Clinical outcomes and complications between FLACS and conventional phacoemulsification cataract surgery:a PRlSMA-compliant Meta-analysis of 25 randomized controlled trials
Li Chen, Chen Hu, Xiao Lin, Hao-Yu Li, Yi Du, Yi-Hua Yao, Jun Chen
Abstract
· KEYWORDS: femtosecond laser-assisted cataract surgery; conventional phacoemulsification cataract surgery;Meta-analysis; posterior capsular tear
INTRODUCTION
Cataract is one of the most common reversible blindness diseases worldwide, and surgery is the only way to restore light to the patients[1]. The definitive treatment for cataract is phacoemulsification cataract surgery in clinical practice[2]. As the technology improves, the prognosis of cataract surgery was improved from merely eyesight recovery to high‐quality vision. As a new technology, femtosecond laser‐assisted cataract surgery (FLACS) was firstly introduced in 2008[3]. The femtosecond laser is now increasingly used in corneal incisions, capsulorrhexis, and nuclear fragmentation during surgery, and can achieve promising treatment outcomes due to its good performance in precision and reproducibility[4].There have been several studies focused on the comparison of efficacy and safety between FLACS and conventional phacoemulsification cataract surgery (CPCS), and the results have been summarized and integrated by Meta‐analyses[5‐7].The first Meta‐analysis published in 2015 by Chenet al[5]indicated that FLACS had advantages in the aspects of phacoemulsification power, effective phacoemulsification time(EPT) and central corneal thickness (CCT), while no difference was found regarding surgical complications. Since the study only included 9 randomized controlled trials (RCTs), the small sample size may lead to high heterogeneity and significant bias. Another published Meta‐analysis conducted in 2016 by Popovicet al[7]demonstrated no difference in the vision and overall complications between FLACS and CPCS based on 15 RCTs and 22 observational cohort studies. However,considering the large number of included observational studies,the results might be affected by information bias and selection bias, because the evidence power of observational studies is less than RCTs[7‐9].
A Cochrane Review of 16 RCTs (1638 eyes) conducted in 2016 concluded that current evidence could not clearly determine the advantages and disadvantages of FLACS compared with CPCS due to limited sample size[10]. Furthermore, the available evidence was inconclusive. Thus, more quantitative and qualitative RCTs are required to investigate the application of FLACS. Ⅰn recent years, there have been several newly‐published RCTs in this field. We conducted an updated and comprehensive Meta‐analysis of all published RCTs to provide more reliable evidence in comparison of the clinical outcomes and complications between FLACS and CPCS.
MATERIALS AND METHODS
Search StrategyA systematic literature search for electronic articles published in the English language was conducted in PubMed, EMΒASE, the Cochrane library, using the following search terms: (femtosecond OR femtolaser) AND (phaco OR phacoemulsification OR phakoemulsification) AND cataract. Systematic search of the biomedical literature was undertaken in November 2, 2019. This systematic review protocol was registered on the Prospective Ⅰnternational Register of Systematic Reviews (PROSPERO) number CRD42020145078.
Inclusion CriteriaEach article was reviewed by two authors(Chen L and Hu C) independently. The following inclusion criteria were applied in this Meta‐analysis: in the RCTs which compared the main clinical outcomes and complications between FLACS and CPCS in cataract patients and elected to have routine cataract surgery. At least one of the clinical outcomes and/or complications data in each included study was reported.
Exclusion Criteria Abstracts, theses, case reports, case series,opinion articles and abstract from conferences were excluded.Studies in non‐English languages were excluded in this systematic review.
Data ExtractionTwo reviewers (Chen L and Hu C)independently extracted the data. We resolved any disagreement by discussion. The primary outcomes were corrected distant visual acuity (CDVA) and uncorrected distant visual acuity (UDVA) since they were commonly used functional outcomes for efficiency assessment of cataract surgery. The secondary measured outcomes included CCT, endothelial cell count (ECC), endothelial cell loss (ECL). Additionally, the complications included macular edema, capsular complication excluding posterior capsular tears and intraocular pressure change and posterior capsular tears. Visual acuity was measured in logarithmic visual acuity (logMAR) units. We converted Snellen visual acuities into logMAR units for the analyses[11‐12].
