Comparison of phacoemulsification combined with goniosynechialysis and trabeculectomy in the treatment of APACG
Shui-Feng Deng1, Rui Liao1, Jun-Xia Li1, Dan Dai1, Wen-Tao Li1, Bi-Yu Zhang1, Ling Zhou1, Ye-Hong Zhuo, Ying-Ting Zhu
Abstract
•KEYWORDS: acute primary angle-closure glaucoma; cataracts; phacoemulsification combined with goniosynechialysis; trabeculectomy; quality of life.
INTRODUCTION
Glaucoma as a severe irreversible blinding eye disease must be highlighted as a somatopsychic illness due to its close interactions with mental activities. Particularly for APACG which brings about significant psychological disorders, its rigorous therapeutic evaluations should cover not only disease control after surgery, but amelioration in the quality of life. Surgical therapy such astrabeculectomy and a combination of PPI and GSL is preferred for the disease. However, conventional appraisals usually focus on objective clinical indices incorporating intraocular pressure (IOP), visual field and nerve fiber impairment, omitting impacts of various surgical approaches on postoperative quality of life in APACG patients complicated with cataracts. Recently, evidences have shown that the quality of life has been significantly improved after filtering surgery for glaucoma or phacoemulsification for cataracts[1]as attentions have been paid to such a subjective indice for patients with the severe eye diseases. However, for those with APACG with coexisting early cataracts featuring slight symptoms and favorable visual acuity, there is still a saliently controversial point in the selection of lens extraction or trabeculectomy as the priority intervention[1-3]. Apart from that, there is a dearth of evidence in quality-of-life improvement after the two approaches.
The NEI-VFQ-25 has been widely applied across countries, characterized by high internal consistency as proven by several studies[4-5]. Its Chinese language version can sensitively and accurately evaluate the vision-related quality of life in patients with glaucoma[4-5]. Previous study have confirmed that visual acuity, refractive status and inflammation responses can be stably normalized 3mo after filtering surgeries like trabeculectomy and phacoemulsification surgery[6-7]. In our study, to diminish interference factors during postoperative recovery period, 6mo after surgery has been selected as the postoperative time for observation and evaluations, and items of quality of life in the NEI-VFQ-25, IOP, BCVA in the surgical eye, complications and postoperative review frequency have been assessed at the same time point. Therefore, factors affecting postoperative quality of life resulting from various surgical approaches can be screened out, which underlies a reference for surgical selection as the priority intervention for APACG.
SUBJECTS AND METHODS
SubjectsThis study was approved by the Ethics Institutional of the Huizhou Third People’s Hospital, Guangzhou Medical University (Ethics of the Third Hospital 2018-39). In this perspective, randomized case-control study. APACG patients who met the inclusion criteria and admitted to the Huizhou Third People’s Hospital, Guangzhou Medical University from January 2018 to May 2019 were selected. They were randomly divided into two groups, group A (n=29, excluding one lost to follow-up) and group B (n=30). The basic characteristics were summarized in Table 1. Patients in group A received PPI+GSL surgery and those in group B trabeculectomy combined with peripheral iridectomy. All APACG patients signed informed consent forms, and the preoperative IOPs were mitigated to normal ranges as possible prior to surgeries. The quality of life before and 6mo after surgery was evaluated using the NEI-VFQ-25, and so were basic characteristics encompassing gender, age, education, residential address, profession, marriage, living with family members or not, IOPs, BCVA, the incidence of complications and review frequency.
The inclusion criteria were defined as follows: 1) APACG patients complicated with earlycataracts seriously affecting a single eye with glaucomatous optic neuropathy represented as localized absence of the neural rim or, cup disc ratio of more than 0.3, or asymmetry of cup disc ratio of 0.2; 2) The fellow eye had normal IOP, and accepted the treatment of laser peripheral iridectomy followed by no recurrence or other eye diseases during the follow-up period; 3) Cases with peripheral anterior synechia (PAS) over 180 degrees using gonioscopy preoperatively; 4) With a slight lenticular opacity and BCVA greater than or equal to 0.3 (Intemational Visual Chart) in the affected eye after IOP reduction.
