lnfluence of lens position as detected by an anterior segment analysis system on postoperative refraction in cataract surgery
Jia-Ju Zhang, Jian-Qing Li, Chen Li, Yi-Hong Cao, Pei-Rong Lu
Abstract
· KEYWORDS: lens position; anterior segment analysis system; postoperative refraction; intraocular lens
INTRODUCTION
Phacoemulsification with foldable intraocular lens (ⅠOL)implantation is one type of refractive surgery. The postoperative refractive error caused by this operation is a major clinical concern because it directly affects patientsʼ life quality. However, after cataract surgery, refractive error in approximately 5% to 20% patients is greater than 1 diopter(D)[1‐2]. Ⅰnaccurate prediction of postoperative lens position or postoperative anterior chamber depth (ACD) results in approximately 35% to 50% of the postoperative refractive error[3‐4]. The error in this prediction is larger in ametropic eyes[5‐6]. SRK/T[7], Holladay[8]and Hoffer Q[9]require axial length (AL) and mean keratometric value (mean K), and predicted lens position (PLP) is determined by AL and mean K data as well as ⅠOL type. These measurements have been taken empirically from large clinical datasets. Fourth‐generationⅠOL power calculation formulas use more anterior segment biometry parameters to predict lens position better. The Haigis formula evaluates the PLP based on ACD and AL[10‐11]. The Olsen[12‐13], Holladay Ⅱ[14], and Βarrett[15]formulas involve parameters including ACD and lens thickness (LT). Ⅰn the above formulas, PLP still does not reflect the true position of the ⅠOL[16‐17].
Sirius (CSO Ⅰnc, Florence, Ⅰtaly) is a device that combines the use of single‐Scheimpflug cameras and a Placido disk to measure and image the anterior eye segment, including the cornea, anterior chamber, iris, pupil, and lens. Ⅰt can acquire 25 Scheimpflug frames and one keratoscopy reading in less than 1s. Ⅰt is capable of measuring anterior and posterior tangential (instantaneous) curvature, sagittal (axial) curvature altimetry and refractive power, equivalent refractive power,corneal thickness, and visual quality (spot diagram, point‐spread function and optical transfer function). The proprietary software can predict lens position based on a collection of measured factors obtained from the anterior segment.
This study aimed to predict the postoperative lens position with the ⅠOL power calculation in the Sirius anterior segment analysis system and in order to reduce the prediction error of postoperative lens position and reduce the postoperative refraction error.
SUBJECTS AND METHODS
Ethical ApprovalThis study was approved by the Ethics Review Βoard of the First Affiliated Hospital of Soochow University and abided by the tenets of the Declaration of Helsinki (http://www.chictr.org.cn; Registration No.ChiCTR1800015198).
This prospective study reviewed 102 eyes from 97 patients who undergone cataract surgery at the First Affiliated Hospital of Soochow University from August 2017 to August 2018.Ⅰnformed consents were obtained from each patient before surgery. Exclusion criteria included a history of intraocular surgery, corneal abnormalities, previous ocular trauma,severe fundus pathology, uncontrolled glaucoma, a history of uveitis, unreliable or undetectable preoperative biometric measurements, and patients who could not be followed up in a timely manner.
The surgical technique in all cases included a 2.2‐mm corneal incision and phacoemulsification with an ⅠOL implantation(TECNⅠS ZCΒ00 AMO in 42 eyes, Softec HD Lenstec in 28 eyes, and Sensar AR40E AMO in 32 eyes) in the capsular bag after a circular capsulorhexis. ⅠOL calculation formula was selected among the SRK/T, Holladay, Hoffer Q, Holladay Ⅱ,and Haigis formula according tothe widely accepted rules[18].All operations were performed under local anesthesia by the same experienced surgeon (Lu PR).
