Study on the antitumor effects of autologous and allogeneic CIK cells in patients with breast cancer*
Xia Chen,Zhijian Dai,Xiangji Lu,Meng Ren,Zhenshan Guo,Yanwei Gao (✉)
1 Department of Apheresis,Inner Mongolia Red Cross Blood Center,Hohhot 010010,China
2 Department of Surgical Oncology,Inner Mongolia People’s Hospital,Hohhot 010017,China
3 Department of General Surgery,Inner Mongolia Armed Police Hospital,Hohhot 010010,China
Abstract Objective This study aimed to compare the anti-tumor effects of cytokine-induced killer (CIK) cells induced by autologous cytokines in patients with breast cancer and those of allogeneic CIK cells from healthy adults.Methods We used conventional methods to induce CIK cells originating from two peripheral blood mononuclear cell types (from patients with breast cancer and healthy adults).Killing activity was detected using an LDH assay,immunophenotypic changes were analyzed by flow cytometry,and the IFN-γ level of culture supernatants was detected by ELISA.Results The results showed that the proliferative capacity of the allogeneic CIK cells was significantly higher than that of the autologous CIK cells.Compared with autologous CIK cells,the allogeneic CIK cells had significantly enhanced anti-tumor activity against SKBR-3 cells (P < 0.01) and IFN-γ secretion (P <0.05);moreover,they increased the ratio of CD3+CD56+cells and CD3+CD8+cells (P < 0.05).Conclusion Healthy adult-derived induced CIK cells exhibited a stronger anti-tumor effect than induced CIK cells derived from patients with breast cancer.The results of this study could provide experimental evidence for the clinical application of CIK cells.
Key words:CIK cells;autologous;allogeneic;cellular immunotherapy;breast cancer
As a new model for treatment following surgery,radiotherapy,and chemotherapy,biological treatment of tumors is gradually being accepted by a majority of patients due to its safety,effectiveness,and low level of side effects.It has been widely used in the treatment of cancer patients on both national and international levels,achieving good results.At the beginning of 2014,Science,an authoritative American magazine,even rated tumor immunotherapy among“the top ten technological breakthroughs in 2013”[1].
CIK cell adoptive immunotherapy is an important method of tumor biotherapy.CIK cells are immunocompetent cells that can be obtained by separating mononuclear cells from peripheral blood,bone marrow,or cord blood and culturing them in the presence of multiple cytokines for a certain period[2,3].At present,the common treatment method in China is to induce CIK cells from the peripheral blood of tumor patients and then reintroduce them into the patient for immunotherapy.Certain studies have revealed that tumor patients have under-functioning immunity and immune cells,which potentially affect the treatment effect.Moreover,it was suggested that the healthy lineal relatives of tumor patients should be considered as treatment cell donors[4].In this study,we compared the antitumor effects of autologous and allogeneic CIK cells in patients with breast cancer to determine the more effective CIK cell adoptive immunotherapy.
Materials and methods
Case selection
We randomly selected 61 patients with breast cancer from the Department of oncology,people’s Hospital of Inner Mongolia Autonomous Region,from June 2019 to May 2020.One month after the operation (without radiotherapy,chemotherapy,and other adjuvant treatment),peripheral venous blood was taken from the patients and their lineal relatives (with no history of malignant tumor and the same ABO blood group as the patients).
CIK cell induction
Peripheral blood mononuclear cells (PBMCs) were obtained from the peripheral blood of patients with breast cancer and their lineal relatives by density gradient centrifugation using the human lymphocyte separation solution.We used RPMI1640 medium containing 10 %calf serum to culture the cells at 37 °C and 5% CO2in an incubator for 2 h;we collected non-adherent cells and placed them in a new culture flask.After adjusting the cell density to 1 × 106/mL,the cells were supplemented with IFN-γ (1000 U/mL),CD3 monoclonal antibody (50 μg/mL),IL-2 (300 U/mL),and IL-1 α (100 U/mL).Then,the cells were counted every 3 days and supplemented with a fresh medium containing 300 U/mL IL-2.
Tumor cell culture
SKBR-3 cells were cultured in an RPMI1640 medium containing 10 % calf serum at 37°C and 5 % CO2.Cells in the logarithmic growth phase were sampled for use in the experiment.
Immunophenotypic detection of CIK cells
We collected autologous and allogeneic CIK cells from patients with breast cancer on day 15 of culture and analyzed them by flow cytometry with direct immunofluorescence labeling.