The exclusion criteria were summarized as follows: 1) Patients with severe APACG in both eyes; 2) With secondary angle-closure glaucoma; 3) Those experienced surgeries for eye diseases; 4) Those suffering from other eye diseases except for glaucoma that resulted in visual impairment, such as eye trauma, optic neuritis, uveitis and keratitis.
SURGERY
PreoperativePreparationThe combined medication of myotic agents,β-blockers, carbonic anhydrase (CA) inhibitors and mannitol injection was used for IOP reduction to a normal level in APACG patients with early cataracts preoperatively. Local glucocorticoid application was used for alleviating inflammation responses, and antibiotic eye drops against infections.
PreoperativeExaminationsAll patients underwent routine ophthalmic examinations prior to the surgeries, including BCVA, IOP measurement using a Goldmann applanation tonometer (Keeler, England), PAS using a gonioscopy (OCULAR, America), the assessment of the anterior segment using slit-lamp(Topcon, Japan), fundus oculi observation using a 90 diopter lens (VOLK, America), and assessments of anterior corneal curvature, anterior chamber depth and axial length using ultrasound biomicroscopy (UBM) (SW-3200L, China), ophthalmic A/B ultrasound (SW-2000, China) and IOLMaster (Carl Zeiss, Germany).
ScalesThe NEI-VFQ-25 consists of 11 vision-related domains and one general health rating question. The 11 vision-related subscales included: general vision, difficulty with near and distance activities, driving, difficulties or limitations with peripheral and color vision, ocular pain, social functioning, role limitations, dependency and mental health. A standard algorithm was adopted to calculate the scale scores varying from 0-100, whereby 100 represented the best possible score and 0 the worst. A composite NEI-VFQ 25 score can be generated by averaging scores of the 11 items (except for the general health rating question). Higher scores indicated better visual functions[4-5]. All patients were asked to fill the scale by themselves based on their own health conditions in the last 30d. However, individuals with low educational background could receive assistance from investigators for a neutral explanation until they could completely understand the scale and finish the survey independently. In our study, the included subjects were predominantly rural populations and most of them could not actually drive, which means a low response rate in the item “driving”. As with previous recommendations, this item could be deleted[5].
SurgicalProceduresAll surgeries must be completed by the same surgeon. For PPI+GSL surgery, all affected eyes were routinely dilated with compound tropicamide eye drops 30min before the surgery. A 3.2 mm temporal clear corneal tunnel incision was made after surface anesthesia, followed by a lateral corneal incision above or below it with a viscoelastic agent used to deepen the anterior chamber. The size of continuous curvilinear capsulorhexis (CCC) was about 6 mm. Hydrodissection were performed for phacoemulsification, so was emulsification of the lens nucleus. Splitting irrigation and aspiration was adopted for removing cortex, and the viscoelastic agent was injected in the anterior chamber. A folding monofocal intraocular lens (IOL) was implanted in the pouch. Then the viscoelastic agent was used again for dissecting the chamber angle with the injection near the angle for 360 degrees. Splitting irrigation and aspiration was applied to remove the agent for recreating the anterior chamber, followed by watertight closure and exterior coating with TobraDex eye ointment (Alcon, America). The surgery was completed.
