Comparison of a 5 F Microtube-Irrigated Ablation Catheter and a General Ablation Catheter in the Treatment of Resistant Hypertension with Renal Denervation
Jun-Qing Go, MD, Hong Zhng, MD , , Ling-Yn Li, MD , Xu Wng, MD , Jin Ye, MD nd Zong-Jun Liu
1 Department of Cardiology, Putuo Hospital, Shanghai University of Traditional Chinese Medicine, 200069 Shanghai, People’ s Republic of China
Abstract Objective: To assess the effectiveness of catheter-based renal denervation for reducing blood pressure in patients with resistant hypertension using a 5 F microtube-irrigated ablation catheter.Methods: Sixty patients with resistant hypertension were divided into two groups: a microtube-irrigated ablation catheter group and a general ablation catheter group.We conducted 12-month follow-up of all patients and recorded clinical blood pressure, ambulatory blood pressure, medication use, and biochemistry test results in both groups at the baseline and at the 12-month follow-up.Results: All patients underwent renal denervation.At the 6-month follow-up, ambulatory blood pressure in the microtube-irrigated ablation catheter group was significantly lower than in the general ablation catheter group (systolic blood pressure 142.0 ± 14.4 mmHg vs.150.8 ± 17.9 mmHg, P = 0.04; diastolic blood pressure 81.2 ± 7.0 mmHg vs.87.6 ± 8.0 mmHg, P = 0.002).At the 12-month follow-up, the between-group difference in ambulatory blood pressure was not statistically significant.At the 12-month follow-up, the number of antihypertensive drugs and diuretics used in the microtube-irrigated ablation catheter group was less than in the general ablation catheter group (P = 0.043).There was no statistical difference between the two groups in the results of biochemistry tests and echocardiography.Conclusion: The microtube-irrigated ablation catheter is more effective in treating hypertension than the general ablation catheter at the 6-month follow up and thus fewer antihypertensive drugs were used in the microtube-irrigated ablation catheter group than in the general ablation catheter group.
Keywords: Renal denervation; sympathetic nervous system; microtube-irrigated ablation catheter; resistant hypertension
Introduction
Hypertension is a major global public health concern.In recent years, with the impact of various adverse factors, the incidence of hypertension has continued to rise, and the trend of a younger age at diagnosis has become a major concern.Although many antihypertensive drugs are used clinically, in approximately half of hypertensive patients, blood pressure remains above the goal despite the broad availability of effective pharmaceutical agents [1,2].Poor blood pressure control may lead to damage of target organs, such as the heart, brain, and kidney, thereby promoting cardiovascular events[3].Active and effective control of blood pressure is an important part of hypertension treatment.
Sympathetic nervous system overactivation plays a major role in the development of hypertension.Therefore, blocking renal sympathetic nerves and affecting nerve activation can effectively control blood pressure levels [4, 5].Renal sympathetic denervation (RDN) is a new type of interventional therapy that damages renal sympathetic nerves and reduces sympathetic activity to lower blood pressure.A series of RDN-related clinical studies have shown that RDN is an effective treatment for resistant hypertension [6, 7].Although the results of the Symplicity HTN-3 study were disappointing[8], RDN treatment has become a research focus again.The SPYRAL HTN-OFF MED study and the SPYRAL HTN-ON MED study verified the effectiveness and safety of RDN [9, 10].Our research group found that RDN is effective for management of heart failure [11, 12].Researchers believe that the key difference between the failure in the Symplicity HTN-3 study and stage success of the SPYRAL HTN studies may be due to the different ablation catheters and different ablation methods used, so choosing a more effective and safer renal sympathetic nerve ablation catheter plays a vital role in RDN.In this study, 60 patients with resistant hypertension in the Department of Cardiology at Putuo Hospital from 2013 to 2016 were treated with RDN to investigate the effect of a microtubeirrigated ablation catheter on resistant hypertension.
Methods
Study Design
This was a single-center, prospective, randomized,single-blind (patient-blind) clinical trial.Sixty eligible patients were randomly assigned to the microtube-irrigated ablation catheter group (study group) and the general ablation catheter group(control group) (30 patients in each group).