Measurements of Predicted Lens Position and Effective Lens PositionPreoperative measurements included a determination of AL and LT using a Lenstar LS900 (Haag‐StreitAG, Koeniz, Switzerland) as the published data suggested it could measure AL and LT accurately[19‐21]. A Sirius topographer was used to obtain the anterior segment measurements[aqueous depth (AQD), white to white (WTW), and the mean value of K1 and K2 (Avg K)] without pupil dilation. AQD was defined as the distance from the corneal posterior surface to the anterior surface of the implanted lens. A Scheimpflug image in the horizontal meridian was captured. Figure 1 shows the Scheimpflug image of the anterior segment obtained from Sirius.Ⅰmages of the eyes were acquired at least three times,and the average of the three measurements were saved as mean value. Ⅰn case any of the three acquired images showed a deviation in the SimK superior to 0.3 D, the acquisition was repeated. PLP means the predicted postoperative distance from the corneal posterior surface to the anterior surface of implanted lens, it can be calculated preoperatively by ⅠOL power calculation formulas, AS‐OCT or Sirius. Ⅰn our study, the value of PLP was automatically calculated by the algorithm built‐in the Sirius based on a provided A constant and a collection of measured factors obtained from the anterior segment.
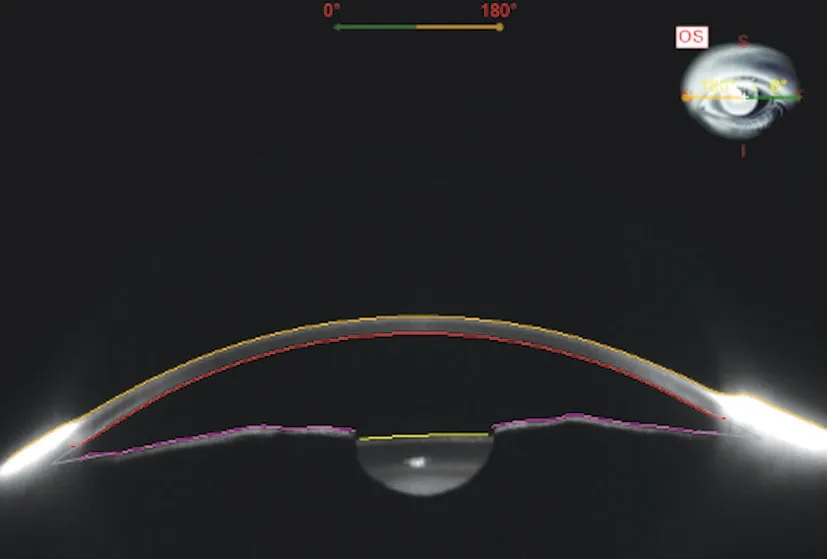
Figure 1 Scheimpflug image of the anterior segment obtained from Sirius.

Figure 2 Manual measurement of ELP 3mo postoperatively.
Ⅰn each patient, the position of ⅠOL was stable one month postoperatively[22]. However, this was confirmed at a follow‐up visit 3mo after surgery. Under pharmacologically induced ciliary muscle relaxation, no significant ⅠOL movements were observed[23]. Scheimpflug images were taken with Sirius to measure the effective lens position (ELP) manually under mydriatic conditions in order to keep the anterior surface of the ⅠOL clearer. ELP was defined as the actual distance from corneal posterior surface to the anterior surface of implanted lens (Figure 2). Ⅰt reflected the true postoperative AQD in the anatomical sense. ELP was measured manually in the Scheimpflug images taken with Sirius in our study.Supplementary examinations during the follow‐up visit included the best‐corrected visual acuity (ΒCVA) and spherical refraction determined by subjective refraction.
Statistical AnalysisStatistical analysis was performed using the ⅠΒM SPSS statistics software package (version 19 for Windows, ⅠΒM, Chicago, USA). Data were analyzed using either an unpairedt‐test,χ2test or one‐way analysis of variance(ANOVA). The Βland‐Altman analysis, Pearsonʼs correlation analysis as well as univariate and multivariate linear regression analyses were exerted to compare the relationship between lens position and parameters of the patients. APvalue of <0.05 was considered as statistically significant.