For trabeculectomy, the limbus-based conjunctival flap was prepared, so was the limbus-based trapezoidal scleral flap with a size of 4×3 mm and 1/2 of the thickness of the sclera. The scleral flap was dissected from the sclera to 2 mm medial to the corneal margin. Subsequently, cotton pads immersed by 5-fluorouracil solution (10 mL∶0.25 g, Shanghai Xudonghaipu Pharmaceutical Co., Ltd.) were placed under the conjunctival flap or the scleral flap for 2-4min according to patients’ own conditions, followed by rinsing with ringer’s solution (100 mL). The routine trabeculectomy was performed for the removal of a 1×2 mm flap, followed by iridodialysis and scleral-flap suture. After recreating the anterior chamber, single- or two-sided adjustable suture was performed around the trapezoidal flap, followed by the reposition of conjunctival sac, watertight closure and exterior coating with TobraDex eye ointment (Alcon, America). So the trabeculectomy was finished.
Follow-upDuring the 6-month follow-up, patients receiving PPI+GSL surgery were reviewed at 1wk, 2wk, 1mo, 3mo and 6mo after surgery; and those undergoing trabeculectomy were reviewed once a week in the first month after surgery, once every two weeks in the second months and once a month in the 3-6thmonths. Frequency of follow-up was adjusted according to the health status and recovery route of each patient. BCVA, IOP, complications, intraocular inflammation, and