The study was approved by the Ethics Committee of Putuo Hospital, Shanghai University of Traditional Chinese Medicine, China, and was conducted in accordance with the Declaration of Helsinki and good clinical practice guidelines.Written informed consent was obtained from all patients.
Patients
The inclusion criteria were as follows:
1.Male or female, aged 18- 85 years.
2.Have been receiving three or more antihypertensive drugs for at least 4 weeks.
3.Blood pressure of 140/90 mmHg or higher at the time of screening.
The exclusion criteria were as follows:
1.Medical history of renal artery stenosis or evidence of renal artery stenosis on imaging examination.
2.Glomerular filtration rate less than 45 mL/min/1.73 m².
3.Type 1 diabetes mellitus.
4.Substantial stenotic valvular heart disease.
5.Pregnancy or planned pregnancy during the study period.
6.Acute phase of myocardial infarction or cerebrovascular accidents in the past 6 months.
Running Period and Randomization
All eligible patients took amlodipine (5 mg), losartan (50 mg), and hydrochlorothiazide (12.5 mg) for at least 4 weeks.After 4 weeks, the patients were checked for inclusion/exclusion again.Blind codes for randomization were sealed in envelopes and eligible patients were randomly assigned to the study group or control group by sequential opening of the envelopes.
RDN Intervention
The patients were given 300 mg of chewable enteric coated aspirin or 300 mg of clopidogrel and an intravenous injection of unfractionated heparin(6000- 8000 U) before the intervention.The skin in the right inguinal region was prepared and disinfected.A puncture was made in the right femoral artery to insert a 7 F catheter sheath, followed by the insertion of a JR4 catheter for bilateral renal angiography.Then a radiofrequency catheter was inserted for rotational ablation with temperature control.In the general ablation catheter group, we used a 3.5 F Symplicity catheter (Medtronic, 25-40 ° C, 6- 15 W).In the microtube-irrigated ablation catheter group, we used a 5 F microtube-irrigated catheter for cooling (Huida, 40- 48 ° C, 6- 15 W,head diameter 3.5 mm, with 12 small side holes;cold saline perfusion at 2 mL/min during mapping and 12 mL/min during ablation).
The effective ablation time per point was less than 60 s (impedance reduction greater than 10%), and each renal artery contained four to eight ablation points (the distance between neighboring points was 0.5 cm).Renal angiography was performed immediately after the percutaneous operation.
Drug Adjustment Plan
Initial oral antihypertensive drugs were recorded for all patients according to the type and number of conventional antihypertensive drugs.During the follow-up period, it was recommended to add drugs if systolic bold pressure (SBP) was greater than 170 mmHg and/or diastolic blood pressure (DBP) was greater than 100 mmHg; it was advisable to reduce the dose if SBP was less than 100 mmHg and/or DBP was less than 60 mmHg and if the patient had symptoms of hypotension,such as dizziness.
Efficacy
Twenty-four-hour ambulatory blood pressure and office blood pressure were recorded at the 6-month follow-up and the 12-month follow-up.The number of antihypertensive drugs used was recorded at the 12-month follow-up.
Safety
Blood biochemistry tests and echocardiography were performed at follow-up.
Data Analysis
Statistical analysis was performed with IBM SPSS Statistics 22.0.All measurement data are presented as the mean ± standard deviation, and thettest was used for self-control comparison and betweengroup comparison.All counting data are presented as a percentage, and the chi-squared test or Fisher’ s exact test was used for comparison.The level of significance was defined as P < 0.05.
Results
Clinical Features of Patients
From 2013 to 2016, 60 patients were eligible for inclusion in the study and were randomly assigned to the microtube-irrigated ablation catheter or the general ablation catheter group.There was no significant difference between the two groups in clinical condition, medical history, liver and kidney function, other biochemical parameters, and echocardiography results (Table 1).