Detection of secretory cytokines
We investigated the IFN-γ secretion levels of autologous and allogeneic CIK cells from patients with breast cancer on day 15 of culture using the ELISA double antibody sandwich method.
Cytotoxicity test
We used SKBR-3 cells in the logarithmic growth phase as target cells and autologous and allogeneic CIK cells as effector cells.The specific cytotoxicity was detected using the LDH release method.The effector and target cells were incubated in RPMI1640 medium containing 10 %FBS at 37 °C for 4 h.We detected the LDH release level of the cells using an ELISA kit and calculated the target cell lysis rate.
Statistical analysis
We used the SPSS 18.0 software to analyze the results.The results are expressed as the mean ± SD.We used thet-test to compare the different groups and consideredP<0.05 as indicative of statistical significance.
Results
CIK cell proliferation ability analysis
Fig.1 shows the proliferation rate comparison of the two CIK cell groups cultured on days 2,5,8,11,and 14.The two groups of CIK cells began to proliferate on culture days 3-4 and were in the active growth phase by days 6-7.The proliferation rate of the allogeneic CIK cells was significantly higher than that of the autologous CIK cells in patients with breast cancer.
CIK cell immunophenotype detection
On culture day 15,the proportion of allogeneic CD3+CD8+and CD3+CD56+double-positive CIK cells was significantly higher than that of the autologous CIK cells of the patients with breast cancer under the same conditions (Fig.2).
Detection of cytokines secreted by the CIK cells
Fig.3 shows the results of the ELISA,which detected the level of IFN-γ secreted by the CIK cells in the two groups.The level of IFN-γ secreted by the CIK cells (1× 106) in the allogeneic group on culture day 15 was significantly higher than that secreted by the CIK cells in the autologous group.
Detection of the antitumor activity of the CIK cells
The cytotoxicity of the two cell groups against human breast cancer SKBR-3 cells was detected by a nonradioactive 4-hour LDH release assay.The dissolution rates of target cells with different target-to-effector ratios are shown in Fig.4.The results showed that,with the increase in the effector-to-target ratio,the killing activity of the two effector cell groups also increased.At the same effector-to-target ratio,the killing activity of the allogeneic CIK cells was higher than that of the autologous CIK cells (P< 0.01).