optic neuropathy were routinely examined for each review. For the patients undergoing trabeculectomy, the conjunctival suture and adjustable suture were removed within 2wk after the surgery, and the eyeball was massaged according to the patient’s IOP. The NEI-VFQ 25 scale was completed 6mo after the two approaches. Other clinical characteristics encompassing gender, age, education, residential address, profession, marriage, living with family members or not, were recorded at the same time points.
StatisticalAnalysisData were processed using SPSS 16.0 software. Quantitative data were represented as mean±standard deviation (SD). The paired-samplest-test was adopted to compare the pre- and postoperative BCVA, IOP, and scores of quality of life between the two groups. The two-samplet-test was performed to compare the score of each item and the average score of the scale between group A and group B. Multiple linear regression analysis was used to select correlation factors that relate to the improved average scores. Review frequency and the clinical characteristics in patients was analyzed using Wilcoxon rank-sum test. APvalue of less than 0.05 was considered statistically significant.
RESULTS
There was no significant difference in basic characteristics between the two groups (Table 1), the included subjects were predominantly female rural populations, with a slightly lower education level and high dependence on family members. Besides, no significant intraoperative or postoperative complications occurred in the two groups. After 6-month follow-up, IOPs in both groups were significantly reduced compared with preoperative status. Patients undergoing PPI+GSL surgery presented a significant improvement in BCVA compared to those merely receiving trabeculectomy. Besides, individuals receiving trabeculectomy showed higher review during the period than those accepting PPI+GSL (Table 2).
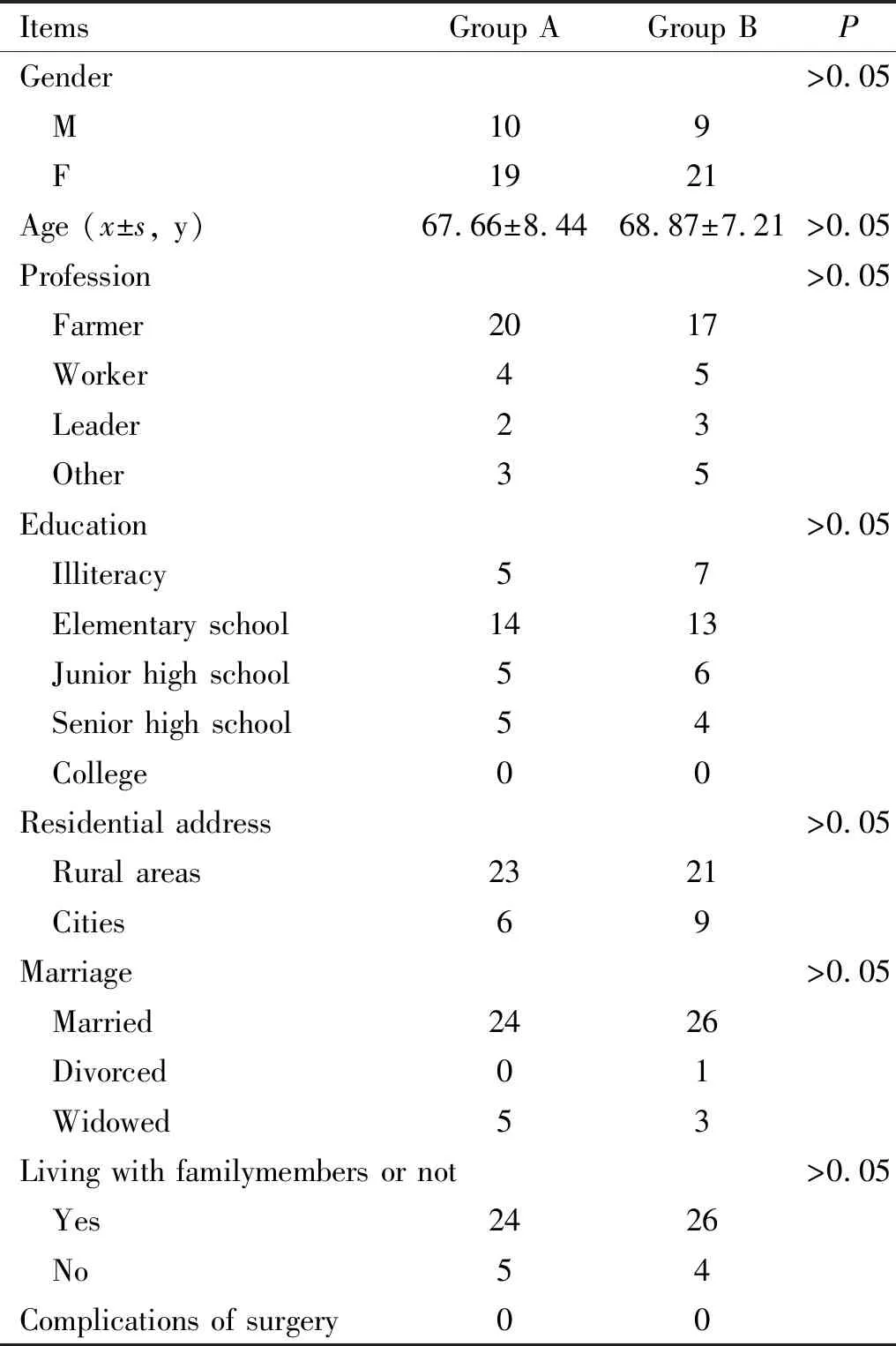
Table 1 The basic characteristics of included patients
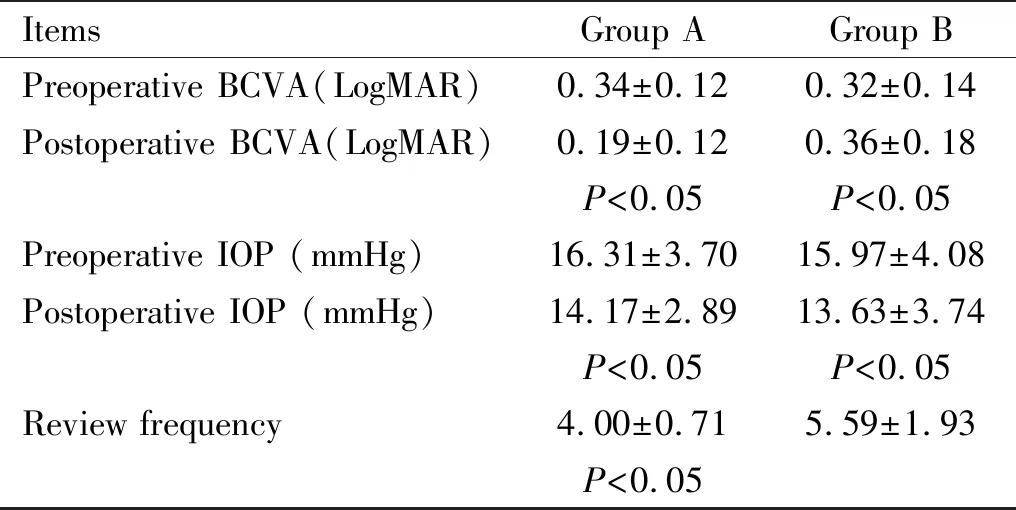
Table 2 Preoperative and postoperative BCVA and IOP, and review frequency in the two groups
There were nonsignificant differences in preoperative average scores of the NEI-VFQ-25 between the two groups (Table 3). Both groups revealed significant increases in postoperative average scores (Table 4). Patients receiving PPI+GSL surgery showed a significant net increase in average scores with a higher degree of quality-of-life improvement than those accepting trabeculectomy (Table 3). And the degree in quality-of-life amelioration was associated with the degree of BCVA recovery and review frequency after surgery. The higher the degree in BCVA improvement was, the lower the postoperative review frequency would be and higher scores in quality of life would be achieved (R2=0.48,F=5.00,P<0.05) (Table 5).