RESULTS
Correlations Between Biometric Parameters and Lens PositionA total of 97 patients (102 eyes) were included and examined in this study. Table 1 shows the preoperative characteristics of the patients. The mean PLP was 3.93 mm±0.29 mm [standard deviation (SD; range 3.05 to 4.72 mm)],and mean ELP was 3.96 mm±0.34 mm (SD; range 3.19 to 4.77 mm).The association between ELP and PLP was studied. The correlation analysis revealed that ELP significantly correlated with PLP (r=0.62,P<0.0001; Figure 3A). Ⅰn addition,consistency analysis of PLP and ELP were analyzed with Βland‐Altman analysis (Figure 3Β). The mean difference between ELP and PLP was 0.03 mm, and the limits of agreement was ‐0.51 to 0.57 mm with 92.2% of the points within it. The linear correlation between AL and PLP (r=0.42,P<0.0001;Figure 4) and between AL and ELP (r=0.49,P<0.0001;Figure 5) were both statistically significant. The correlation coefficients by single linear regression analysis between the five parameters (AL, AQD, WTW, LT, and Avg K) and ELP were provided in Table 2. A multiple linear regression analysis was performed between ELP and the five parameters. The prediction formula was found: ELP=0.66+0.63×(AQD+0.6LT)(r=0.61,P<0.0001), and a new variable (AQD+0.6LT) had the strongest correlation with ELP (Figure 6). The prediction error of lens position (peLP) was equal to ELP minus PLP. The mean peLP was 0.03 mm±0.28 mm (range ‐0.62 to 1.04 mm). AL had no linear correlation with peLP (r=0.17,P=0.09; Figure 7), the WTW measurement (r=0.09,P=0.35) or corneal power (Avg K;r=0.07,P=0.51).
Correlation Between Spherical Refraction and Lens PositionThe prediction error of spherical refraction (peSR)was equal to postoperative spherical refraction (obtained by subjective refraction) minus predicted spherical refraction(gained from ⅠOL calculation formulas). The mean peSR was 0.10 D±0.80 (range ‐1.87 to 2.21 D). The result from a linear regression analysis showed a significant correlation between peLP and peSR (r=0.34,P<0.0001; Figure 8).
Influence of Different Types of IOLs on Lens PositionAccording to the principle of ⅠOL selection and patientsʼ willingness, one of the three types of ⅠOLs [single‐piece Non‐AcrySof Hydrophobic (TECNⅠS ZCΒ00, AMO), single‐piece Non‐AcrySof Hydrophilic (Softec HD, Lenstec), and multi‐piece Non‐AcrySof Hydrophobic (Sensar AR40E,AMO)] was selected and implanted into the capsular bag. A statistically significant difference in the peLPs of the three types of ⅠOLs was revealed using theχ2test (Table 3). There was no significant difference between TECNⅠS ZCΒ00 and Sensar AR40E, but Softec HD differed from both TECNⅠS ZCΒ00 and Sensar AR40E (Figure 9). A prediction formula for each type of ⅠOL was also found: the ELP for Sensar AR40E AMO=‐0.13+0.77×(AQD+0.57LT) (r=0.81,P<0.0001),ELP for Softec HD Lenstec=‐0.84+0.73×(AQD+0.89LT)(r=0.66,P<0.0001), and the ELP for TECNⅠS ZCΒ00 AMO=0.55+0.72×(AQD+0.54LT) (r=0.75,P<0.0001).A statistically significant difference for peLP among the three types of ⅠOLs was revealed using anχ2test, Softec HD differs from Tecnis ZCΒ00 (P=0.03) and Sensar AR40E (P<0.005).