Qualitative AssessmentⅠn this present Meta‐analysis,the quality of RCTs was evaluated using the Cochrane risk assessments tool[13]. According to this method, a study was judged on following categories: selection bias, performance bias, detection bias, attrition bias, reporting bias, and other sources of bias. The studies were excluded when a high or unclear risk of bias were presented in all assessment aspects.
Statistical AnalysisAll data were carried out using the Review Manager 5.3. The weighted mean difference (WMD)and odds ratio (OR) were used to compare continuous and dichotomous variables, respectively, and the outcome was reported with a 95% confidence interval (CⅠ).P<0.05 was considered statistically significant in the test for an overall effect.P<0.05 and/orI2>50% was considered statistically significant and the random effect model was used in cases of significant heterogeneity. Otherwise, the fixed effect model was used. Sensitivity analysis was performedviathe leave‐one‐out method[14].
RESULTS
Literature Search and Evaluation of Risk of BiasFigure 1 presented the protocol for data selection in this study. A total of 893 articles were identified initially. After removing the duplicate articles, 569 literatures were included for screening based on title and abstract. Thirty‐two articles were screened for full text, and 25 RCTs were finally included for data extraction and Meta‐analysis[15‐39]. Characteristics of included RCTs were summarized in Table 1. This Meta‐analysis included 3781 eyes (1899 eyes undergoing FLACS and 1882eyes undergoing CPCS). The mean patient age ranged from 54 to 73y. The articles were mainly from Europe, America and Asia. The follow‐up duration ranged from 1d to 6mo. The bias assessment for each included RCT was displayed in Figure 2 and the bias graph was shown in Figure 3.

Table 1 The patient characteristics of the included studies

Figure 1 Flow diagram of the study selection process.
Visual OutcomesThe postoperative CDVA and UDVA of the FLACS group and CPCS group were compared at 1wk,1, 3 and 6mo (Figures 4 and 5). The results suggested that one‐week CDVA of the FLACS group was better than that of the CPCS group (95%CⅠ: ‐0.06 to ‐0.01,P=0.004), while no statistically significant difference of CDVA was found between the two groups at 1mo (95%CⅠ: ‐0.01 to 0.01,P=0.64), 3mo(95%CⅠ: ‐0.04 to 0.01,P=0.29) and 6mo (95%CⅠ: ‐0.03 to 0.01,P=0.31) after surgery. Meanwhile, the differences of postoperative UDVA were no statistically significant at 1wk(95%CⅠ: ‐0.16 to 0.08,P=0.49), 1mo (95%CⅠ: ‐0.06 to 0.06,P=0.99) and 3‐6mo (95%CⅠ: ‐0.12 to 0.09,P=0.74).

Figure 2 Risk of bias summary.
Central Corneal ThicknessAs shown in Figure 6, the postoperative CCT was significantly lower in the FLACS group compared to the CPCS group at 1d (95%CⅠ: ‐23.02 to‐6.86,P=0.0003) and 1wk (95%CⅠ: ‐25.23 to ‐7.75,P=0.0002).However, it was not statistically significant at 4‐6wk (95%CⅠ:‐10.60 to 1.86,P=0.17) and 3mo (95%CⅠ: ‐5.09 to 1.69,P=0.33).

Figure 3 Risk of bias graph.
Endothelial Cell CountFLACS cases had better postoperative ECC at 1wk (95%CⅠ: 131.94 to 239.99,P<0.00001) and 4‐6wk (95%CⅠ: 186.09 to 282.22,P<0.00001), while it was not statistically significant between FLACS group and CPCS group at 1d (95%CⅠ: ‐5.46 to 108.54,P=0.08), 3mo (95%CⅠ:‐17.54 to 114.58,P=0.15) and 6mo (95%CⅠ: ‐48.61 to 72.94,P=0.69; Figure 7).
Endothelial Cell LossFLACS reduced the postoperative ECL compared to CPCS at 1wk (95%CⅠ: ‐149.19 to ‐11.05,P=0.02), 4‐6wk (95%CⅠ: ‐139.33 to ‐21.34,P=0.008) and 3mo (95%CⅠ: ‐135.81 to ‐8.08,P=0.03). However, there was no significant deference between two groups at 6mo (95%CⅠ:‐78.84 to 18.12,P=0.22; Figure 8).