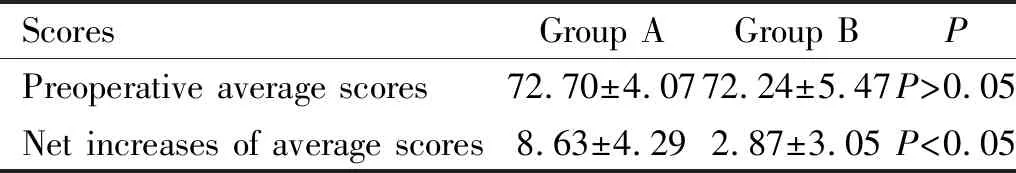
Table 3 Net increases in pre- and postoperative scores on quality of life in the two groups
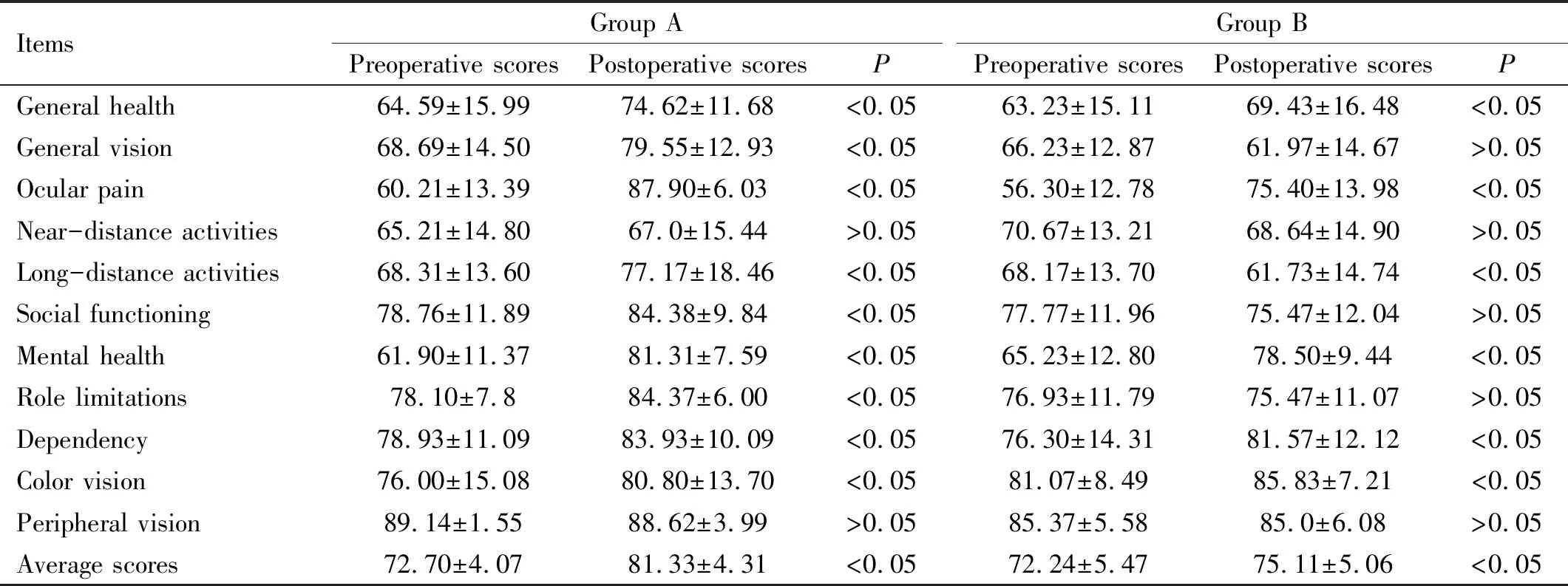
Table 4 Preoperative and postoperative scores on quality of life in the two groups
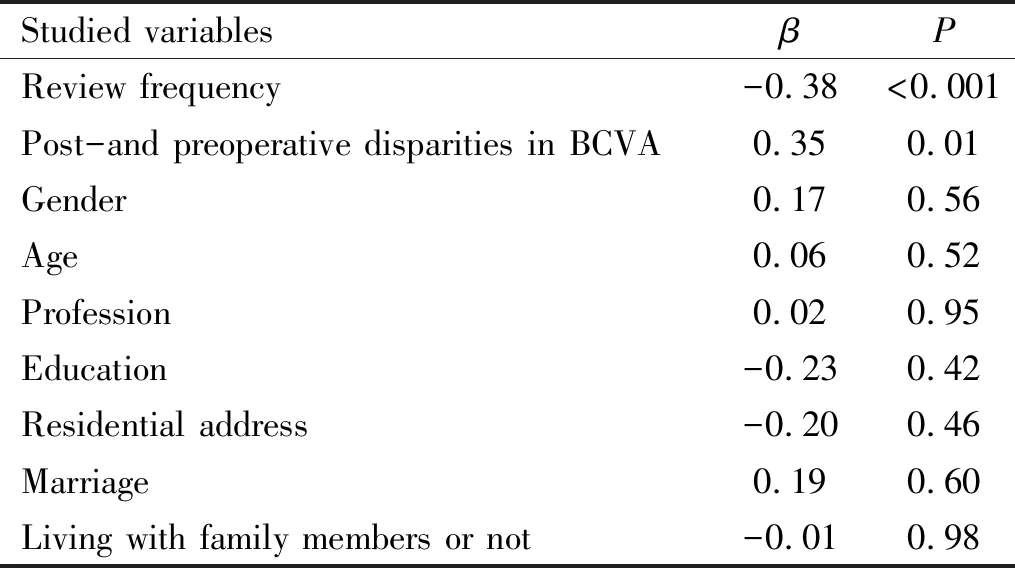
Table 5 Correlation factors affecting the net increases inaverage scores on quality of life after surgery
Group A revealed higher average scores in general health, general vision, ocular pain,long-distance activities, mental health, social functioning, role limitations, dependency and color vision (allP<0.05), but nonsignificant mitigation in near-distance activities and peripheral vision (allP>0.05), than preoperative records. Group B revealed higher average scores in general health, ocular pain, mental health, color vision and dependency (allP<0.05) and a lower average score in postoperative long-distance activities (P<0.05) than preoperative records, but nonsignificant improvement in general vision, near-distance activities, role limitations, social functioning and peripheral vision (allP>0.05) (Table 3). Although the two groups showed various degrees in quality-of-life amelioration, group A achieved greater improvement in ocular pain alleviation than group B (P<0.05). There were nonsignificant differences in the degree in the improvement of mental health, dependency and color visions between the two groups (allP>0.05) (Table 6).