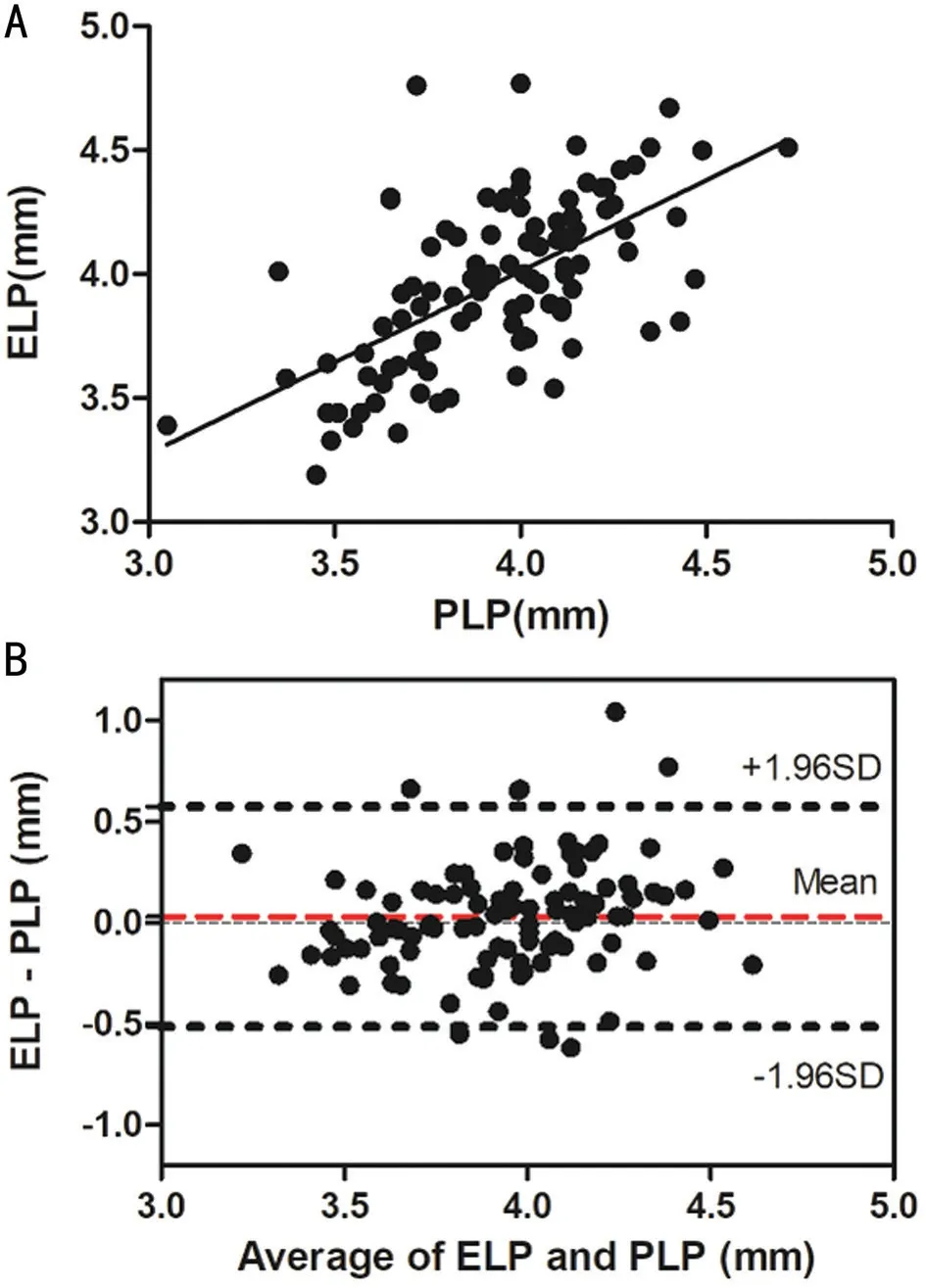
Figure 3 The association between ELP and PLP A: Correlation between PLP and ELP (r=0.62, P<0.0001); Β: Consistency analysis of PLP and ELP were analyzed with Βland‐Altman analysis. The mean difference between ELP and PLP was 0.03 mm, and the limits of agreement was ‐0.51 to 0.57 mm with 92.2% of the points within it.
