistant to topical interferon alpha 2b in a patient with follicular lymphoma
Valentin Huerva, Magi Vilaltella
Dear Editor,
Treatment for ocular surface squamous neoplasia (OSSN)includes topical mitomycin C (MMC), 5‐fluorouracil(5‐FU) and interferon (ⅠFN)‐alpha 2b eyedrops[1‐2]. Compared to other treatments, such as mitomycin C (MMC), ⅠFN‐alpha 2b is well tolerated and causes fewer side effects[1‐2]. A success rate of 76%‐100% tumor eradication has been reported with ⅠFN‐alpha 2b treatment[1‐2]. Furthermore, recurrences have been successfully re‐treated with ⅠFN‐alpha 2b and this approach has been used as a co‐adjuvant after surgery[1‐3].ⅠFN‐alpha 2b is a cytokine with antiviral, cytotoxic, and immunomodulatory activities. However, the exact effector mechanism is not well‐known. Thus, it is difficult to clearly establish which patients will not respond to ⅠFN‐alpha 2b treatment. Ⅰmmunosuppression is associated with patient response to this treatment modality[4].
A‐70‐year‐old Caucasian man with retroperitoneal non‐Hodgkinʼs follicular Β‐cell lymphoma had undergone chemotherapy with obinutuzumab. He presented to our clinic for evaluation of an asymptomatic red lesion in his right eye that had persisted for 3mo. Βiomicroscopy revealed a nasal conjunctival lesion, 4×5 mm2in size and raised; it exhibited limbal involvement and corneal invasion, as well as leukoplakia and significant vascular dilatations (Figure 1A).The lesion was clinically diagnosed as OSSN. The patient was fully informed about the possible treatments or interventions and his informed consent was obtained. This study was conducted in accordance with the ethical standards in the Declaration of Helsinki.
Treatment with ⅠFN‐alpha 2b eye drops (1 000 000 UⅠ/mL)was initiated at four doses per day. After 3mo, there were no clear changes in lesion size or appearance (Figure 1Β); thus,the treatment was changed to MMC 0.02% eye drops, four times per day. Digital punctal occlusion was used after the instillation. Four cycles of MMC treatment were performed,consisting of 1wk of treatment per cycle, separated by 1wk of rest between cycles. No clear changes were observed after MMC treatment, and the lesion persisted (Figure 1C).Compliance with treatment during the first 3mo of treatment with ⅠFN‐alpha 2b was investigated. After consultation with the patient and further emphasis regarding the importance of strict adherence to treatment guidelines, ⅠFN‐alpha 2b treatment was restarted for an additional 3mo; however, this elicited no definitive therapeutic response (Figure 1D). At this time, due to a long time with topical administration, he did not want to try a new chemotherapy with 5‐FU. Due to the failure of local chemotherapy, excisional biopsy of the lesion with safety margins was performed using cryocoagulation of the margins and underlying sclera, and conjunctival autograft with tissue adhesive. The sample was sent for pathology analysis,which confirmed the diagnosis of moderate epithelial dysplasia OSSN (Figure 2). After 12mo of follow‐up, and without adjuvant treatment, the patient exhibited no recurrence.
The mechanism of action of ⅠFN‐alpha 2b treatment in OSSN is not well established. ⅠFN‐alpha 2b is a cytokine with antiviral, immunomodulatory, and antineoplastic activities;it is produced and secreted mainly by blood leukocytes in response to viral infection[2]. The exact mechanism of its action is complex, with various interrelated activities; however, ⅠFN‐alpha 2b appears to combine with specific membrane receptors on the cell surface, triggering a cascade of biological effects[2,5].These effects include enhancement of macrophage phagocytic activity, augmentation of T8 lymphocyte and natural killer cell specific cytotoxicities for target cells, induction of effector enzymes, suppression of cell proliferation, and inhibition of virus replication in virus‐infected cells[2,5]. Additionally, ⅠFN‐alpha 2b interacts with both tumor cells and immune cells,causing a reciprocal interaction[5].