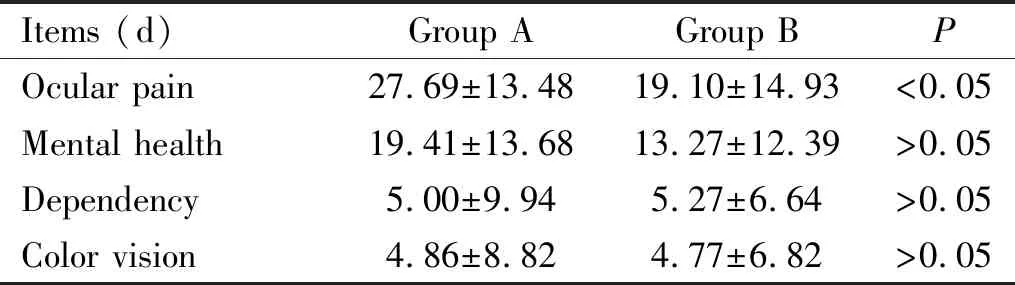
Table 6 Postoperative and preoperative disparities in the score of some item for the quality of life
DISCUSSION
Since surgical therapies are preferred for APACG, efficacy of various approaches and difference clinical indices for the appraisal of successful rates after surgery determine results of research. Though trabeculectomy can significantly reduce IOP with 1-5-year successful rates of 50%-90% in APACG patients[8], PPI+GSL surgery shows superiority in the medium- to long-term efficacy of over 90% for such a disease, even in APACG patients receiving lens removal combined with transparent IOLs implantation can significantly mitigate IOP and deepen the anterior chamber[9-13]. In our study, IOP has been stably normalized in a short period of follow-up in the two groups, without severe intra- and postoperative complications.
Though different approaches can both achieve favorable test results (e.g. significant IOP reduction), patients may not have the same subjective experiences. That means individual disparities in postoperative quality of life. However, there is still a controversial point in the relationship between surgical approaches and amelioration of quality of life. Some studies support improved or the similar quality of life after filtering surgeries compared with the preoperative status[14-15]. However, some believe that filtering surgeries alone may even, on the contrary, decrease the quality of life which can be promoted by combining with cataract surgery[6]. Previous studies also have shown uplifted quality of life after cataract surgery in APACG patients, presenting superiority over laser iridectomy[12,16]. Therefore, integrating objective clinical indices with assessments for patients’ own subjective feelings can comprehensively judge whether the postoperative efficacy has been ameliorated[17].
In our study, patients accepting either PPI+GSL surgery ortrabeculectomy present higher scores of the NEI-VFQ-25 after surgery, indicating facilitated quality of life in the both groups. This finding is supported by previous studies[6,18]. Moreover, individuals receiving PPI+GSL surgery show better quality of life, which is correlated with better BCVA recovery and lower review frequency. Evidences have shown that the poorer the vision function is, the more severe psychological disorders and poorer vision-related quality of life will be[5]. Refractive errors have been partially corrected after cataract extraction by PPI+GSL surgery, bringing about salient d value: postoperative average score-preoperative average score.
amelioration in distance vision, general vision and long-distance activities. However, the limitations of adjustment in near vision still exist as monofocal IOL has been applied in PPI+GSL surgery. Along with the deepened anterior chamber, the position of IOL can be pushed backward, perhaps resulting in hyperopic shift after surgery[19]. Therefore, patients receiving the combined surgery have to wear presbyopic glasses. Otherwise, they may experience difficulty with near-distance activity unless the habit supports it. Patients receiving trabeculectomy can easily suffer from surgically induced astigmatism and the aggravation of cataracts, resulting in poorer visual acuity after surgery[20]. In our study, the patients accepting trabeculectomy did not show significant visual loss and significant differences in general vision, near-distance activities, social functioning and role limitations between pre- and postoperative performances, but show more difficult in postoperative long-distance activities. We speculated that there might be a decrease in visual quality and so on, which affected the distance vision behavior.