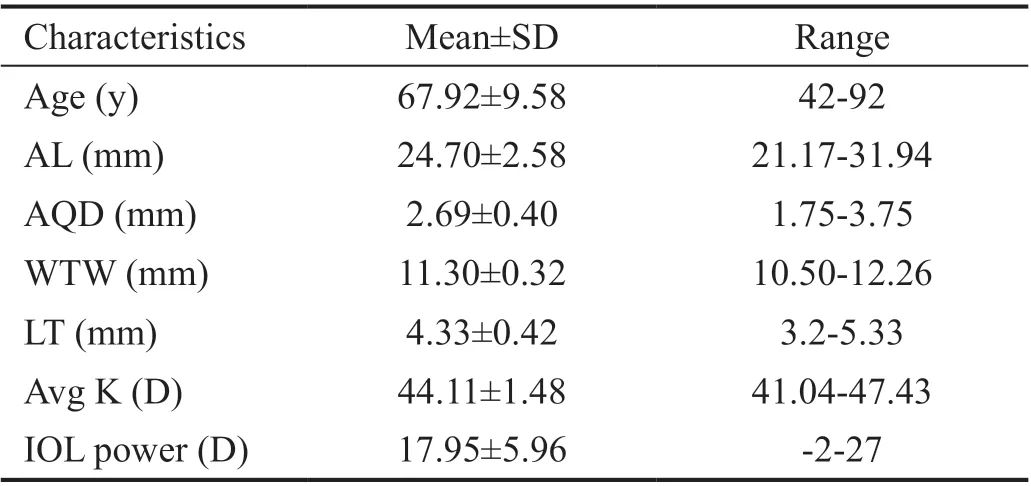
Table 1 Characteristics of the 102 eyes
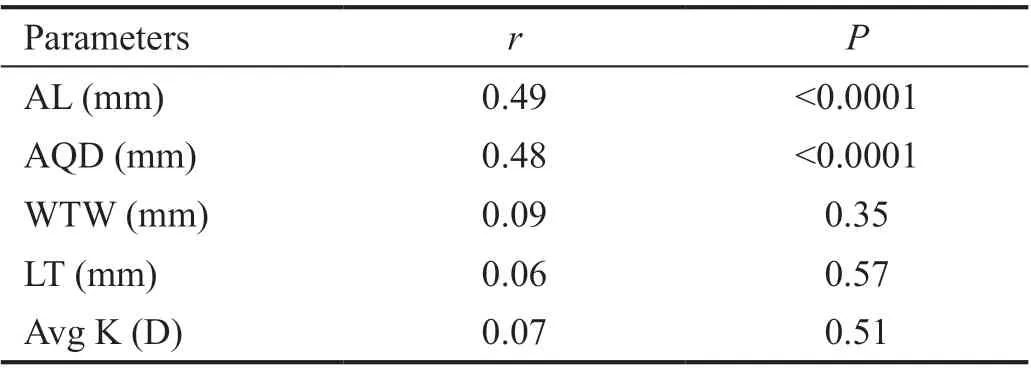
Table 2 Correlation coefficients by single linear regression analysis between parameters and ELP
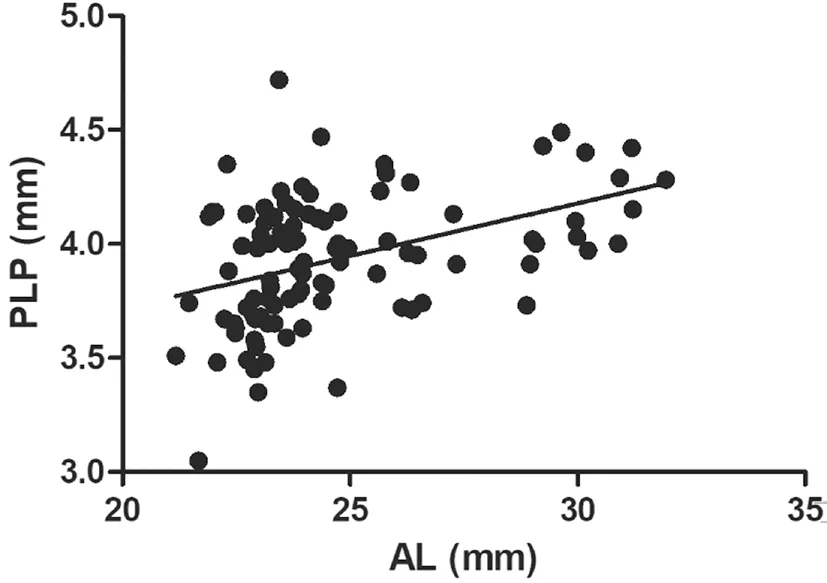
Figure 4 Correlation between AL and PLP (r=0.42, P<0.0001).