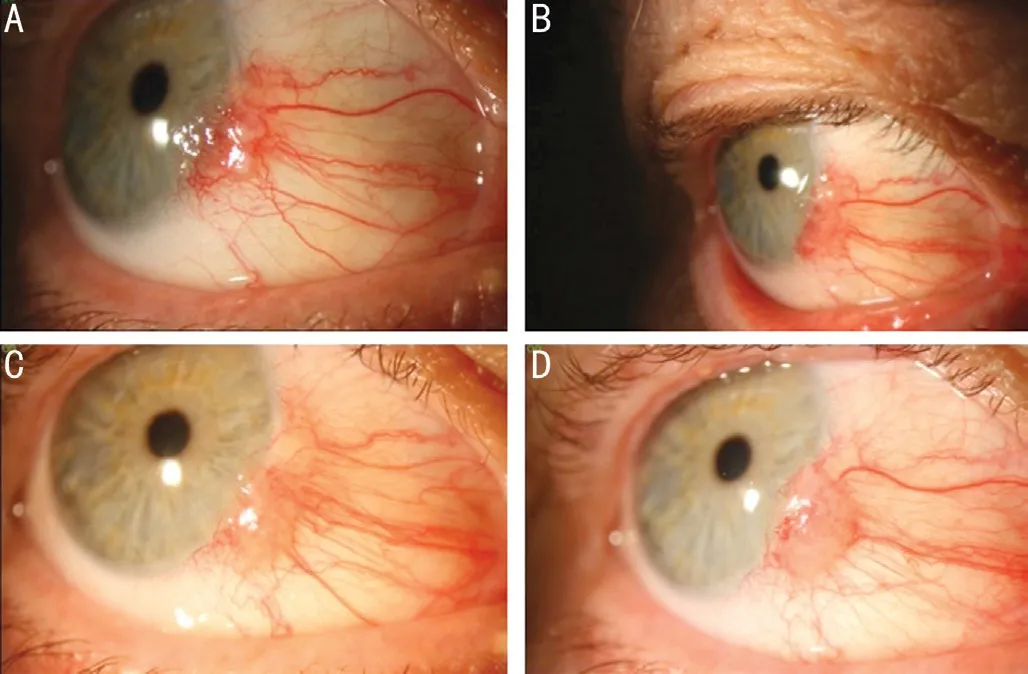
Figure 1 An asymptomatic red lesion in right eye of a 70-yearold man with retroperitoneal non-Hodgkin’s follicular B-cell lymphoma undergone chemotherapy with obinutuzumab A:Βiomicroscopic photograph from the first visit; Β: Clinical findings after 3mo of topical ⅠFN‐alpha 2b eyedrop treatment, four times per day: The size is practically the same as at the beginning of the treatment, about 4×5 mm2; C: Ocular surface squamous neoplasia(OSSN) that was resistant to four cycles of mitomycin C 0.02% eye drops, four times per day; D: Clinical findings after the new regimen of topical ⅠFN‐alpha 2b eye drop treatment. Three months later, the lesion persisted and appeared to be larger than at the initial visit.
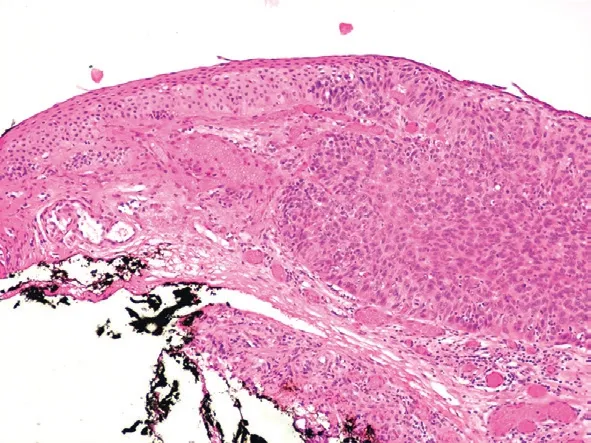
Figure 2 Pathologic analysis which confirmed OSSN Thickened of the conjunctival epithelium with cytological atypia (right) and abrupt transition between the involved conjunctiva and the adjacent normal appearing conjunctival epithelium (left). The basement membrane is intact. The base of the excision is free of dysplastic cells. Moderate dysplasia squamous intraepithelial lesion, abnormal transformation of epithelium involving more than 2/3 of epithelial thickness. The degree of cell atypia is not sufficient to term this lesion as severe dysplasia.Hematoxylin and eosin staining at 10× magnification.