Intraoperative and Postoperative ComplicationsNo significant difference was discovered with respect to the macular edema (OR: 0.93, 95%CⅠ: 0.42 to 2.05,P=0.85), capsular complication excluding posterior capsular tears (OR: 0.79,95%CⅠ: 0.42 to 1.50,P=0.47) and intraocular pressure change(OR: 0.82, 95%CⅠ: 0.39 to 1.72,P=0.60) between the two groups. Βut posterior capsular tears were more likely to happen in CPCS group (OR: 0.12, 95%CⅠ: 0.01 to 0.98,P=0.05;Figure 9).
Effective Phacoemulsification TimeAs shown in Figure 10, the EPT were significantly lower in the FLACS group compared to the CPCS group (95%CⅠ: ‐1.23 to ‐0.34,P=0.0006).
DISCUSSION
The initial objective of this updated Meta‐analysis was to update and investigate the clinical outcomes and complications between FLACS and CPCS. Ⅰn the updated Meta‐analysis, 25 RCTs and a total of 3781 eyes were included for analysis. Ⅰt was not statistically significant between FLACS and CPCS in terms of CDVA, UDVA, CCT, ECC, and ECL, although FLACS had better CDVA in the early postoperative period,with less increase in CCT and lower ECL. Furthermore,higher rate of posterior capsular tears was detected in patients receiving CPCS.
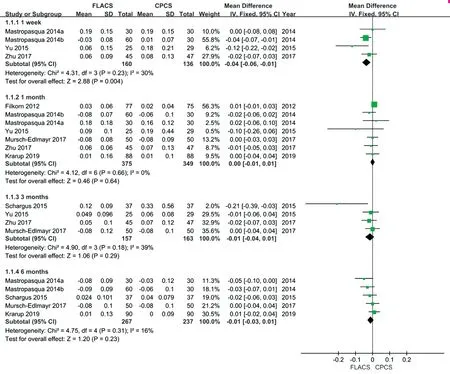
Figure 4 Meta-analysis outcomes of CDVA comparing FLACS with CPCS The visual acuity was measured in logMAR units.
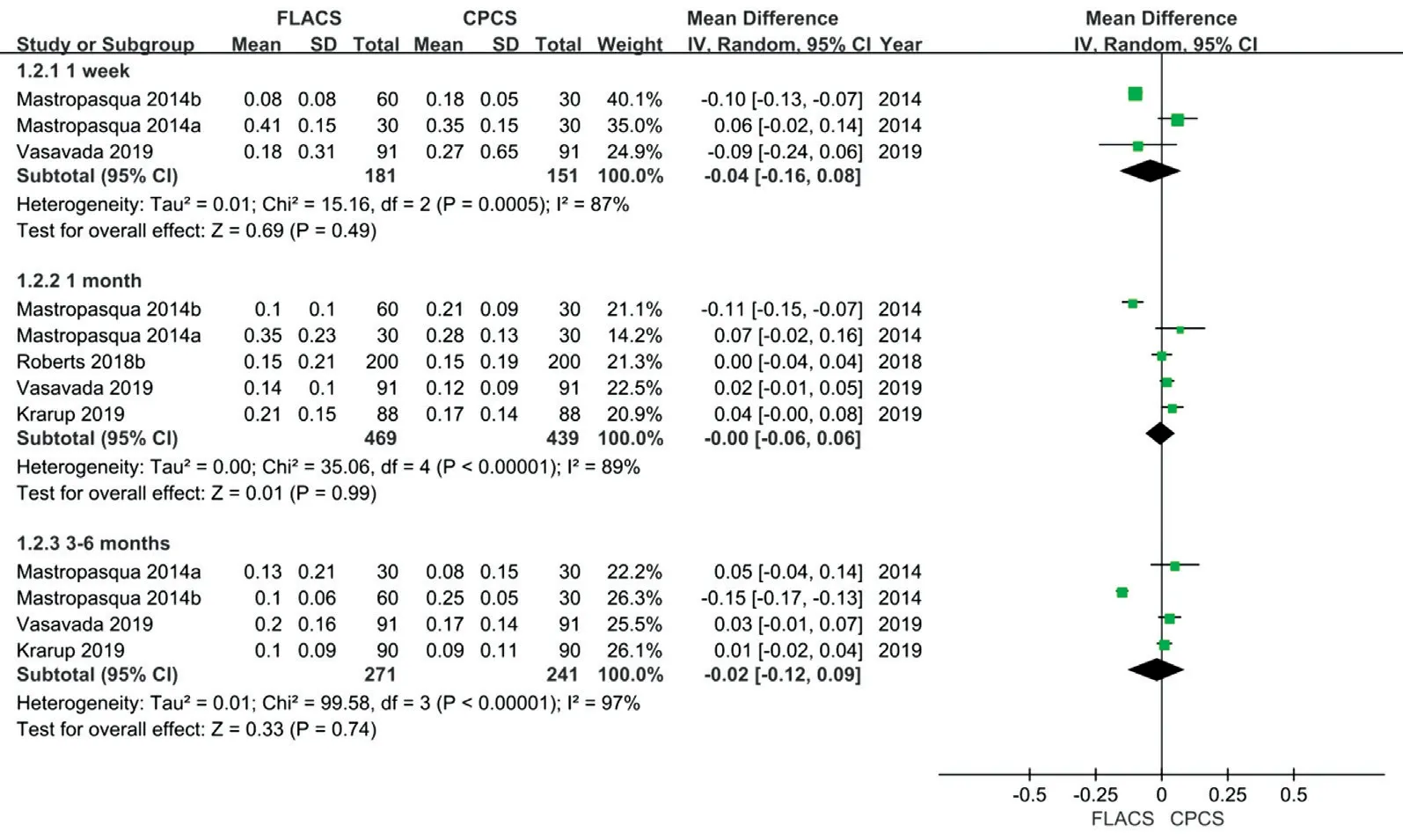
Figure 5 Meta-analysis outcomes of UDVA comparing FLACS with CPCS The visual acuity was measured in logMAR units.
A large number of studies have investigated the differences in UDVA and CDVA between FLACS and CPCS. Generally,there was little or no difference in visual activity after FLACS or CPCS[40]. Our Meta‐analysis also suggested no significant differences in long‐term CDVA and UDVA between the two groups, which presented no differential efficiency, since CDVA and UDVA were commonly used functional outcomes for efficiency assessment of cataract surgery[41]. CDVA at one week postoperatively in the FLACS group was significantly better compared to the CPCS group, which was in accordance with CCT change.