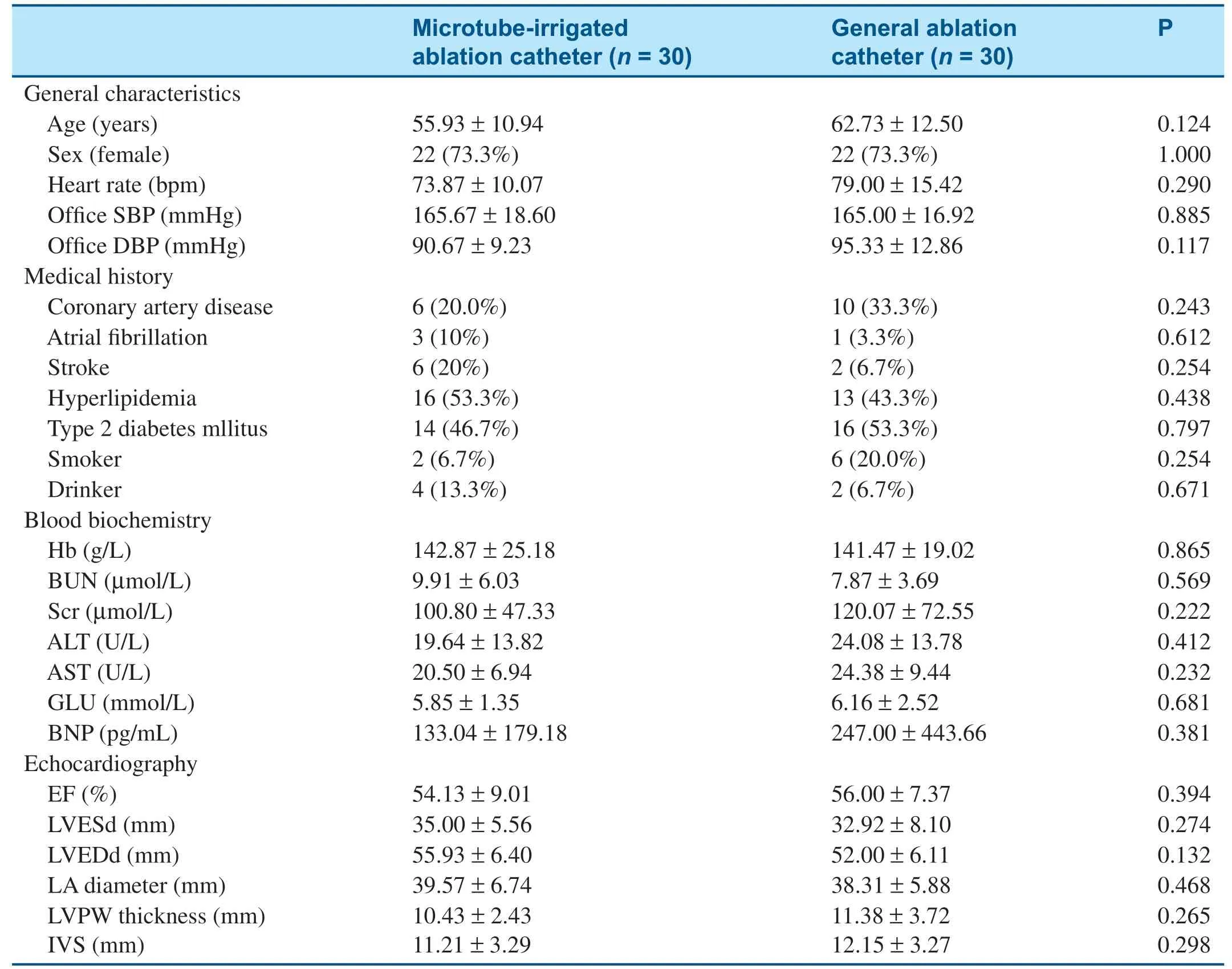
Table 1 Between-Group Comparison of General Characteristics and Echocardiography Results at the Baseline.
Procedural Parameters and Safety
RDN-related parameters are listed in Table 2.Ablation points were comparable between the two groups.There were significant differences in postablation impedance reduction, ablation temperature,and radiofrequency energy between the two groups:the impedance of the microtube-irrigated ablation catheter results in higher energy release, while significantly reducing the temperature during catheter ablation.Angiographic images of both groups did not show postoperative complications such as renal artery dissection and renal artery stenosis occurred(Figure 1).