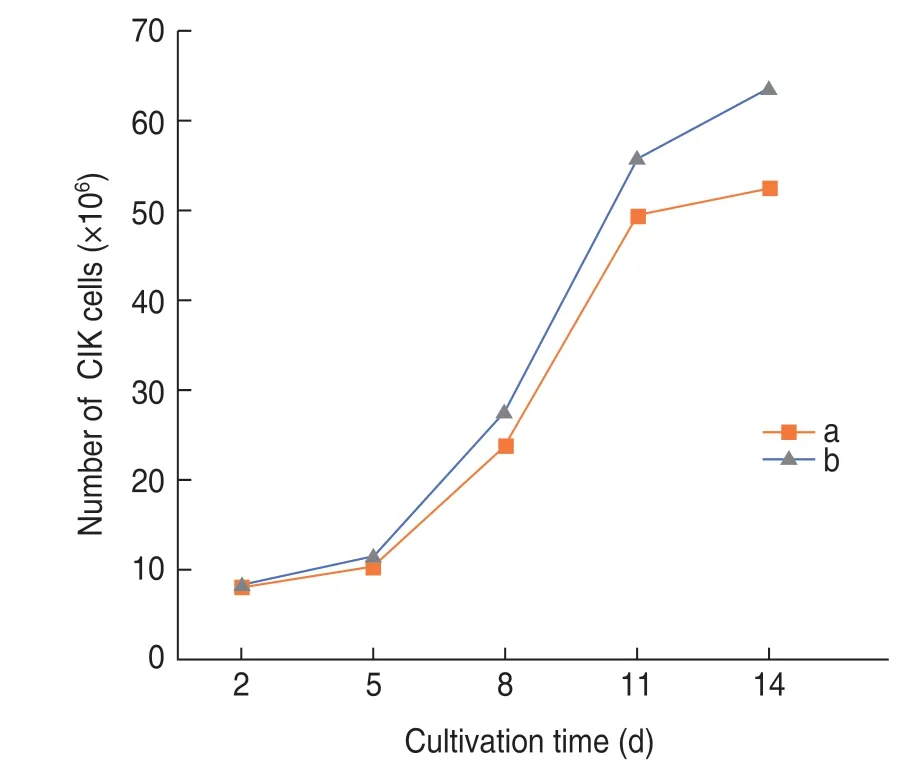
Fig.1 Analysis of CIK cell proliferation.Lines a and b represent the autologous CIK cells of patients with breast cancer and allogeneic CIK cells of their healthy lineal relatives,respectively
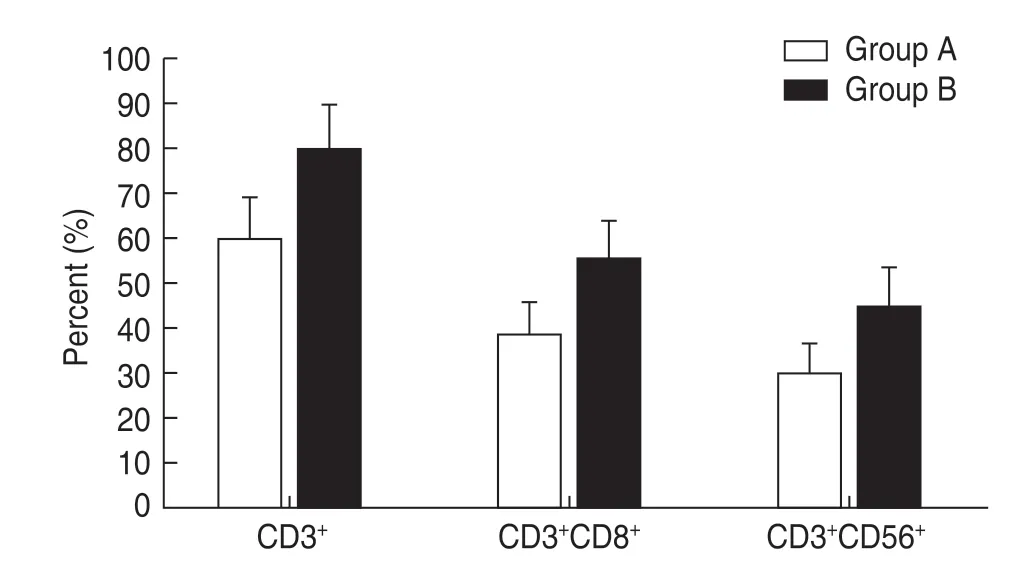
Fig.2 Immunophenotype detection of the two CIK cell groups.Groups A and B represent the autologous CIK cells of patients with breast cancer and allogeneic CIK cells of their healthy lineal relatives,respectively
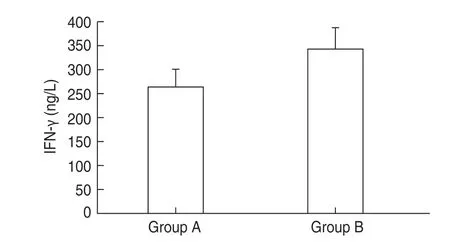
Fig.3 Detection of IFN-γ secreted by the two CIK cell groups.Groups A and B represent the autologous CIK cells of patients with breast cancer and allogeneic CIK cells of their healthy lineal relatives,respectively

Fig.4 The lysis rates of the two groups of CIK cells for SKBR-3 cells.Groups A and B represent the autologous CIK cells of patients with breast cancer and allogeneic CIK cells of their healthy lineal relatives,respectively
Discussion
Tumor biotherapy is considered to be the only way to cure cancer.As a new treatment approach after surgery,radiotherapy,and chemotherapy,tumor biotherapy is gradually being accepted by a majority of patients,due to its safety,effectiveness,and low level of side effects.It is widely used in the treatment of tumor patients both nationally and internationally,and has given good results.Adoptive cellular immunotherapy is the most common and effective approach for tumor biotherapy.It mainly enhances the anti-tumor effect of the immune system by stimulating cultured immune cellsin vitroto inhibit or eliminate tumors[1,5].Several national and international clinical studies have confirmed that adoptive cellular immunotherapy has obvious therapeutic effects on a variety of malignant tumors,including breast cancer;malignant tumors of the digestive,urinary,and hematological systems;and gynecological malignant tumors and malignant melanoma.Adoptive cell immunotherapy mainly uses immune cells,such as lymphokine-activated killer cells (LAK),tumorinfiltrating lymphocytes (TIL),and cytokine-induced killer cells (CIK),of which CIK cells are the most widely used[6-7].