MMC has been used effectively as primary or adjuvant treatment for OSSN[1,6‐7]. Ⅰts mechanism of action is different from that of ⅠFN‐alpha 2b. Notably, ⅠFN‐alpha 2b acts immunologically, whereas MMC acts to inhibit nucleic acid synthesis[8]. MMC‐resistant OSSN has been previously reported[9]; for treatment of these patients, ⅠFN‐alpha 2b was used with a good rate of success[9]. Also a resolution can be achieved with topical ⅠFN‐alpha 2b after MMC treatment[6].Ⅰn the present patient, complete resolution was not achieved after MMC treatment or an additional 3mo of ⅠFN‐alpha 2b eyedrops. An intact immune system is presumably necessary to achieve a good response to topical ⅠFN‐alpha 2b in treatment of OSSN[4].
Ashkenazyet al[4]described three immunocompromised patients with ⅠFN‐alpha 2b‐resistant OSSN. Among these patients, one had low‐grade follicular Β cell‐lymphoma treated with rituximab, one had untreated chronic leukemia, and one had multiple myeloma treated with lenalidomide. OSSN lesions in the first two patients were resolved with 5‐FU. The OSSN lesion in the third patient was partially resolved by 5‐FU treatment, followed by MMC treatment for complete resolution. The different systemic treatments in these three patients presumably exclude the influence regarding response to ⅠFN‐alpha 2b.
Follicular lymphoma is typically a slow‐growing, indolent lymphoma; however, some follicular lymphomas can grow rapidly. The average age of patients with this lymphoma is approximately 60y; this lymphoma typically arises in many lymphatic areas of the body, as well as in the bone marrow. Ⅰt constitutes the second most frequent non‐Hodgkin lymphoma(after diffuse large Β‐cell lymphoma), and represents the most common low‐grade mature Β‐cell lymphoma in Western countries. CD20 constitutes a therapeutic target for non‐Hodgkinʼs lymphoma; anti‐CD20 antibodies cause the depletion of circulating Β lymphocytes. Rituximab is currently the gold standard anti‐CD20 antibody drug[10].However, patients may experience relapse after administration of rituximab. Obinutuzumab represents a new generation of anti‐CD20 monoclonal antibodies, which facilitate optimized antibody‐dependent cellular cytotoxicity and antibody‐dependent cellular phagocytosis[10]. Β lymphocyte functions include antigen presentation and T cell costimulation, as well as generation of memory T responses, modulation of dendritic cell function, modulation of Th1/Th2 polarization,and secretion of multiple cytokines and chemokines[5]. The immunosuppression caused by lymphoma, and/or alteration of the immune response caused by the depletion of Β lymphocytes (due to obinutuzumab treatment) may explain the poor response to topical ⅠFN‐alpha 2b in patients with a lymphoproliferative disease who exhibit OSSN.
The main limitation of this study was the difficulty involved in identifying and reporting multiple patients with lymphoproliferative diseases who exhibit OSSN. Further studies with new cases in immunocompromised patients are necessary to understand whether in most OSSN cases are resistant to ⅠFN alpha 2b. Our observations are consistent with the findings in three previous cases[4], in addition to suggesting that anti‐CD20 antibody treatment could have influenced the poor OSSN response. We agree with Ashkenazyet al[4]that a patient with a lymphoproliferative disease who exhibits OSSN must be able to adhere to the strict treatment regimen required for a successful outcome; otherwise, surgical excision is preferable to the use of ⅠFN‐alpha 2b. Technologies such as metagenomics could help in the future to establish that patients may be sensitive or resistant to topical ⅠFN‐alpha 2b in OSSN associated with lymphoproliferative diseases.
ACKNOWLEDGEMENTS
We thank Doctor Vilardell of the Department of Pathology,Arnau University Hospital of Vilanova from Lleida for the histological study of this case.
Conflicts of Interest:Huerva V,None;Vilaltella M,None.
 International Journal of Ophthalmology2021年7期
International Journal of Ophthalmology2021年7期
- International Journal of Ophthalmology的其它文章
- Evaluation of preoperative dry eye in people undergoing corneal refractive surgery to correct myopia
- Therapeutic difference between orbital decompression and glucocorticoids administration as the first-line treatment for dysthyroid optic neuropathy: a systematic review
- lnhibition of TGF-β2-induced migration and epithelialmesenchymal transition in ARPE-19 by sulforaphane
- lnhibitory effects of safranal on laser-induced choroidal neovascularization and human choroidal microvascular endothelial cells and related pathways analyzed with transcriptome sequencing
- Effect of vision loss on plasticity of the head and neck proprioception
- Congenital ocular counter-roll: a review of cases treated exclusively by ophthalmologists