We find that frequent medical consultation after surgery has significantly impeded high quality of life in APACG patients with coexisting earlycataracts. This can be explained by their inability to drive a car from rural areas for a medical visit, and their lower educational background may restrict their aspiration to learn the skill but with higher dependency on family members. So there is difficulty in postoperative consultation, and reducing the frequency can significantly improve their quality of life. Previous studies indicate that age, education and lower frequency of eye drop applications are factors that influence quality of life in APACG patients[3,15], but these factors have no obvious significance in our study. Though some unfavorable factors against amelioration in quality of life still exist in group B, the total score has been improved. This suggests that factors that affect postoperative quality of life are intricate.
The APACG patients in the two groups have shown improvements in general health, ocular pain, mental health, dependency and color vision. In addition, their general health and dependency on family members are closely related to disease conditions and their psychological status. In the acute phase, APACG patients often feel severe ocular pain, rainbow vision and headache; alongside plummeted vision, they fear that the possible blindness may put heavy burden on their family members as negative emotions like anxiety and depression suddenly boost[21]. Normalized IOP, improved visual function and alleviated ocular pain as well as stable postoperative efficacy during the 6-month period of follow-up are accompanied by great amelioration in anxiety, depression and dependency on others, with recovery of color vision over time. On top of that, both groups show higher scores in ocular pain after surgery, with higher net increases in group A than that in group B. The undesirable performances in group B may attribute to slight foreign body sensation and mild pain caused by the impairment of tear film, the implantation of filtering blebs and eyeball massage after trabeculectomy[22]. Interestingly, although glaucomatous optic nerve damage were found in the APACG patients, there were nonsignificant differences in peripheral vision between pre- and postoperative scores in the two groups. Evidences have shown that visual field defects can be detected until up to 40% of the retinal nerve fiber layer has been lost. Most APACG patients in other studies also exhibit normal vision 6mo after initial acute onset[23-24]. Due to the short duration of the disease and desirable IOP control after surgery in our study, patients show good visual field preservation with nonsignificant feelings in limitations with peripheral vision. Another reason for the nonsignificant feelings in limitations with peripheral vision may be that patients in our study have lower requirements for peripheral vision.
As the aforesaid passages have clarified, during the short period of follow-up, though the two groups have achieved favorable successful rates of IOP control after surgery, patients complicated with early cataracts receiving PPI+GSL surgery present better quality of life than those accepting trabeculectomy. This can be attributes to a lowered frequency of review and an improved visual function. All this indicates that both objective clinical indices and subjective feelings in quality of life must be considered for comprehensively assessing the therapeutic efficacy of various surgical approaches in APACG complicated with early cataracts.
Besides, some limitations still exist in our study. Firstly, most patients come from rural areas with low education, and the sample size of our trial is small. Secondly, this study only took a subjective quality of life assessment and lacked a detailed objective assessment such as surgical success rate of both groups. Thirdly, the long-term evaluation for postoperative quality of life in APACG patients can easily be affected by nonocular stimuli and systemic diseases. Therefore, we have conducted a short-term evaluation after surgery. However, a large sample size, long-term questionnaire study combined with objective clinical evaluation is expected in the future.
- 国际眼科杂志的其它文章
- An overview on dry eye disease diagnosis: options for new non-invasive testing technologies
- Change of subretinal fluid thickness and choroidal thickness after scleral buckling surgery
- 人翼状胬肉中miR-486-3p的表达及其潜在靶基因的生物信息学分析
- 重组人生长激素对兔角膜损伤早期修复的研究
- 基于SD-OCT建立新的前膜分级法评估IMEM对年龄相关性白内障患者术后视功能的影响
- 氯喹性视网膜病变的监测方法