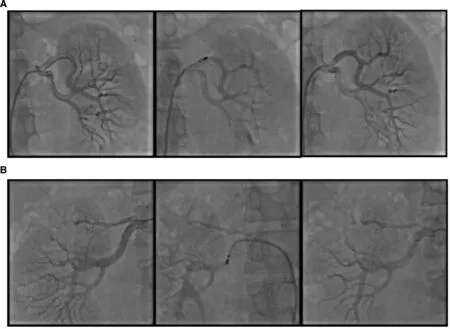
Figure 1 Angiographic Images of Microtube-Irrigated Denervation Catheter Applying Circumferential Ablations in Renal Arteries (A: right; B: left).
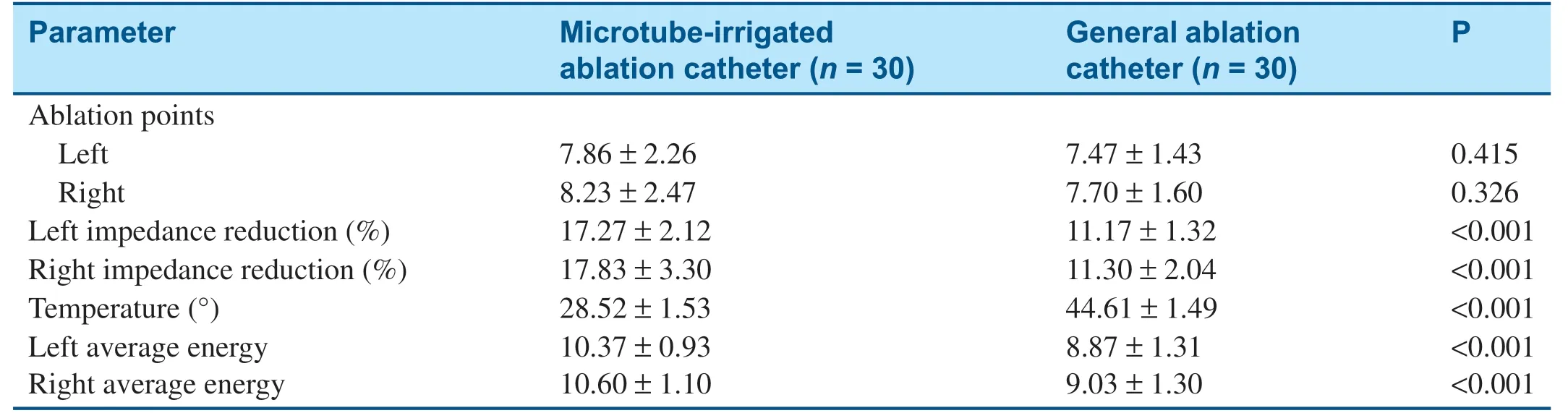
Table 2 Procedural Parameters.
Medication during Follow-up
At the 12-month follow-up visit, the number of antihypertensive drugs used in the microtube-irrigated catheter ablation group was significantly less than in the general catheter ablation group (3.13 ± 1.04 vs.3.73 ± 1.20, P = 0.043; Table 3); particularly,significantly fewer patients (P = 0.004) in the study group (26.7%) were taking thiazide diuretics than in the control group (63.3%).