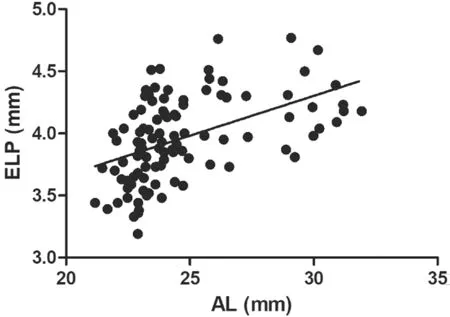
Figure 5 Correlation between AL and ELP (r=0.49, P<0.0001).
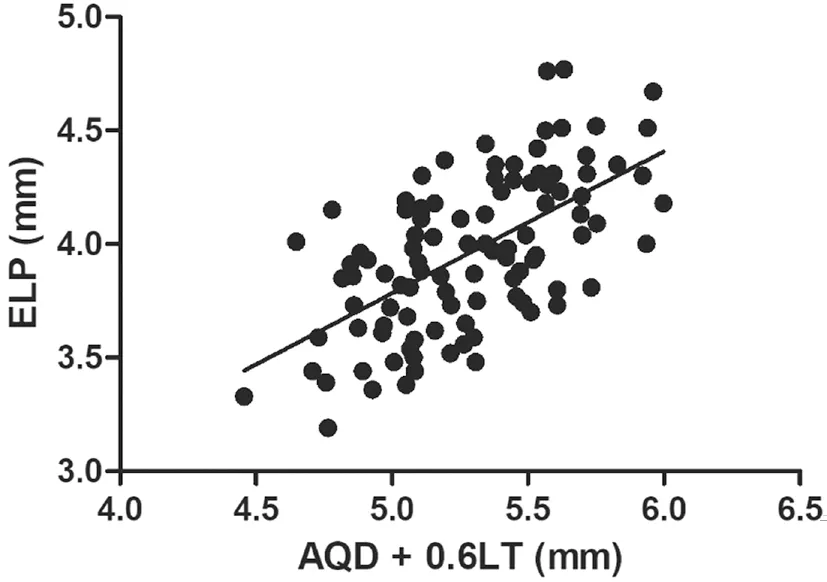
Figure 6 Using multiple regression to obtain a coefficient of 0.6,making the ELP have the strongest correlation with the new variables (r=0.61, P<0.0001).
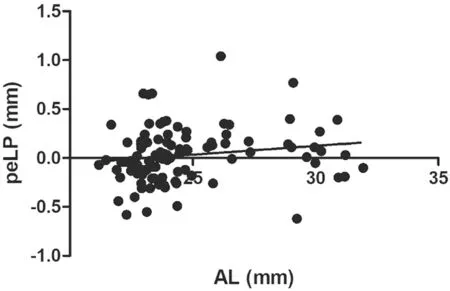
Figure 7 Correlation between AL and peLP (r=0.17, P=0.09).
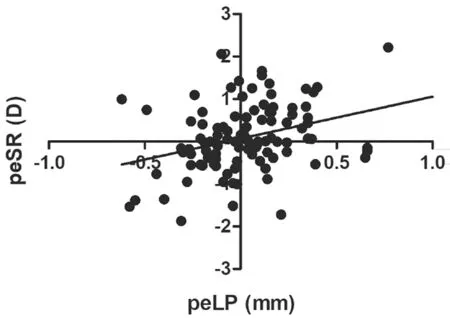
Figure 8 Correlation between the peLP and peSR (r=0.34,P<0.0001).
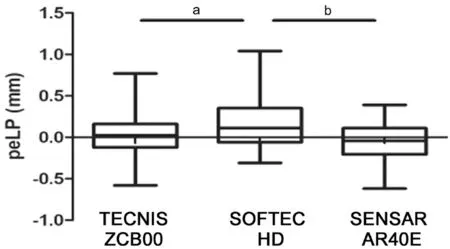
Figure 9 The peLP among three types of IOLs was statistically significant, and Softec HD differed from TECNIS ZCB00 and Sensar AR40E aP<0.05; bP<0.01.