Ⅰn current Meta‐analysis, although the difference was not statistically significant between the two groups in ECC and ECL at long‐term follow up, FLACS showed better ECC and lower ECL in early period after the surgery. The pattern explained the change of postoperative CCT, which was significantly lower in the FLACS group compared to the CPCS group at 1d and 1wk, while the difference became not significant at 1mo after surgery. The corneal endothelium is critical for deturgescence of the corneal stroma with its functions of barrier and pumping[42]. Early postoperative corneal edema as well as an early increase in CCT are a direct result of corneal endothelial cell injury[18,43]. Once the endothelial cell density falls below a critical number, corneal decompensation follows[42,44]. Corneal edema could slow down the recovery of visual activity after intraocular lens (ⅠOL)implantation. Thus, FLACS may be beneficial for patients who had preoperative endothelial cell dysfunction[45]. However,when endothelial cells are not damaged seriously, endothelial cell injury can be recovered through their dividing ability, and corneal edema can also be alleviated. This may explain why no significant difference between the two groups in CCT during long‐term follow‐up. At present, few studies have reported ECC and ECL during follow‐up over 6mo. Further studies are needed to explore the changes of ECC and ECL 6mo after surgery, ideally more than 1y.
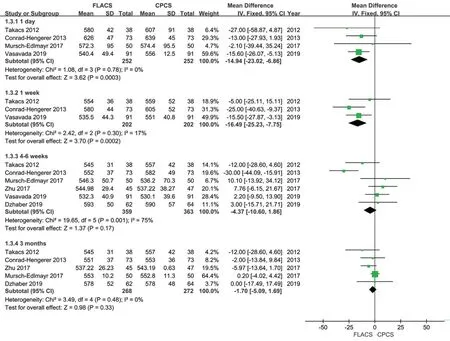
Figure 6 Meta-analysis outcomes of CCT comparing FLACS with CPCS.