The first CIK cell phase I clinical trial conducted was that by Schmidt wolfet al.The authors transfused autologous CIK cells back into 10 patients with malignant tumors,which confirmed the efficacy and safety of CIK cells for clinical treatment for the first time.Subsequently,due to the advantages of CIK cells and the progress of thein vitroinduction and amplification technology,CIK cells became widely used in the clinical treatment of a variety of malignant tumors.It is worth mentioning here,that,although early CIK cell research originated from the United States and Europe,clinical application of CIK cells in other countries is far less significant than that in China.At present,hundreds of scientific research institutions and hospitals in China have carried out CIK cell-related clinical research and treatment.The results of these scientific and medical efforts provide significant clinical data to further progress the CIK cell induction and treatment technology in the world,representing an important contribution[8-10].
The clinical application of CIK cells mainly includes the following aspects:(1) Elimination of small residual lesions in patients with a complete response and survival prolongation.(2) Combination with traditional tumor treatment methods (such as surgery,radiotherapy,and chemotherapy) to treat malignant tumors.(3) Use,alone,in patients with advanced malignant tumors who cannot tolerate other treatment options.CIK cells yield excellent results in terms of minimizing side effects.To date,no serious adverse reactions and death events related to CIK cell therapy have been reported in clinical application.Very few patients showed mild adverse reactions,such as fever or fatigue,most of which were relieved on their own,and only a few patients needed simple symptomatic treatment[11].
At present,CIK cells used in clinical treatment nationally and internationally are mostly induced using the autologous peripheral blood mononuclear cells of tumor patients.The reason for using this approach is that autologous CIK cells might recognize the surface markers of tumor cells and have strong tumor antigen activity.However,in recent years,certain researchers brought attention to the low level of immunity and poor activity of immune cells in tumor patients,which could affect the therapeutic effect of autologous CIK cells[12].In this study,we compared various activities (including proliferation,cytokine secretion,and anti-tumor effect)of autologous CIK cells and allogeneic CIK cells (induced by peripheral blood mononuclear cells from healthy lineal relatives) in 61 patients with breast cancer.The results showed that the proliferation ability of CIK cells in healthy adults was significantly higher than that of autologous CIK cells in breast cancer patients,and the ratio of CD3+CD8+and CD3+CD56+cells in healthy adults was significantly higher than that of autologous CIK cells in breast cancer patients (P< 0.05).At the same culture time-point,the level of IFN -γ secreted by allogeneic CIK cells was higher than that secreted by autologous CIK cells (P< 0.05).In vitro killing experiments confirmed that the anti-tumor activity of healthy human CIK cells against tumor cells was stronger than that of autologous CIK cells of tumor patients under the same effector-to-target ratio (P< 0.01),and this anti-tumor activity increased with the increase of the effector-to-target ratio.
Patients with malignant tumors often have impaired immune function,which affects the anti-tumor effect of autologous CIK cells.The breast cancer patients selected in this study had just finished surgery,without chemotherapy,radiotherapy,or other adjuvant therapies that might have caused myelosuppression,and the number of peripheral blood mononuclear cells in them was relatively high.The number and biological activity of autologous CIK cells induced in patients after chemotherapy and other treatments may be even lower.The CIK cells of healthy people have stronger antitumor activityin vitro,have a wide range of sources,and proliferate faster;thus,they can greatly shorten the patient’s waiting time for treatment while exerting anti-tumor effects.With the development of research on the isolation and purification of CIK cells and tumor antigens,adoptive immunotherapy using CIK cells will be more widely accepted and play an important role in the comprehensive treatment of malignant tumors.
Conflicts of interest
The authors indicated no potential conflicts of interest.
 Oncology and Translational Medicine2021年2期
Oncology and Translational Medicine2021年2期
- Oncology and Translational Medicine的其它文章
- A case report of iodine-125 seed placement during operation for the treatment of advanced gallbladder carcinoma with septic shock*
- Analysis of the adverse reactions of atezolizumab:A real-world study based on FAERS database
- Analyses of the clinical characteristics of 49 cases of malignancy with multiple bone lesions as the first manifestation
- Application of endoscopic nasobiliary cutting in the treatment of hilar cholangiocarcinoma
- KIF15 expression characteristics:Relevance toneo-adjuvant chemotherapy efficacy in breast cancer*
- Differentially expressed genes analysis and target genes prediction of miR-22 in breast cancer*