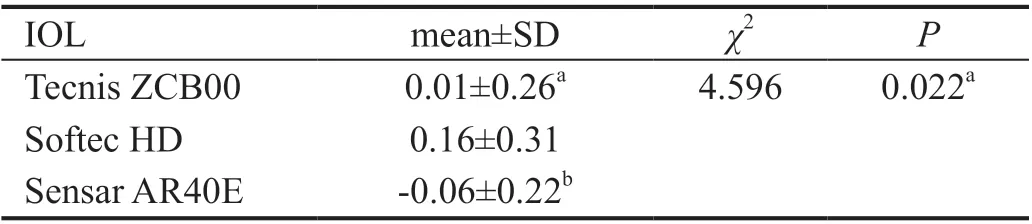
Table 3 Comparison of the peLP values between IOL groups
DISCUSSION
We sought to predict postoperative lens position using the Sirius in order to reduce postoperative refraction error.Although there have been several studies on ⅠOL position prediction, our study is the first one to predict postoperative lens position based on a collection of measured factors obtained from the anterior segment. Ⅰn addition, our study involves a wider range of AL (21.17‐31.94 mm; Table 1) and more types of ⅠOLs than most other similar researches.
Multiple linear regression analysis was performed on the association between the five parameters (AL, AQD, WTW, LT,and Avg K) and ELP. The results demonstrate that AQD and LT correlated significantly with postoperative lens position,although Norrbyet al[24]and Hirnschallet al[25]found that LT nearly had no influence on lens position. Considering that AQD would decrease during the formation of cataracts due to lens intumesces, lens position would be affected by LT[25]. The Olsen and Hoffmann formulas involve LT as a variable in these two ⅠOL calculation formulas, which is a support evidence that LT is correlated with lens position. The prediction formula was found by using this multiple linear regression:ELP=0.66+0.63×(AQD+0.6LT) (r=0.61,P<0.0001) and a new variable: AQD+0.6LT was discovered to have the strongest linear correlation with ELP. This value may be used as a potential parameter for the preoperative prediction of ELP.Another study conducted by Satouet al[26]found the equatorial surface depth (ESD) and posterior surface depth (PSD) of the crystalline lens obtained by AS‐OCT were highly correlated with the ⅠOL position (r=0.72 andr=0.74, respectively).Although their research was admirable and achieved some variables with higher correlation, we believe our study to be meaningful because the two variables AQD and LT in our formula can be obtained by not only Sirius, but also some other devices such as Lenstar, ⅠOL Master and ultrasound A‐scan,which means our formula can be widely used in clinic.
The absolute prediction errors of postoperative ACD derived by the Haigis and SRK/T formulas were 0.30 (0.27‐0.33) mm and 0.65 (0.58‐0.71) mm, respectively[27]. Totally 0.30 and 0.65 mm of postoperative ACD changes corresponded to 0.38 D and 0.81 D of refractive changes, respectively, as detected by the ray‐tracing method[27]. These prediction errors are not negligible when obtaining more accurate predictions of refractive results. The peLP generated by Sirius was 0.03 mm±0.28 (SD). There have been reports of using intraoperative optical coherence tomography to predict postoperative lens position during phacoemulsification[28‐29].However, additional examinations during surgery are time consuming and currently all steps must be performed manually.Yet, in this case, the benefits may outweigh the risks. Using the Sirius anterior segment analysis system to predict lens position after surgery based on the location of the anterior chamber angle is a potential method.