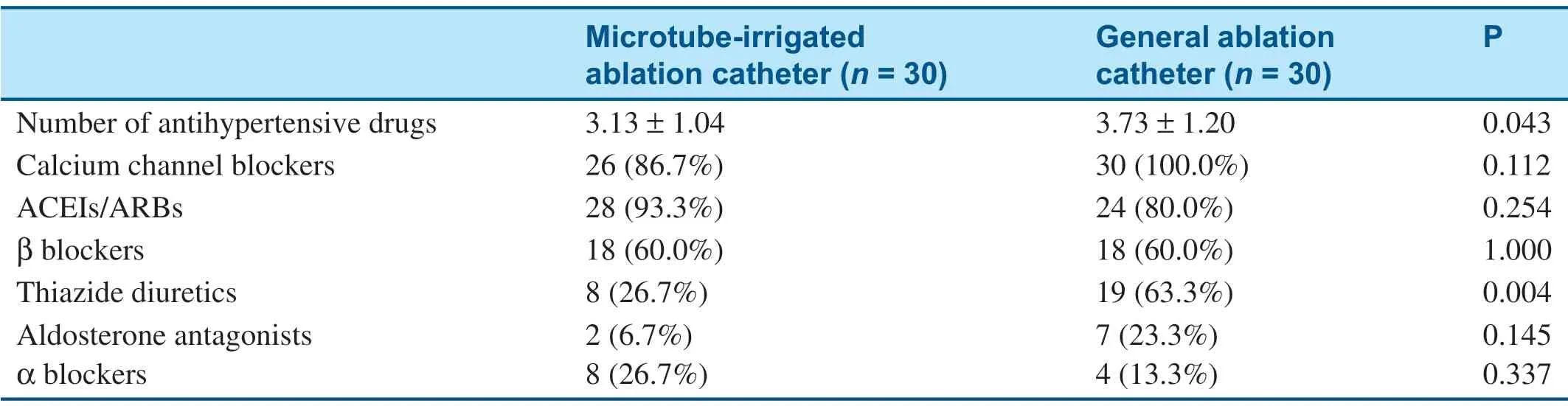
Table 3 Antihypertensive Medications Used at the 12-month Follow-up.
Efficacy
All patients underwent the RDN operation successfully and were followed up at 6 months and 12 months after the intervention.The baseline ambulatory blood pressure was similar between thetwo groups.The 24 h average SBP and DBP in the microtube-irrigated ablation catheter group were significantly lower than in the general ablation catheter group at the 6-month follow up (SBP, P = 0.04,DBP, P = 0.002; Table 4), but the trend disappeared at the 12-month follow-up (SBP, P = 0.102, DBP,P = 0.115; Table 4).The blood pressure change from the baseline was higher in the study group than in the control group (Figure 2).
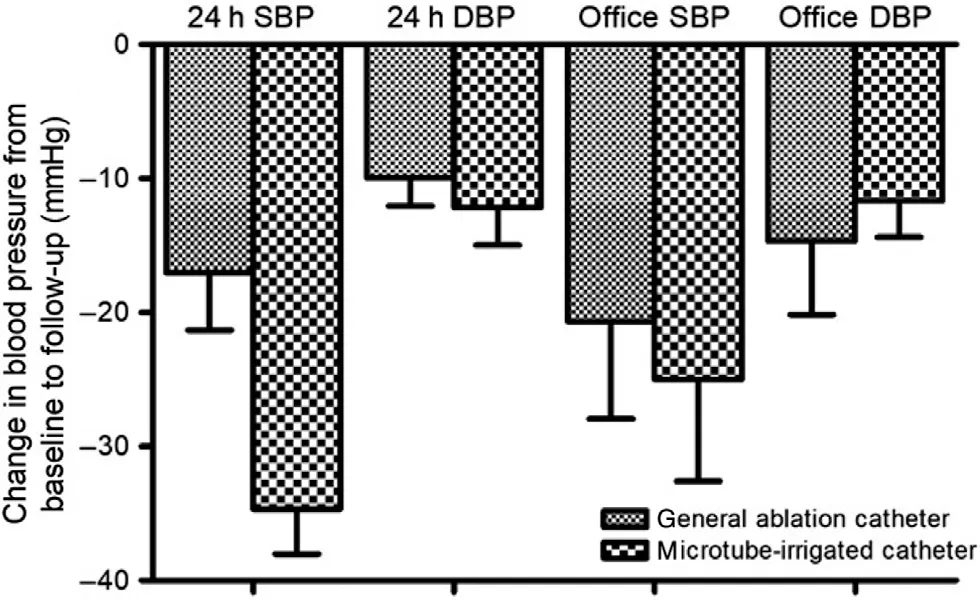
Figure 2 Change at 6-month Follow-up in Office and Ambulatory Systolic Blood Pressure (SBP) and Diastolic Blood Pressure (DBP) for the General Ablation Catheter and the Microtube-Irrigated Catheter.
Safety
Blood biochemistry test results and echocardiography results during the follow-up are shown inTable 5.There was no statistical difference between the two groups.