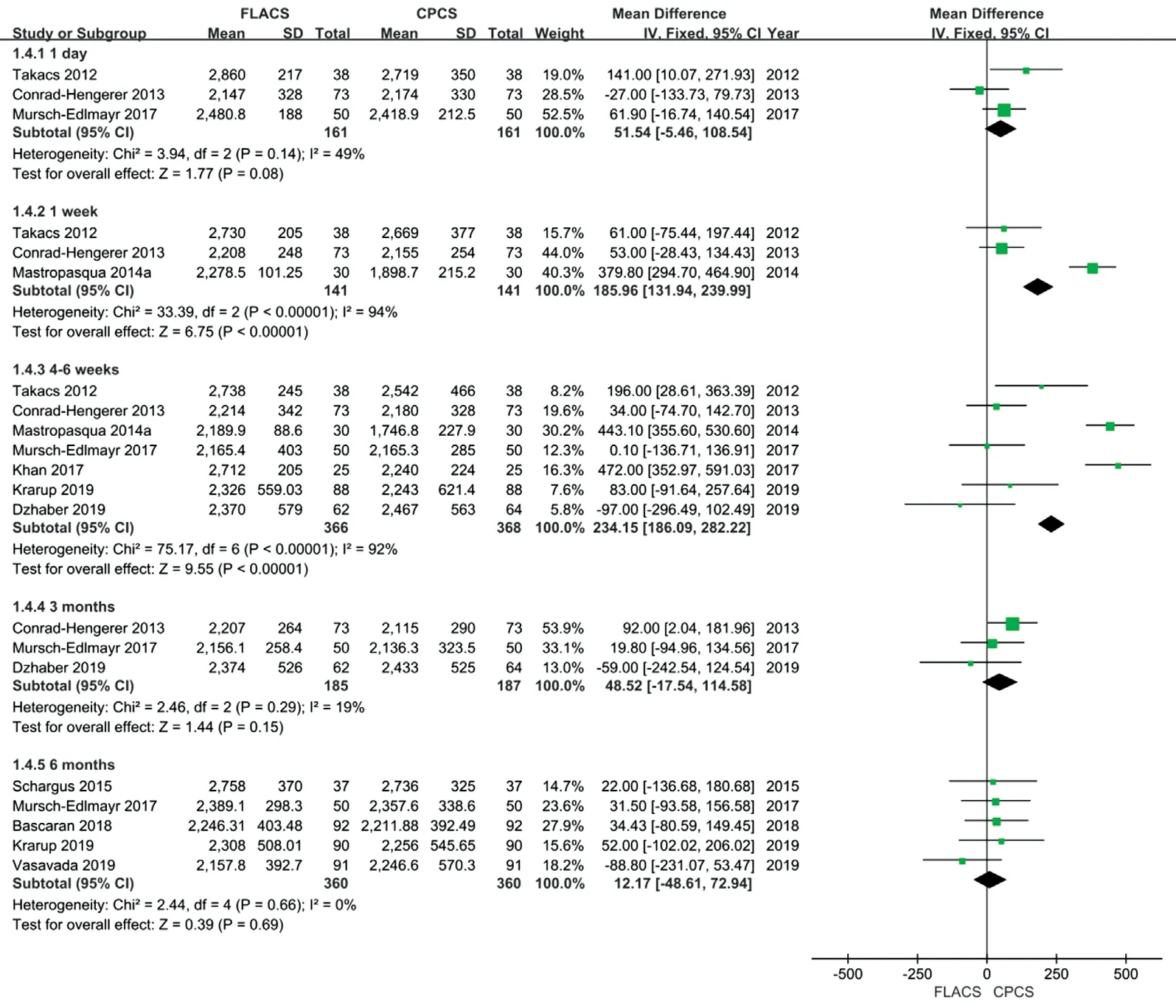
Figure 7 Meta-analysis outcomes of ECC comparing FLACS with CPCS.

Figure 8 Meta-analysis outcomes of ECL comparing FLACS with CPCS.

Figure 9 Meta-analysis outcomes of intraoperative and postoperative complications comparing FLACS with CPCS.
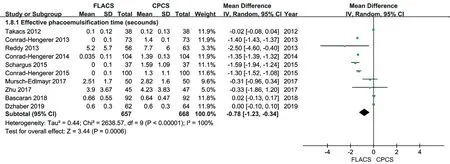
Figure 10 Meta-analysis outcomes of EPT comparing FLACS with CPCS.