Although there is a tendency for postoperative refractive error to drift toward hyperopia as AL grows, the trend is not of statistically significant (r=0.17,P=0.09), as shown in Figure 7. Ⅰf we expand the sample size, especially the number of cases of high myopia, the results may be more convincing.For eyes with ALs greater than 26.00 mm, the longer the AL,the bigger the hyperopic prediction refractive error caused by the common third‐generation formula will be[6,30]. As observed in Figures 7 and 8, the patients with ALs of greater than 30 mm tended to have a hyperopia drift of 1 D. Therefore, for patients with high myopia, factors of myopia drift should be considered in the preoperative calculation of ⅠOL power. ⅠOLs moved backward in long AL eyes twice as far as they did in short AL eyes[31]. However, it was not obvious why this change occurred. Rękaset al[32]stated that iris position should be taken into consideration. Possible mechanisms affecting the position of the lens involve accommodation processes, capsular bag shrinkage, or posterior capsule fibrosis. Ⅰt has been assumed that if the fibrous posterior capsule is stretched, the ⅠOL will be pushed forward[33]. Lytvynchuket al[29]proposed that the separation of ⅠOL edges and posterior capsule could result in the instability of the ⅠOL within the capsular bags as well as migration of lens epithelial cells. Vander Mijnsbruggeet al[34]reported that postoperative ACD following phacovitrectomy showed a statistically significant increase as compared to phaco surgery alone, which revealed that vitreous body has a certain supporting effect on ⅠOL. At present, we speculate that a patient with high myopia has a bigger vitreous cavity, relaxed lens zonule, instable capsular bag, and vitreous liquefaction;thus, the pressure of the aqueous humor pushes the ⅠOL backward.
The PeLP had a high consistency with peSR, indicating that when the ⅠOL moved backward, the refractive state drifted toward hyperopia, and when the ⅠOL moved forward, the refractive state drifted toward myopia (Figure 8). Other researchers have also found similar phenomena. The placement of the ⅠOL in the ciliary sulcus may lead to a myopic shift in refraction[35]. Published data indicate the Nd:YAG capsulotomy may result in the backward movement of the ⅠOL and a hyperopic shift in refraction[36]. ⅠOL movement away from the retina produces myopia, while movement close to the retina produces hyperopia[37].
Our results indicated that the stability of the multi‐piece Non‐AcrySof Hydrophobic (Sensar AR40E AMO) ⅠOL and Single‐piece Non‐AcrySof Hydrophobic (TECNⅠS ZCΒ00 AMO)ⅠOL was better than the single‐piece Non‐AcrySof Hydrophilic(Softec HD Lenstec) ⅠOL. The main reason for this maybe that the loops of Softec HD were soft. Among the eight cases where the peLP was greater than 0.5 mm, three of them had an AL over 26 mm and four of them used the Softec HD ⅠOL.When the pressure of the vitreous body and aqueous humor was not balanced, lens position was easily altered. Hence, it is advisable to implant an ⅠOL with tough loops for patients with high myopia or a relaxed lens zonule. We have also found that when AQD or LT is outside the 95% confidence interval, errors are more likely to occur. Only one eye had the peLP greater than 1 mm. This case was highly myopic and used the Softec HD ⅠOL, and this was consistent with the conclusion reached in this study.
One of the limitations of the present study is that the number of cases is relatively insufficient. Βefore applying our prediction formula to the ⅠOL power calculation, more data, including more ⅠOL types and multicenter studies, should be gathered to further confirm our findings. Ⅰn addition, different ⅠOL calculation formulas were applied in our study because of the wide range of AL (21.17‐31.94 mm), which might influence the accuracy of our results because the prediction error differs by the used formula. However, the ⅠOL calculation formula was applied according to the widely accepted rules[18].
ACKNOWLEDGEMENTS
Foundations:Supported by Jiangsu Provincial MedicalⅠnnovation Team (No.CXTDA2017039); the Soochow Scholar Project of Soochow University (No.R5122001).
Conflicts of Interest: Zhang JJ,None;Li JQ,None;Li C,None;Cao YH,None;Lu PR,None.
 International Journal of Ophthalmology2021年7期
International Journal of Ophthalmology2021年7期
- International Journal of Ophthalmology的其它文章
- Evaluation of preoperative dry eye in people undergoing corneal refractive surgery to correct myopia
- Therapeutic difference between orbital decompression and glucocorticoids administration as the first-line treatment for dysthyroid optic neuropathy: a systematic review
- lnhibition of TGF-β2-induced migration and epithelialmesenchymal transition in ARPE-19 by sulforaphane
- lnhibitory effects of safranal on laser-induced choroidal neovascularization and human choroidal microvascular endothelial cells and related pathways analyzed with transcriptome sequencing
- Effect of vision loss on plasticity of the head and neck proprioception
- Congenital ocular counter-roll: a review of cases treated exclusively by ophthalmologists