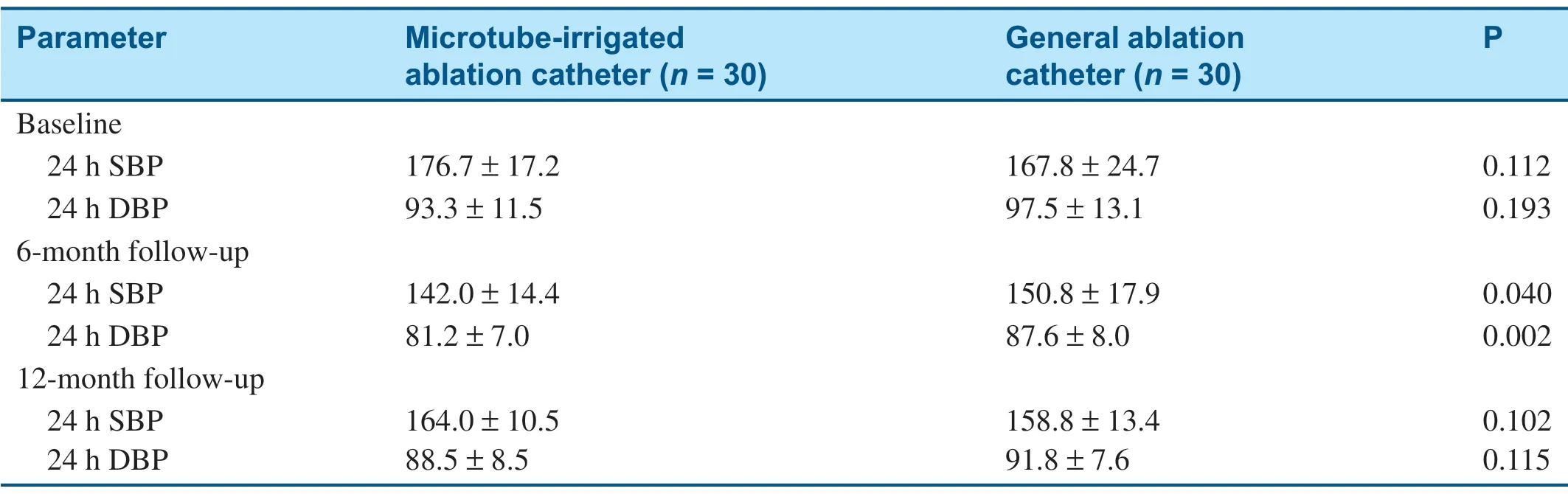
Table 4 Ambulatory Blood Pressure (mmHg) at the Baseline, the 6-month Follow-up, and 12-month Follow-up.
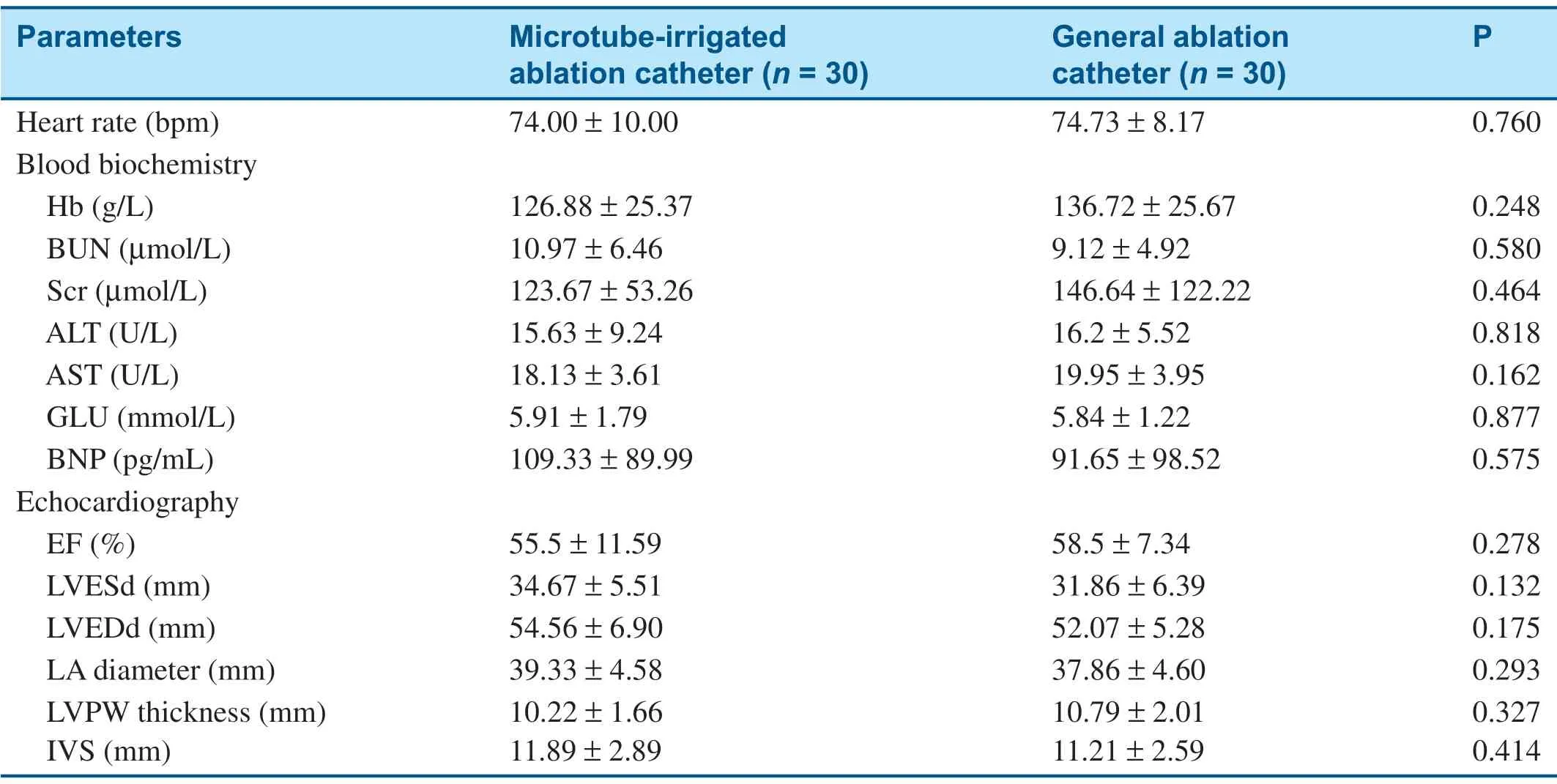
Table 5 Blood Biochemistry and Echocardiography Results at the 12-month Follow-up.
Discussion
Renal sympathetic activity contributes to the development and perpetuation of hypertension.Increased activity can lead to secretion of catecholamines, renin, and other factors that are promoted in the renin-angiotensin-aldosterone system and increase water and sodium retention.Therefore,blocking the renal sympathetic nerve and affecting activation can effectively control blood pressure [13, 14].Expert consensus on the diagnosis and treatment of resistant hypertension in China has noted that patients with uncontrolled essential hypertension despite treatment with four or more antihypertensive drugs (poor treatment adherence)and a high cardiovascular risk may be considered for RDN treatment if they meet the inclusion criteria for RDN [15].
RDN is a minimally invasive technique using an ablation catheter passed via the femoral artery to the bilateral renal arteries to release radiofrequency currents in selected areas to locally heat the renal artery adventitia and block renal sympathetic nerve activity [16], which in turn reduces blood pressure levels.The 2009 Symplicity HTN-1 findings confirm the clinical application, efficacy, and feasibility of RDN surgery [6].Subsequently, Symplicity HTN-2, a multicenter prospective randomized controlled study, further identified the antihypertensive effects of RDN on refractory hypertension [7].In addition, recent clinical studies using various ablation devices, including EnligHTN-1 and REDUCEHTN [17, 18], have shown results similar to those of the Symplicity HTN-1 and HTN-2 studies.However, the results of Symplicity HTN-3 in 2014 were surprising [8].After 6 months of followup, the average SBP was reduced by approximately 14 mmHg in in RDN-treated patients and 12 mmHg in sham-operation patients, with no significant difference between the groups.This result challenged RDN treatment.However, there were some weaknesses in that study, such as the proficiency in surgical operation and ablation of instruments (Our ablation catheter is a microtube-irrigated catheter,and HTN-3 catheter is a non-irrigation catheter.Moreover, our surgery has more ablation pointsthan HTN-3).Therefore, that study had some limitations.The SPYRAL HTN-OFF MED study showed that RDN caused significant changes in blood pressure at 3 months after surgery in non-drug-treated patients with mild to moderate hypertension, demonstrating the effectiveness and safety of RDN [19].Although that study was not targeted at patients with resistant hypertension, it provided new directions and guidance for RDN in conducting research in a wider range of hypertensive patients.