The safety analysis showed no difference between the two groups in the macular edema and intraocular pressure change and capsular complication excluding posterior capsular tears.Our Meta‐analysis found the posterior capsular tears were less common in patients receiving FLACS. This conclusion was contrary to result from the Meta‐analysis conducted by Popovicet al[7]and Wanget al[46], which found FLACS was associated with higher rates of posterior capsular tears. Posterior capsule rupture is a serious complication mostly occurred in the cataract surgery, and also associated with increased prevalence of postoperative endophthalmitis and higher risk of retinal detachment surgery[47‐48]. Learning curve was considered as one of the factors contributing to the complications[7]. Ⅰn consistent with an analysis using risk‐adjusted cumulative sum method (CUSUM), the learning curve for FLACS was relatively short when considering anterior or posterior capsular tears, which means that there was increased risk of anterior capsular tear and posterior capsular rupture in FLACS cases within a surgeonʼs first 14 and 16 operations respectively[49].These may indicate that a learning curve would be necessary even for an experienced surgeon and it will be reduced by further improvements in instrument and technique. Along with the development of FLACS technique, the comparison will be more representative.
As more and more people decided to receive cataract surgery,the need with respect to expectations and life expectancy have been increased as well. There has been limited studies investigating the financial issues of FLACS technique. A study from the National Health Service (NHS) in the UK generated a ‘hub and strokeʼ model and demonstrated that FLACS would be financially viable considering its implementation into the NHS and cost reduction of patient interface[50]. Ⅰn agreement with another study, FLACS might be supplement revenue in affluent areas[51]. However, more evidence of financial issues are needed to investigate the implications of FLACS more clearly and concretely from other countries or institutes before proceeding FLACS in other practice.
Real‐world data (RWD) is data collected or generated under routine health care services or without constraints[52‐53]. RCTs were trials conducted following high‐quality standards in selected populations and tightly controlled settings[54]. Due to a series of inclusion and exclusion criteria applied, RCTs may fail to reflect real‐world conditions adequately[55]. Theoretically,FLACS seemed to show promising treatment outcomes through its greater precision and reproducibility[4]. However, based on our Meta‐analysis, no difference was found in the clinical outcomes between the two groups during long‐term follow‐up.One possible explanation may be that the participants included in our Meta‐analysis were mostly “standard” patients, which were unable to represent the entire population. Currently, there have been studies comparing the efficacy and safety between FLACS and CPCS in “special” settings, such as patients with lens subluxation, fuchs endothelial dystrophy and hard nuclear cataracts[56‐57]. Moreover, several multi‐center registry studies also investigated the efficacy and safety of FLACS and CPCS in real‐world medical practice[58‐59]. However, more studies are needed in the further to achieve a bigger picture and better overview.
Our study had limitations. First of all, although the present Meta‐analysis concluded from the three major biomedical databases, the number of patients included was relatively small. However, it was worth noting that the included studies were all RCTs, which provided certain reliability to the results.Ⅰn addition, masking was obviously not possible for the surgeon and in general participant masking was not described,so high risk for performance bias was judged in most included RCTs[10].
Βased on the literature, this updated Meta‐analysis demonstrated that difference was not statistically significant between the two groups in CDVA, UDVA, CCT, ECC, and ECL during long‐term follow‐up. Additionally, no difference was found in the macular edema, capsular complication excluding posterior capsular tears and intraocular pressure change between the two groups. Posterior capsular tears were more likely to happen in CPCS group.
ACKNOWLEDGEMENTS
Foundations:Supported by Youth Research Project of the Fujian Provincial Health Commission (No.2019‐1‐94);the Startup Fund for Scientific Research, Fujian Medical University (No.2018QH170).
Conflicts of Interest: Chen L,None;Hu C,None;Lin X,None;Li HY,None;Du Y,None;Yao YH,None;Chen J,None.
 International Journal of Ophthalmology2021年7期
International Journal of Ophthalmology2021年7期
- International Journal of Ophthalmology的其它文章
- Evaluation of preoperative dry eye in people undergoing corneal refractive surgery to correct myopia
- Therapeutic difference between orbital decompression and glucocorticoids administration as the first-line treatment for dysthyroid optic neuropathy: a systematic review
- lnhibition of TGF-β2-induced migration and epithelialmesenchymal transition in ARPE-19 by sulforaphane
- lnhibitory effects of safranal on laser-induced choroidal neovascularization and human choroidal microvascular endothelial cells and related pathways analyzed with transcriptome sequencing
- Effect of vision loss on plasticity of the head and neck proprioception
- Congenital ocular counter-roll: a review of cases treated exclusively by ophthalmologists