In the present study, we found that at the 6 months follow-up, the 24 h average ambulatory blood pressure in the microtube-irrigated ablation catheter group was lower than in the general ablation catheter group (SBP 142.0 ± 14.4 mmHg vs.150.8 ±17.9 mmHg, P = 0.040; DBP 81.2 ± 7.0 mmHg vs.87.6 ± 8.0 mmHg, P = 0.002; Table 4).These data are similar to data from the HTN-2.But the effect disappeared at the 12 month follow-up.This result suggests that the microtube-irrigated ablation catheter ablates more thoroughly than the traditional catheter for only half a year.In the course of the operation, the average temperature in the microtube-irrigated ablation catheter group was only approximately 28 ° C, whereas the temperature in the general ablation catheter group was 44 ° C.In addition, the microtube-irrigated ablation catheter group had a greater reduction in impedance and more energy released than in the general ablation catheter group, which made the ablation more thorough.In current RDN treatment, general ablation catheters are often used.Compared with the general ablation catheter, the microtube-irrigated ablation catheter was developed to be securer and more effective.In the process of ablation, the microtubeirrigated ablation catheter does not easily cause a thrombus or eschar and ablates tissue more deeply;the temperature at the contact surface is also lower.Because the sympathetic nerve fibers are located deeper in the adventitia of the renal arteries, deeper ablation can damage the nerves more easily and a lower contact surface temperature (intima side of the renal arteries) can protect the intima of the renal arteries, thereby decreasing the risk of injury.Therefore, microtube-irrigated ablation catheters in RDN are more favorable.However, in this study,although the microtube-irrigated ablation catheter achieved better results by the 6-month follow-up,this advantage disappeared by the 12-month followup.Whether this phenomenon is related to sympathetic regeneration or central sympathetic feedback readjustment needs further study.
In addition, there was no significant difference between the two groups in the follow-up ofliver,kidney, and cardiac function, which indicated that the microtube-irrigated ablation catheter is a safe treatment for resistant hypertension.
Conclusion
In summary, the microtube-irrigated ablation catheter is more effective in treating hypertension than the general ablation catheter at the 6-month followup and thus fewer antihypertensive drugs were used in the microtube-irrigated ablation catheter group than in the general ablation catheter group.Further research with more participants and long-term follow-up is needed in the future.
Conflicts of Interest
The authors declare that they have no conflicts of interest in the research.
Funding
Support for this study was provided by the Overseas Program of Shanghai University of Chinese Medicine, the Shanghai Key Medical Specialties Construction Project (ZK2019A11), the Shanghai Health and Family Planning Commission Medical Clinical Special Project (201840247), and the Young Elite Scientists Sponsorship Program by CAST (QNRC2-B03).
 Cardiovascular Innovations and Applications2021年4期
Cardiovascular Innovations and Applications2021年4期
- Cardiovascular Innovations and Applications的其它文章
- Barriers to the Implementation of Primary PCI in the Management of STEMI in Egypt
- Main Renal Artery Plus Branch Ablation in the Treatment of Resistant Hypertension with Renal Denervation
- Clinical Significance of Angiographically Detectable Neovascularity in Patients with Cardiac Myxoma
- ST-Segment Depression in Leads I and aVL:Artifactual or Pathophysiological Findings?
- A Case Report of Radiofrequency Ablation of Typical Atrial Flutter Combined with Atrial Tachycardia
